Abstract
Diabetes mellitus (DM) is a substantial risk factor in developing coronary artery disease (CAD), coronary chronic total occlusion (CTO) lesions are discovering 10–35% in patients who underwent coronary angiography. This study compares the long-term clinical outcomes of two treatment strategies, percutaneous coronary intervention (PCI) with complete recanalization versus medication therapy (MT) with CTO lesion in DM patients with CTO. This study is a single-center, prospective, all-comer registry designed to reflect “real world” practice since 2004. Of a total of 4909 consecutive patients were diagnosed with significant CAD by coronary angiography (CAG). A total of 372 patients has DM and CTO lesions. Patients were divided into the PCI group (n = 184) and the MT group (n = 179). The primary endpoint, defined as the composite of death or myocardial infarction (MI), was compared between the two groups up to 5 years. In addition, inverse probability weighting (IPTW) analysis, derived from the logistic regression model, was performed to adjust for potential confounders. Compared to the MT group, the PCI group was associated with a significantly reduced incidence of the primary endpoint before [hazard ratio; HR 0.267, 95% confidence interval (CI) 0.116–0.614] and after (HR 0.142, 95% CI 0.032–0.629) adjusting confounding factors by IPTW. Complete revascularization by CTO-PCI with MT in DM patients should be the preferred treatment strategy compared with the MT alone strategy since it reduces the composite of death or MI up to 5 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many studies reported that successful revascularization for chronic total occlusion (CTO) lesions could benefit long-term survival, including improved left ventricular (LV) function, symptom relief, and quality of life [1,2,3,4]. However, a percutaneous coronary intervention (PCI) of CTO lesions remains one of the most challenging procedural techniques. These coronary CTO lesions were discovered 10 to 35% in patients who underwent coronary angiography [5,6,7]. Also, an earlier study showed that CTO-PCI was failed a total of 20 to 35% [8]. In addition, the prevalence of diabetes mellitus (DM) showed 10 to 35% of all CTO patients [9,10,11]. These DM patients have a higher risk of cardiovascular events and death than those without DM [12]; furthermore, stenting for coronary artery lesions in DM patients is known to be associated with significantly higher in-stent restenosis (ISR) rates of 32–66% [13]. In addition, after coronary stenting, ISR in DM patients remains a challenging clinical problem [13]. Therefore, medication therapy (MT) could be essential for DM patients with CTO lesions to reduce PCI recurrence or prevent de novo progression. Recently, Korean data reported that patients with CTO-PCI combined with MT experienced significantly reduced long-term risk of death or myocardial infarction (MI) and improved LV function compared with MT alone [14,15,16,17]. Based on these results, patients with CTO and well-developed collateral circulation may be recommended for revascularization as an initial treatment [15, 18]. However, the long-term prognostic effect of CTO-PCI on cardiovascular events in CTO patients with DM remains uncertain as compared with MT alone. Therefore, this study aims to compare the long-term clinical outcomes of two different treatment strategies: PCI with complete recanalization versus MT with CTO lesion in DM patients with CTO.
Methods
Study design
The study data were obtained from Korea University Guro Hospital (KUGH), Seoul, South Korea [15, 17]. This trial is a single-center, prospective, all-comer registry designed to reflect “real world” practice since 2004. Data were collected by trained study coordinators using a standardized case report form. The participants or their legal guardians received a literal and verbal explanation of the study procedures before the study. They also gave the written consent to research investigators to participate in the study. The Medical Device Institutional Review Board of KUGH approved this study protocol. The authors of this manuscript have certified that the information contained herein is true and correct, as reflected in the Medical Device Institutional Review Board (#MD07014).
