Abstract
The subcutaneous implantable cardioverter-defibrillator (S-ICD) may provide comparable protection while avoiding the disadvantage of transvenous lead, but the abnormal features of the hypertrophic cardiomyopathy (HCM) electrocardiogram (ECG) make it a challenge for S-ICD template screening. We aimed to investigate S-ICD eligibility according to the S-ICD manufacturer’s surface ECG screening template in China, and further analyze its corresponding ineligible predicting factors in 12-lead suface ECG. A total of 179 HCM patients (114 males; mean age: 45 ± 14 years) underwent S-ICD screening at rest and on exercise, among which 91 patients (50.8%) were eligible for S-ICD. Among the patients who passed screening, 43 (47.3%) had 3 vectors eligibility; 64 (70.3%) screening qualified on both sides; 10 patients (11.0%) passed the screening while the electrodes located only on the left parasternal line versus 17 patients (18.7%) moved to the right line. The secondary sensing vector (Lead III) was mostly appropriate (53.6%), followed by the primary sensing vector (lead II, 53.1%) and the alternate sensing vector (Lead I, 46.9%). Higher R wave was the major cause, accounted for 70.5%, for screening failure. There existed significant difference in T wave in lead II, aVF, V5 and V6, adds R/T ratio in lead V5 and V6, between the screening success group (group A) and screening failure group (group B) at rest and on exercise. A multivariable logistic regression analysis was performed to identify that R/T ≤ 3.5 in lead V5 was the independent factor to predict the screening ineligibility, with odds ratio 3.648. S-ICD screening success is 50.8% in HCM patients, which is much lower than that in other studies. R/T ≤ 3.5 in lead V5 in 12-lead surface ECG was an independent predicting factor for screening failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypertrophic cardiomyopathy (HCM), a genetically inherited heterogeneous sarcomeric disorder that increases the risk of sudden cardiac death (SCD) mainly due to fatal ventricular arrhythmias. SCD is the most devastating consequence of HCM in younger patients, especially those below the age of 35 years. According to the latest report, with the early availability of genetic testing and cardiac magnetic resonance (CMR) imaging, the incidence rate of HCM was almost 1/200; the advent of contemporary management strategies and treatment interventions, including implantable cardioverter-defibrillator (ICD) for the high risk of SCD prevention, resulted in a low disease-related mortality rate of 0.5%/year and an opportunity for extended longevity [1, 2].
There is no doubt that the ICD has become a life-saving treatment for preventing SCD. For those who are not expected to receive pacing due to bradycardia or antitachycardia pacing (ATP) therapy, the subcutaneous ICD (S-ICD) is emerging as a new promising therapeutic option. Implanting in the lateral thoracic region of the body and using a tunneled lead to sense and deliver limits the risk of systemic infection, vascular/cardiac trauma, and lead failure since it is implanted entirely outside the vasculature [3]. EFFORTLESS study [4] found that successful defibrillation at < 80 J was achieved in 98.9% of HCM and 98.5% of non-HCM patients; one-year post-operative complication-free rates were similar (92.7% vs 89.5%); overall final shock conversion efficacy was 100% in HCM; inappropriate shocks occurred in 12.5% of HCM patients, similar to non-HCM patients. These initial data indicate the S-ICD is safe and effective in patients with HCM who are at high risk of ventricular arrhythmias, and there are no lead complications requiring reintervention.
With S-ICDs, ventricular sensing is conducted through 3 sensing vectors (primary vector, secondary vector, alternative vector), and subcutaneous electrocardiograms (ECG) recorded between 2 sensing electrodes and the pulse generator. However, patients with HCM present obviously ECG changes, containing high R and T wave, T inversion, fragmented QRS and so on. A study showed that currently available pre-implant screening algorithms recommended by the manufacturer are associated with a significant failure rate (15–16%) in patients with HCM, particularly in the high-risk subgroup [5, 6]. In other words, HCM may be a potential independent risk factor for screening failure of S-ICD. However, in the above mentioned two studies, screening success was defined as a single ECG vector satisfied the screening template. While according to 2014 ESC guidelines [7], we consider each patient should have more than one ECG vector passed screening to allow alternative programming in case of T-wave oversensing. Thus we tried to assess the exact rate of patients with HCM, on base of the definition about screening success that at least 2 vectors satisfied the screening template, passed the prerequisite S-ICD vector screening and its corresponding predicting ineligibility factors in China.
Materials and methods
Demographics
The study population included 179 consecutive HCM patients admitted to our centers, the First Affiliated Hospital of Airforce Military Medical University, between May 2017 and January 2018. The diagnosis of HCM was based upon the ESC Guidelines that echocardiographic demonstration of a hypertrophied but non-dilated left ventricle in the absence of any other cardiac or systemic disease that could be induced comparable left ventricular hypertrophy [7]. The clinical data, ECG, Echo, and stress ECG/Echo were all collected, and the S-ICD screening was achieved containing exercise stress ECG. Using routinely collected anonymous data was approved by the hospital ethics committee and deemed not to require formal patient consent.
