Abstract
Background
Shuntograms are performed when patients present with symptoms suggestive of, but inconclusive for, shunt malfunction, without confirmatory radiological evidence.
Methods
Shuntograms over the past 3.5 years were reviewed. Patient records were reviewed for revision in proximity to a negative (normal) study.
Results
One hundred and fifteen out of 149 tests were negative. Thirty-four surgeries (in 31 patients) occurred subsequent to a negative shuntogram. In 18 out of 34 revisions the shunt was functional: 13 surgeries were for overdrainage, 4 were for unrelated reasons with shunt function confirmed incidentally and 1 was an exploration for cognitive deterioration. In 16 cases (13 patients) the shunt was not functional: 12 had proximal catheter occlusion in which, on subsequent review, there was no ventricular reflux present and the remaining had distal malfunctions.
Conclusions
The false negative rate for shuntograms was 16 out of 115 (14%) with proximal occlusion most common. This estimate of the predictive value of a normal flow study may influence the decision to revise a shunt.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebrospinal fluid (CSF) diversion through ventriculoperitoneal, and less commonly ventriculoatrial shunts, plays an integral role in the management of pediatric hydrocephalus. A significant proportion of most modern pediatric neurosurgical practices consist of CSF shunting procedures [12]. Shunt failure remains inevitable during a patient's life, with 81% requiring revision at 12 years of follow-up [15]. In the early months (0–5) following shunt insertion certain clinical features have high predictive values for shunt failure regardless of the radiological findings. These include nausea/vomiting, irritability, bulging fontanel, and decreased level of consciousness [7]. Decreased level of consciousness and loss of developmental milestones alone are strongly predictive of shunt malfunction in those who are 9 months to 2 years post shunt insertion [7].
With radiological evidence of ventriculomegaly and/or shunt disconnection shunt malfunction is an easy diagnosis in the presence of symptoms and signs of raised intracranial pressure. However, a considerable proportion of patients presenting to emergency rooms with new onset headache and suspected shunt malfunction will have equivocal radiological findings. It has been estimated that approximately one third of patients presenting with shunt failure will not have corroborative head computer axial tomogram (CT) imaging [9, 20]. Some workers consider baseline CT scans to be of little value when patients present with symptoms of shunt malfunction [4].
The initial identification and subsequent differentiation of the slit ventricle syndrome (SVS) with high intracranial pressure (ICP) due to shunt obstruction from the syndrome of overdrainage and low ICP (LICPS) can be difficult both clinically and radiologically. ICP monitoring can help in this process [3, 14].
The injection of radionucleotide into the reservoir of a shunt ("shuntogram") has been recommended as an investigation of the patency of both the proximal and distal shunt catheters and the integrity of the valve mechanism assuming that the reservoir lies proximal to the shunt valve [1, 2, 19]. In our institution shuntograms are performed when patients present with symptoms suggestive of, but inconclusive for, shunt malfunction, without CT or shunt series evidence of malfunction. We set out to audit our experience with shuntograms in patients subsequently requiring surgery and to determine our own experience with it and its predictive value for normal shunt function. We used the endpoint of persistent clinical symptoms that led to surgical identification of shunt failure to determine the predictive value of the test.
Materials and methods
All shuntograms performed in St. Louis Children's Hospital were reviewed over a 3.5-year period between 1997 and 2001. Shuntograms performed on ventriculoperitoneal shunts, ventriculoatrial shunts and cystoperitoneal shunts were included. Virtually all patients had a PS Medical valve present with the reservoir integral to the valve housing. The procedure involved a member of the neurosurgical staff injecting an average of 0.5 ml of 99mTc-diethylenetriaminepentaacetic acid into the shunt reservoir proximal to the valve. Distal occlusion was variably performed due to a combination of patient factors and difficulty with palpation of the distal occluder site. Reflux to the ventricle and flow to the peritoneal cavity was monitored and determined if present. A 'negative' study referred to a functioning shunt determined by flow to the peritoneal cavity within 15 min and reflux into the ventricle. The nuclear medicine staff generally commented on whether gravity aided the flow of the tracer if progression was slow and the time it took for radionucleotide to first enter the peritoneal cavity.