Study population
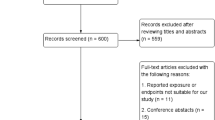
A total of 4909 consecutive patients were diagnosed with significant coronary artery disease (CAD, defined by ≥ 70% coronary artery stenosis) by coronary angiography (CAG). In this study, 17.1% (840/4909) of patients with CAD had a CTO lesion, of which 44% (372/840) had type 2 DM. In patients with CTO and DM, they were stable angina of 33.1%, unstable angina of 45.7%, and MI of 22.2%. Among these, 214 patients were allocated into the PCI and MT (the PCI group), and 149 patients were allocated into the MT-only group (the MT group). In the PCI group, the CTO procedure was attempted but failed in 10.7% (23/214) of the patients, while 3.2% (7/214) received a partially successful PCI, where CTO lesions remained in patients with multi-vessel CTO. These patients survived at discharge and were re-allocated into the MT group. Finally, the study population was divided into the PCI group with 184 patients and the MT group with 179 patients (Fig. 1). The exclusion criteria of this study were one or more of the followings: (1) no type 2 DM; (2) CTO located in a small vessel (reference vessel diameter ≤ 2.5 mm) and the side branch vessels, including the acute marginal, diagonal, septal, and obtuse marginal arteries; or (3) history of coronary artery bypass graft (CABG) surgery for CTO.
PCI procedure and medical treatments
In the non-CTO lesions, PCI was preferentially performed for patients with symptoms expected to improve their symptoms. However, regarding the CTO lesions, physicians selected treatment options including MT and/or the PCI procedure for CTO lesions, because PCI for CTO lesions is well-known for its relatively low success rate and higher complication rate, while CTO treatment efficacy remains controversial. CTO-PCI has performed a general standard PCI technique by an elective PCI [19]. PCI was performed through either the femoral or the radial artery after administration of unfractionated heparin (70–100 U/kg). Before PCI, all patients received aspirin (200–300 mg) and clopidogrel (300–600 mg). Drug-eluting stents were deployed after prior balloon angioplasty, and anticoagulation therapy during PCI was left to the individual operator's discretion. A successful PCI was defined as achieving residual angiographic stenosis of less than 10% without major adverse cardiac events (MACE) in the presence of thrombolysis in myocardial infarction (TIMI) blood flow grade 3. The patients maintained dual antiplatelet therapy for at least 1 year. In addition, patients received cardiovascular beneficial medications during the in-hospital period, including beta-blockers, renin–angiotensin–aldosterone system receptor inhibitors, calcium channel blockers, and statins. After discharge, the patients were encouraged to maintain the same medicines they received in the hospital.
Study definitions
CTO has defined a total occlusion in the main coronary artery (TIMI grade 0) for longer than 3 months. The main coronary artery has defined an above 2.5 mm of the reference vessel diameter, and CTO has located in the main vessel at the left main (LM), left anterior descending (LAD), left circumflex (LCX), right coronary (RCA), and ramus arteries. The LV ejection fraction (EF) was assessed by echocardiography. Preserved LV function has defined above EF ≥ 50% and reduced LV function below EF < 50%. Criteria for DM is above one of the following: (1) patients diagnosed with DM prior or who had treatments, including diabetic medications, diet, and exercise. (2) They received a fasting blood glucose test and these records above 7 mmol/L at least two times from doctors. (3) Patients have a use hypoglycemic therapy for diabetic control. MACE has defined a composite of all-cause death, MI, and revascularization, including PCI and CABG. Target lesion revascularization (TLR) has defined repeat revascularization at the same CTO lesion. Also, a target vessel revascularization (TVR) has defined repeat revascularization at the same CTO artery. Non-TVR has defined revascularization for the non-CTO lesion. It means repeat revascularization at the non-CTO lesions or performed revascularization at De-novo lesions.
Statistical analysis
The differences between the two groups were evaluated using the unpaired t test or Mann–Whitney rank test for continuous variables. These are shown as means ± standard deviations. Also, the discrete variables are shown as counts and percentages and analyzed with the χ2 or Fisher’s exact test. Inverse probability weighting (IPTW) analysis, derived from the logistic regression model, was performed to adjust for potential confounders.
The Kaplan–Meier analysis and the log-rank test estimated the various clinical outcomes for a 5-year follow-up between the groups. Proportional hazards models assessed the PCI group's hazard ratio (HR) compared with the MT group among the IPTW weighted population. The statistical significance of a two-tailed test has considered below P value ≤ 0.05 for all analyses. All statistical analysis was performed using SPSS (version 20.0, SPSS-PC, Inc., Chicago, Illinois).
Study outcomes
The primary endpoint is defined as the composite of death (regardless of cardiac origin) or MI. Secondary endpoints were death, MI, revascularization including PCI or CABG, and MACE. Follow-up on the clinical data of all enrolled patients was possible through face-to-face interviews at regular outpatient clinic visits, medical chart reviews, and telephone calls.
Results
In the initially allocated PCI group, 85.9% (184/214) of patients had a successful PCI for CTO. The remaining 14.1% (30/214), who underwent an attempted CTO procedure that either failed (23 patients) or had remaining CTO lesions (7 patients), were moved to the MT group. The resulting 179 patients were enrolled in the MT group, finally. Among these, 83.2% (149/179) had a multi-vessel disease, and 53.1% (95/179) underwent a successful PCI for non-CTO lesions.
The baseline clinical, angiographic, and procedural characteristics are shown in Tables 1 and 2. The PCI group had more stable angina (42.9% vs. 22.9%), old MI (19.6% vs. 7.8%) and a preserved LV ejection fraction (51.2% vs. 47.2%); conversely, the MT group had more unstable angina (55.3% vs. 36.4%), multi-vessel disease (83.2% vs. 58.2%), and a more well-developed collateral artery (grade III or IV, 82.1% vs. 70.1%). Compared to the PCI group, the MT group had more disease arteries (2.4 ± 0.8 vs. 1.8 ± 0.8), including LCX, RCA, and LM. CTO lesions had more commonly located at LAD in the PCI group (37.0% vs. 25.1%) but more frequently at LCX (73.2% vs. 48.4%) or RCA (57.5 vs. 45.1%) in the MT group. The PCI group received more calcium channel blockers of the non-dihydropyridine class (34.2% vs. 23.5%), statins (90.2% vs. 70.4%) than the MT group at discharge.
Table 3 shows the various clinical outcomes in up to 5-year follow-up by Kaplan–Meier survival analysis and log-rank test. The primary endpoint occurred more in the MT group (14.5%) than in the PCI group (3.8%), as did all-cause death (10.6% vs. 3.3%). However, as a secondary endpoint, TVR occurred more in the PCI group than in the MT group (11.4% vs. 5.6%).
To adjust for confounding factors, IPTW analysis was used. After IPTW, the baseline clinical and angiographic characteristics were well-balanced between the two groups except that the PCI group had more old MI than the MT group (20.3% vs. 11.3%) [Table 1]. The primary endpoint still occurred more in the MT group (11.9%) than in the PCI group (2.6%), as did all-cause death (8.8% vs. 2.3%) and MI (4.7% vs. 1.5%). Interestingly, non-TVR had lower in the PCI group (9.9%) than in the MT group (18.8%) after adjusting potential confounders by IPTW.
The MT group included 30 patients who underwent an attempted CTO procedure that either failed or had remaining CTO lesions (as the failed CTO-PCI group). In the primary endpoint, the PCI group showed better clinical outcomes when compared to both the MT-only group and the failed CTO-PCI group before (3.8% vs. 14.7% vs. 13.0%, respectively, P = 0.002) and after IPTW (2.6% vs. 11.4% vs. 14.5%, respectively, P < 0.001) (Fig. 2).
Subgroup analyses were performed to evaluate the impact of successful CTO-PCI on the primary endpoint using Cox-proportional hazards ratio analysis (Fig. 3). A successful CTO-PCI resulted in better clinical outcomes in various subgroups with DM patients, including elderly patients greater than 65 years old [HR 2.276, 95% confidence interval (CI) 0.090–0.841, P = 0.024], patients without prior MI (HR: 0.245, 95% CI 0.070–0.859, P = 0.028), patients with > 50% preserved LV EF (HR 0.146, 95% CI 0.027–0.771, P = 0.023), non-smokers (HR 0.198, 95% CI 0.048–0.807, P = 0.024), patients with multi-vessel disease (HR 0.151, 95% CI 0.032–0.713, P = 0.017), and patients with CTO at non-LAD arteries (HR 0.130, 95% CI 0.027–0.616, P = 0.010).