The case notes and shuntograms of patients who had 'negative shuntograms' and who subsequently required surgery were reviewed. The following data were collected from the case notes: sex of patient and age at time of surgery, symptoms and signs prior to surgery, presence of arachnoid cyst or hydrocephalus requiring shunt placement, duration between shuntogram and operation, the time in minutes for radionucleotide to enter the abdomen, and intra-operative findings/surgical management. The shuntograms were reviewed for visibility of ventricular reflux and progression of radionucleotide along the peritoneal catheter to the abdomen.
Results
In total 333 shunt revisions were performed in this unit during this 3.5-year time period. One hundred and forty-nine shuntograms were performed; 34 were reported positive and 115 negative. Despite a negative (normal) study 34 surgeries were performed on 31 patients within 1–14 days of such a shuntogram. There were 22 boys and 9 girls in this group, with a mean age of 9.2 years. Twenty-seven had ventriculoperitoneal shunts, 1 had a ventriculoatrial shunt, and 3 had cystoperitoneal shunts. All patients had pre-shuntogram CT scans that were unchanged from before with decompressed ventricles or intracranial cysts.
All patients more than 3 years of age presented with recurrent headaches and occasional vomiting. Those less than 3 presented with irritability and lethargy.
Patients were divided into four groups based on surgical findings: those found at surgery to have a proximal catheter occlusion, those found to have a functioning shunt and whose valve was changed to either a programmable one or to one of a higher resistance (LICPS), those with a distal catheter malfunction, and 'other' groups.
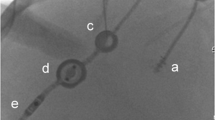
Twelve cases had proximal catheter occlusion. All of these cases showed no evidence of ventricular reflux when the shuntograms were reviewed (Fig. 1, Table 1). In only one of these cases was the absence of ventricular reflux commented upon, yet the shunt systems were declared patent in all cases. The mean shuntogram transit time in these cases was 8.6 min.
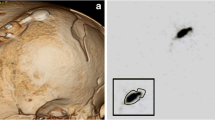
There were 13 LICPS cases in which the shuntogram revealed brisk flow to the peritoneal cavity with a 4.5-min mean transit time (Fig. 2). Sitting up aided progression of radionucleotide in all cases. Ventricular reflux was present when reviewed in 7 of these cases, yet it was remarked upon only once.
Four cases were of distal catheter malfunction. The mean transit time in these 4 cases was 12 min. Sitting up also aided the flow of radionucleotide but not quite to the same extent as in the overdrainage cases (Fig. 3, Table 1).
Five cases were revised for 'other' reasons such as an impending mastoid operation requiring re-routing of the shunt.
The mean time from shuntography to surgery is shown in Table 2. This shows almost similar values for the overdrainage cases and the proximal occlusion cases: 10 and 9 days respectively.
All cases improved following revision. Although there is a theoretical risk of infection when shuntography is carried out, there were no such complications in our series. The valve was not aspirated and no rapid deterioration occurred following shuntogram.
Discussion
Difficulties are universally experienced assessing the patency of a shunt in a child with headaches presenting to the emergency room [19]. It can be difficult to distinguish a viral illness or migraine from shunt malfunction. As simple palpation of the shunt flushing device is not accurate investigations are needed to establish a diagnosis [13]. Some workers emphasize the role of CT imaging [10], while others, in the presence of normal imaging, favor the measurement of the pressure in a separate reservoir [17]. In 1966 Di Chiro and Grove injected radionucleotide into a shunt system directly for the first time and imaged the radioactivity along its path [5]. This method has gained in popularity ever since [6, 8].
Some workers have emphasized the importance of ventricular reflux as a pre-requisite feature in declaring a shuntogram to be normal [11, 18, 19]. A false negative rate for shuntography of 14% (3 out of 22) has been reported with proximal catheter malfunction present in 2 out of 3 cases [19]. Our series differed in that there were no cases of proximal catheter occlusion found at surgery in which ventricular reflux was found on pre-operative shuntography. The absence of ventricular reflux in the 12 cases of proximal catheter occlusion is understandable, but that was largely underreported in this series. As occlusion of the distal outlet of the valve can be quite difficult in young, awake children, and as it was variably performed, it was not known whether the lack of ventricular reflux was real or due to technical error. It was assumed to be the latter.
There was an absence of ventricular reflux in 47% of the LICPS cases. Again this was probably influenced by the PS Medical reservoir being integral to the valve housing. A separate reservoir proximal to the valve may have produced greater reflux in the overdrainage cases. An overly stringent policy on the presence of ventricular reflux indicating normality would certainly increase the false positive rate and could lead to unnecessary revisions. Many of these cases represented partial occlusion of a sub-optimally functioning shunt. Thus, even retrograde flow would not necessarily have excluded partial proximal malfunction.
Slit ventricle syndrome has been classified into acute, subacute and chronic forms [16]. Given that the patients in the proximally occluded group were not that unwell, had all had decompressed ventricles on CT scan, and symptoms over a period of days to weeks, it is reasonable to suggest that this proximally occluded group is a chronic subgroup of slit ventricle syndrome.
The rapid transit time in overdrainage cases together with rapid radionucleotide flow when the patient sits up seem to indicate features of low intracranial pressure syndrome on shuntography. Shuntography can therefore differentiate between SVS and LICPS by the absence of ventricular reflux in SVS and the rapid transit time to the peritoneal cavity in LICPS. An anatomically normal shuntogram, with ventricular reflux and peritoneal flow as in the LICPS cases, does not offer total re-assurance as to the patient's shunt being optimal, but it may obviate the need for ICP monitoring to distinguish one syndrome from the other.
It is interesting to note that radionucleotide can enter the peritoneal cavity even in the presence of a malfunctioning distal system. Our experience is that distal malfunctions may produce spontaneous passage of tracer and relatively normal transit times. At surgery in these cases, externalization of the distal catheter revealed suboptimal or non-existent CSF flow. The reason why radionucleotide and CSF flow seem to differ is difficult to explain, but this would suggest that gravity aids radionucleotide in overcoming a partial distal malfunction. It is also possible that the upper limit of normal for radionucleotide to reach the abdomen and the study to be declared normal, i.e., 15 min, is excessive in cases of partial distal malfunctions.
If all the cases in our series, which were reported as being negative and which were found to be malfunctioning at surgery (12 proximally and 4 distally occluded cases) are included, then our false negative rate is also 14%. However, if the 12 proximally occluded cases, in which on retrospect there was no ventricular reflux on shuntography, are excluded, the false negative rate is lowered to 3.4%. The false positive rate was 0% as all abnormal reported shuntograms were found to have an improperly functioning shunt at surgery. Eighty percent of shunt revision cases did not have a preoperative shuntogram.
Conclusions
Despite several publications on the subject there still remains a great deal of confusion amongst all involved in radionucleotide shuntography as to what constitutes a normal shuntogram [11, 18, 19]. We re-iterate the value of requiring ventricular reflux to be present for a shuntogram to be labeled as being normal (Fig. 4). We emphasize the role of shuntography in the diagnosis of overdrainage cases and highlight its role in the differentiation of LICPS from subacute and chronic forms of SVS in which the proximal catheter is occluded. By diligent assessment of ventricular reflux the false negative rate of 14% can be lowered to 3.4% at the risk of increasing the false positive rate. This study highlights the sine qua non of the necessity for shunt revision as being the clinical assessment of the patient.