Subgroups analysis of diabetes, the impact of the percutaneous coronary intervention (PCI) on death or myocardial infarction compared to the medication therapy (MT) up to the 5-year follow-up by Cox-proportional hazard ratio analysis adjusted using IPTW score. LV left ventricular, CTO chronic total occlusion, LAD left anterior descending
Discussion
Our study confirmed the benefits of a successful CTO-PCI in DM and CTO patients. The main findings are as follows: (1) compared to the MT group, the PCI group was associated with significantly reduced incidence of the primary endpoint, composite of death, or MI at 5-year follow-up before (HR 0.267, 95% CI 0.116–0.614) and after (HR 0.142, 95% CI 0.032–0.629) adjusting for confounding factors. (2) A successful complete CTO-PCI was more beneficial to the primary endpoint in the following subgroups: the elderly (> 65 years); patients with preserved LV ejection fraction (≥ 50%), or CTO of non-LAD arteries; non-smokers; and patients with multi-vessel disease or without a history of MI.
DM is a substantial risk factor in the development of CAD and demonstrates a three-fold increase in cardiovascular morbidity and mortality [19]. Bulugahapitiya et al. reviewed 13 studies comprising 45,108 patients, with a follow-up ranging from 5 to 25 years by meta-analysis [20]. DM patients had a 43% higher risk of developing coronary heart disease events than patients without DM. The pathophysiology of vascular disease in DM involves abnormalities in the endothelial, vascular smooth muscle cell, and platelet function [21]. Thus, optimal medication therapy may be one of the important treatment strategies for DM patients with CTO lesions. Also, the systematic review of a previous study has shown that a complete PCI could improve the long-term clinical outcomes of DM patients with CTO lesions [22]. From the bypass angioplasty revascularization investigation 2 diabetes trial (BARI2D trial), patients underwent either revascularization with intensive medical therapy (IMT) or IMT alone, according to the presence of CTO in DM patients. The study results have shown that a CTO lesion might not increase mortality risk if patients treated with revascularization [23]. In contrast, a randomized trial showed no significant difference in the incidence of death and major cardiovascular events between CAD patients with DM undergoing prompt revascularization and those undergoing medical therapy [12]. Importantly, in CAD patients, the presence of a CTO has a major impact on clinical management and is a strong predictor against recommending PCI, with a preference for MT or CABG [22, 24].
Our study results showed the benefits of a successful CTO-PCI in DM patients. After adjustment for baseline confounders by IPTW, successful CTO-PCI reduced the primary endpoint risk (HR 0.190, 95% CI 0.090–0.400), including all-cause death (HR 0.697, 95% CI 0.493–0.985) up to 5 years follow-up. In particular, CTO-PCI was effective to the primary endpoint in the following subgroups of DM patients, including elderly (> 65 years), preserved LV ejection fraction (≥ 50%), CTO of non-LAD arteries, non-smokers, multi-vessel disease, and patients without a prior MI. Of particular interest is that the non-TVR had significantly lower occurred in the PCI group (HR 0.471, 95% CI 0.303–0.733) than in the MT group. Base on our results, we carefully assumed that CTO-PCI might prevent further coronary events via a reduced burden of non-CTO arteries in DM patients. This is because a myocardium territory on the CTO artery has blood supply from self or other coronary arteries via collateral arteries. As shown in our result, DM-CTO patients had a multi-vessel disease above minimum half. Therefore, successful CTO-PCI could reduce the functional burden of non-CTO arteries; also, if those who have further coronary events, treated CTO artery may support the event artery functionally.
In the present study, the MT group included patients who underwent an attempted CTO procedure that either failed or had remaining CTO lesions. As shown in Fig. 2, the PCI group showed a better result in the primary endpoint, as compared to both the MT-only group and the failed CTO-PCI group. Notably, the failed CTO-PCI group was not different from the MT-only group regarding the primary endpoint. The poor prognosis of the failed CTO-PCI group was entirely predictable. However, if the long-term outcome of a failed CTO-PCI survivor is similar to that of the MT-only group, CTO-PCI might be a good option in DM patients with CTO.
Another interesting, result of our study is that in the MT group, the patients in the crude population of 5.6% and the IPTW cohort of 11.0% received revascularization for CTO lesions finally during the follow-up period. It means that these patients are continuously suffering ischemic symptoms including chest pain or dyspnea despite the medication therapy, and further if their doctor had determined that CTO-PCI could help to improve patient’s clinical symptoms. In the IPTW cohort during follow-up, the occurrence of TVR for CTO lesions was no different between the PCI group and the MT group (13.1% vs. 11.0%, P = 0.407). Therefore, in the MT group, persistent clinical symptoms remained a problem.
CTO-PCI is a technically challenging procedure in the cardiovascular intervention field, and procedural success rates are still limited [25]. However, developments in equipment and techniques have led to the achievement of higher rates of success and lower rates of complications [26, 27], which shows as successful guidewires crossing CTO lesions within 30 min [28]. In the present study, 86.0% of patients (184/214) received complete CTO-PCI, and 3.2% of patients (7/214) partially underwent CTO-PCI. Operators seemed to prefer CTO-PCI in patients with stable angina or preserved LV function. The PCI group had more patients with stable angina and preserved LV function. However, the MT group had more patients with unstable angina, multi-vessel disease, and a well-developed collateral artery. These patients' conditions may affect the choice of PCI or medication treatment as the CTO's treatment strategy, but the procedural success rate and clinical outcomes of CTO-PCI also play a role in the decision [11, 17]. Our previous study reported that the elderly, patients with multi-vessel disease, a history of CABG, a retrograde approach to CTO, and lack of expert operator are related to procedural failure for CTO [11].
There are some limitations in this study. First, the present study was analyzed retrospectively, and an IPTW analysis was performed to minimize the confounding factors that might have influenced the results. Second, according to the clinician's discretion, all participants received adequate treatment, including PCI in non-CTO lesions. However, it is likely that the remaining non-CTO lesions in the MT group are reflected in the study results. For example, in the MT group, a total of 83.2% (149/179) had a multi-vessel disease, and 53.1% (95/179) received PCI treatment. Finally, the KUGH-PCI registry consisted of an all-comer prospective design since 2004. Thus, we could not adjust for all limiting factors not identified through medical records or collected through telephone calls despite data quality control.
In conclusion, our study results showed a complete PCI with IMT could improve the long-term clinical outcomes than patients who received IMT alone in DM patients with CTO lesions. Successful CTO-PCI is associated with reduced risk of the primary endpoint, composite of all-cause death, or MI up to a 5-year clinical follow-up, compared with MT alone strategy in patients with DM. However, these results are from an observational study, and therefore, a well-designed, large-scale randomized trial is needed to confirm these findings.
Data availability
All data can be checked by sending an email to correspondence.
Abbreviations
- CABG:
-
Coronary artery bypass graft
- CAD:
-
Coronary artery disease
- CAG:
-
Coronary angiography
- CI:
-
Confidence interval
- CTO:
-
Chronic total occlusion
- DM:
-
Diabetes mellitus
- EF:
-
Ejection fraction
- HR:
-
Hazard ratio
- IPTW:
-
Inverse probability weighting
- ISR:
-
In-stent restenosis
- KUGH:
-
Korea University Guro Hospital
- LAD:
-
Left anterior descending
- LCX:
-
Left circumflex
- LM:
-
Left main
- LV:
-
Left ventricular
- MACE:
-
Major adverse cardiac events
- MI:
-
Myocardial infarction
- MT:
-