Shuntogram in a patient with hydrocephalus treated with a ventriculoperitoneal shunt (medium pressure PS Medical valve), showing radionucleotide in the reservoir of the shunt and reflux into the ventricle. He developed a low intracranial pressure syndrome. The valve was revised to a low pressure PS Medical valve attached distally in series to a Codman-Medos programmable valve with resolution of symptoms
References
Bartynski WS, Valliappan S, Uselman JH, Spearman MP (2000) The adult radiographic shuntogram. Am J Neuroradiol 21:721–726
Brendel AJ, Wynchank S, Castel JP, Barat JL, Leccia F, Ducassou D (1983) Cerebrospinal shunt flow in adults: radionuclide quantification with emphasis on patient position. Radiology 149:815–818
Bruce DA, Weprin B (2001) The slit ventricle syndrome. Neurosurg Clin N Am 36:709–717
Cantrell P, Fraser F, Pilling D, Carty H (1993) The value of baseline CT head scans in the assessment of shunt complication in hydrocephalus. Pediatr Radiol 23:485–486
Di Chiro G, Grove AS (1966) Evaluation of surgical and spontaneous cerebrospinal fluid shunts by isotope scanning. J Neurosurg 24:743–748
French BN, Swanson, M (1981) Radionuclide-imaging shuntography for the evaluation of shunt patency. Surg Neurol 16:173–182
Garton HJ, Kestle JR, Drake JM (2001) Predicting shunt failure on the basis of clinical symptoms and signs in children. J Neurosurg 94:202–210
Graham P, Howman-Giles R, Johnson I, Besser M (1982) Evaluation of CSF shunt patency by means of technetium-99m DTPA. J Neurosurg 57:262–266
Iskandar BJ, McLaughlin C, Mapstone TB, Grabb PA, Oakes WJ (1998) Pitfalls in the diagnosis of ventricular shunt dysfunction: radiology reports and ventricular size. Pediatrics 101:1031–1036
Kan L, Nagelberg J, Maytal J (2000) Headaches in a paediatric emergency department: etiology, imaging and treatment. Headache 40:25–29
May CH, Aurisch R, Kornrumpf D, Vogel S (1999) Evaluation of shunt function in hydrocephalic patients with the radionuclide 99mTc-pertechnetate. Childs Nerv Syst 15:239–245
McComb JG (1990) Techniques for CSF diversion. Concepts Neurosurg 3:47–64
Osaka K, Yamasaki S, Hirayama A, Sato N, Ohi Y, Matsumoto S (1977) Correlation of the response of the flushing device to compression with the clinical picture in the evaluation of the functional status of the shunting system. Childs Brain 3:25–30
Pudenz RH, Foltz EL (1991) Hydrocephalus: overdrainage by ventricular shunts. A review and recommendations. Surg Neurol 35:200–212
Sainte-Rose C, Piatt JH, Renier D, Pierre-Kahn A, Hirsch JF, Hoffman HJ, Humphreys RP, Hendrick EB (1991) Mechanical complications in shunts. Pediatr Neurosurg 17:2–9
Serlo W, Heikkinen E, Saukkonen AL, Wendt LV (1985) Classification and management of the slit ventricle syndrome. Childs Nerv Syst 1:194–199
Sood S, Canady AI, Ham SD (2000) Evaluation of shunt malfunction using shunt site reservoir. Paediatr Neurosurg 32:180–186
Uvebrant P, Sixt R, Bjure J, Roos A (1992) Evaluation of cerebrospinal fluid shunt function in hydrocephalic children using99mTc-DTPA. Childs Nerv Syst 8:76–80
Vernet O, Farmer JP, Lambert R, Montes JL (1996) Radionuclide shuntogram: adjunct to manage hydrocephalic patients. J Nucl Med 37:406–410
Watkins L, Hayward R, Andar U, Harkness W (1994) The diagnosis of blocked cerebrospinal fluid shunts: a prospective study of referral to a paediatric neurosurgical unit. Childs Nerv Syst 10:87–90
Acknowledgements
Dr. O'Brien is grateful for financial assistance received from the Royal College of Surgeons in Ireland, which enabled him to travel to St. Louis Children's Hospital. J.G.O. is supported by NIH grant NS41272.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O'Brien, D.F., Taylor, M., Park, T.S. et al. A critical analysis of 'normal' radionucleotide shuntograms in patients subsequently requiring surgery. Childs Nerv Syst 19, 337–341 (2003). https://doi.org/10.1007/s00381-003-0752-y
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-003-0752-y