Medication therapy
- PCI:
-
Percutaneous coronary intervention
- RCA:
-
Right coronary artery
- TIMI:
-
Thrombolysis in myocardial infarction
- TLR:
-
Target lesion revascularization
- TVR:
-
Target vessel revascularization
References
Grantham JA, Marso SP, Spertus J, House J, Holmes DR Jr, Rutherford BD (2009) Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv 2(6):479–486
Hoye A, van Domburg RT, Sonnenschein K, Serruys PW (2005) Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992–2002. Eur Heart J 26(24):2630–2636
Suero JA, Marso SP, Jones PG, Laster SB, Huber KC, Giorgi LV, Johnson WL, Rutherford BD (2001) Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol 38(2):409–414
Valenti R, Migliorini A, Signorini U, Vergara R, Parodi G, Carrabba N, Cerisano G, Antoniucci D (2008) Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J 29(19):2336–2342
Kahn JK (1993) Angiographic suitability for catheter revascularization of total coronary occlusions in patients from a community hospital setting. Am Heart J 126(3 Pt 1):561–564
Puma JA, Sketch MH Jr, Tcheng JE, Harrington RA, Phillips HR, Stack RS, Califf RM (1995) Percutaneous revascularization of chronic coronary occlusions: an overview. J Am Coll Cardiol 26(1):1–11
Ruygrok PN, De Jaegere PP, Verploegh JJ, Van Domburg RT, De Feyter PJ (1995) Immediate outcome following coronary angioplasty. A contemporary single centre audit. Eur Heart J 16 Suppl L:24–29
Hwang JW, Yang JH, Choi SH, Hwang JK, Jang WJ, Hahn JY, Song YB, Choi JH, Lee SH, Gwon HC (2016) Optimal medical therapy may be a better initial strategy in patients with chronic total occlusion of a single coronary artery. Int J Cardiol 210:56–62
Gray WA, Feiring A, Cioppi M, Hibbard R, Gray B, Khatib Y, Jessup D, Bachinsky W, Rivera E, Tauth J, Patarca R, Massaro J, Stoll HP, Jaff MR, Investigators SS (2015) S.M.A.R.T. self-expanding nitinol stent for the treatment of atherosclerotic lesions in the superficial femoral artery (STROLL): 1-year outcomes. J Vasc Interv Radiol 26(1):21–28
Olivari Z, Rubartelli P, Piscione F, Ettori F, Fontanelli A, Salemme L, Giachero C, Di Mario C, Gabrielli G, Spedicato L, Bedogni F, Investigators T-G (2003) Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE). J Am Coll Cardiol 41(10):1672–1678
Rha SW, Choi BG, Choi SY, Choi CU, Gwon HC, Chae IH, Kim HS, Park HS, Lee SH, Kim MH, Hur SH, Jang Y, Registry KC (2020) Multicenter experience with percutaneous coronary intervention for chronic total occlusion in Korean population: analysis of the Korean nationwide multicenter chronic total occlusion registry. Coron Artery Dis 31(4):319–326
Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, MacGregor JM, Orchard TJ, Chaitman BR, Genuth SM, Goldberg SH, Hlatky MA, Jones TL, Molitch ME, Nesto RW, Sako EY, Sobel BE (2009) A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 360(24):2503–2515
Choi D, Kim SK, Choi SH, Ko YG, Ahn CW, Jang Y, Lim SK, Lee HC, Cha BS (2004) Preventative effects of rosiglitazone on restenosis after coronary stent implantation in patients with type 2 diabetes. Diabetes Care 27(11):2654–2660
Choi JY, Choi BG, Rha SW, Mashaly A, Abdelshafi K, Choi CU, Yu CW, Gwon HC, Chae IH, Kim HS, Sik Park H, Lee SH, Kim MH, Hur SH, Jang Y (2020) One-year clinical outcomes of coronary chronic total occlusion intervention in patients with acute coronary syndrome versus stable angina: from the Korean chronic total occlusion registry. Coron Artery Dis 31(5):430–437
Choi SY, Choi BG, Rha SW, Baek MJ, Ryu YG, Park Y, Byun JK, Shim M, Li H, Mashaly A, Jang WY, Kim W, Choi JY, Park EJ, Na JO, Choi CU, Lim HE, Kim EJ, Park CG, Seo HS, Oh DJ (2017) Percutaneous Coronary Intervention Versus Optimal Medical Therapy for Chronic Total Coronary Occlusion With Well-Developed Collaterals. J Am Heart Assoc 6(9)
Park JY, Choi BG, Rha SW, Kang TS, Choi CU, Yu CW, Gwon HC, Chae IH, Kim HS, Park HS, Lee SH, Kim MH, Hur SH, Jang Y (2018) Chronic total occlusion intervention of the non-infarct-related artery in acute myocardial infarction patients: the Korean multicenter chronic total occlusion registry. Coron Artery Dis 29(6):495–501
Rha SW, Choi BG, Baek MJ, Ryu YG, Li H, Choi SY, Byun JK, Mashaly A, Park Y, Jang WY, Kim W, Choi JY, Park EJ, Na JO, Choi CU, Lim HE, Kim EJ, Park CG, Seo HS, Oh DJ (2018) Five-year outcomes of successful percutaneous coronary intervention with drug-eluting stents versus medical therapy for chronic total occlusions. Yonsei Med J 59(5):602–610
Jang WJ, Yang JH, Choi SH, Song YB, Hahn JY, Choi JH, Kim WS, Lee YT, Gwon HC (2015) Long-term survival benefit of revascularization compared with medical therapy in patients with coronary chronic total occlusion and well-developed collateral circulation. JACC Cardiovasc Interv 8(2):271–279
Voudris VA, Skoularigis JS, Dimitriou YK, Grapsa GN, Malakos JS, Pavlides GS, Manginas AN, Cokkinos DV (2004) Diabetes mellitus and unstable coronary artery disease: improved clinical outcome of coronary artery stenting in an era of glycoprotein IIb/IIIa inhibitors and lipid-lowering therapy. Coron Artery Dis 15(6):353–359
Bulugahapitiya U, Siyambalapitiya S, Sithole J, Idris I (2009) Is diabetes a coronary risk equivalent? Systematic review and meta-analysis Diabet Med 26(2):142–148
Paneni F, Beckman JA, Creager MA, Cosentino F (2013) Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J 34(31):2436–2443
Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR (2005) Effect of chronic total coronary occlusion on treatment strategy. Am J Cardiol 95(9):1088–1091
Damluji AA, Pomenti SF, Ramireddy A, Al-Damluji MS, Alfonso CE, Schob AH, Marso SP, Gilchrist IC, Moscucci M, Kandzari DE, Cohen MG (2016) Influence of Total Coronary Occlusion on Clinical Outcomes (from the Bypass Angioplasty Revascularization Investigation 2 DiabetesTrial). Am J Cardiol 117(7):1031–1038
Hoye A (2012) Management of chronic total occlusion by percutaneous coronary intervention. Heart 98(10):822–828
Galassi AR, Boukhris M, Azzarelli S, Castaing M, Marza F, Tomasello SD (2016) Percutaneous coronary revascularization for chronic total occlusions: a novel predictive score of technical failure using advanced technologies. JACC Cardiovasc Interv 9(9):911–922
Claessen BE, Dangas GD, Godino C, Henriques JP, Leon MB, Park SJ, Stone GW, Moses JW, Colombo A, Mehran R, Multinational CTOR (2013) Impact of target vessel on long-term survival after percutaneous coronary intervention for chronic total occlusions. Catheter Cardiovasc Interv 82(1):76–82
Galassi AR, Tomasello SD, Reifart N, Werner GS, Sianos G, Bonnier H, Sievert H, Ehladad S, Bufe A, Shofer J, Gershlick A, Hildick-Smith D, Escaned J, Erglis A, Sheiban I, Thuesen L, Serra A, Christiansen E, Buettner A, Costanzo L, Barrano G, Di Mario C (2011) In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention 7(4):472–479
Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, Hiasa Y, Doi O, Yamashita T, Hinohara T, Tanaka H, Mitsudo K, Investigators JCR (2011) Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv 4(2):213–221
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
SWR, HL, and BGC researched data and wrote the manuscript. SWR and BGC contributed to the study design. BGC contributed to the collection of research data. CCU contributed to provide intellectual inputs for the discussion. BGC contributed to data analysis and edited the manuscript. All authors take full responsibility for this work.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rha, SW., Li, H., Choi, C.U. et al. Impact of complete revascularization on long-term clinical outcomes for patients with diabetes mellitus and coronary chronic total occlusion lesion. Heart Vessels 37, 1679–1688 (2022). https://doi.org/10.1007/s00380-022-02079-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02079-y