Screening for S-ICD eligibility
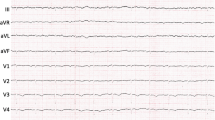
To screen S-ICD eligibility, an ECG simulating three sense vectors of the S-ICD was obtained using three-limb lead electrodes, as recommended by the S-ICD manufacturer (Boston Scientific, Natick, MA, USA). ECG lead were placed in the standard configuration (left arm = 1 cm lateral to the xiphoid process; right arm = 14 cm cranial to the left arm lead along the sternum, left leg = fifth or sixth intercostal space on the left midaxillary line) with a ground electrode placed on abdomen. The electrocardiogram was obtained at a paper speed of 25 mm/s at gains of 5, 10, and 20 mV for a period of 10 s in the supine position as well as sitting position at rest and during activation [8]. The screening protocol was repeated after moving the sternal electrodes (electrodes RA and LA) on the right parasternal line, with electrode LA at 1 cm lateral to the right sternal border and 1 cm above the xiphoid process, and electrode RA at 14 cm superior to electrode LA, no matter whether the left parasternal sensing electrode position test succeeded or failed (Fig. 1a). The morphology of the QRS complex and T wave was analyzed using the template of the patient screening tool provided by the manufacturer. The tool contained six-colored templates corresponding to the six S-ICD automatic gain morphology templates used by the discrimination algorithm (Fig. 1b). The template was placed over a single QRS-T complex and the horizontal line was aligned with the isoelectric line, whereas the left edge of the template was aligned with the onset of QRS complex. For S-ICD eligibility analysis, the QRS-T complex must lie completely inside the colored shape. Moreover, the maximum amplitude of the QRS must cross the dashed line (Fig. 1c). All tracings were analyzed by two independent experienced electrophysiologists. Using the Boston Scientific screening templates, a patient was classified to the group of“screening success” when ≥ 2 sensing vectors were acceptable for the template, at the gain of 5 mm/mv, 10 mm/mv and 20 mm/mv, in all positions (supine, sitting and on exercise) (group A). Otherwise, the patient would be classified to the group of screening failure if only one vector or none satisfied the template (group B).
a Location of the surface electrocardiogram lead and S-ICD sensing vectors during screening for eligibility for subcutaneous implantable cardioverter defibrillators (S-ICD) in left parasternal and right parasternal positions are shown separately. RA right arm, LA left arm, LL left leg, G ground. b Six different screening templates to fit the shape and size of ECG. c Examples of the surface ECG for screening pass or fail, QRS-T should entirely within the shape of the template, and QRS complex required to cross the peak zone
Surface 12-lead ECG analysis
The surface 12-lead ECGs at rest and during activation were all obtained, moreover, exercise ECG was recorded during peak exercise. Two independent electrophysiologists who were blinded to patients’ identity and S-ICD screening results analyzed the ECG separately. Each intervals measured by 2 observers were average. Lead I, II, and aVF were analyzed because they mimicked 3 sensing vectors of the S-ICD, V5 and V6 were also included because of HCM subjects. The following parameters were assessed and measured: HR (heart rate), PR Interval, QRS duration, numbers of T-wave inversion (TWI > 0.1 mv or > 1/10R wave) and QRS-T discordance, adds R, T, RS (the total QRS) amplitude and R/T in lead I, II, aVF, V5 and V6. Cornell index of RV5 plus SV1 was collected. VAT was the duration between the start of QRS and the summit of R or S wave, Tp-e was the duration from the peak to the end of T wave, RS was equal to R wave plus S wave amplitude, which denoted the total amplitude of ventricular depolarization. The lead of R/S = 1 located among all precordial lead was the R wave migration one. Reasons for failure were recorded for every analyzed vector and categorized into high T-wave voltages or T inversion, high R wave and wide QRS/QT interval.
Statistical analysis
SPSS statistical software (v22, SPSS Inc, Chicago, IL, USA) was used for all analyzes. Normally distributed continuous variables were presented as mean ± SD, and number and percentages for categorical variables. The differences of the continuous variables between two groups were assessed using two-tailed Student’s t test or the Mann–Whitney U test. Categorical variables were compared using the chi-squared test or Fisher’s exact test when the data were very unequally distributed. ROC curves were used to detect the best cutoff point of sensibility and specificity of interested parameters. Finally, A multivariable logistic regression analysis was performed to identify the independent clinical predictors of S-ICD ineligibility. P < 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 179 patients (114 males; mean age: 45 ± 14 years) visiting the HCM outpatient clinic underwent the S-ICD screening. Ninety-three patients were identified as non-obstructive HCM (NOHCM). None had implanted ICD. No statistical differences were found in age, sex, BMI and heart size, except for maximum thickness of interventricular septum (IVS) between two groups. Unlike RBBB, there was significant difference in left bundle branch block (LBBB) numbers between two groups (Table 1). Among all the screening patients, 11 patients underwent interventricular septal resection, 3 patients accepted percutaneous alcohol septal ablation, and 7 patients received percutaneous interventricular septal radiofrequency ablation.
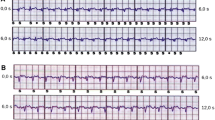
Comparison of ECGs between two groups
The surface 12-lead ECGs at rest and during activation were all obtained, unless the patients had contraindications for stress Echo or could not tolerate because of other reasons such as leg discomfort or severe left ventricular outflow obstruction. What we would like to highlight here was that there existed no difference in the exercise equivalent [(6.26 ± 1.59) vs (5.48 ± 1.77)w] and target heart rate [(132.70 ± 21.85) vs (134.75 ± 21.94) beats per minute] for patients on exercise between the two groups. Then HR, PR, QRS interval, QT, TWI and QRS-T discordance numbers were all calculated, adds R wave amplitude, T wave amplitude, R/T, RS (the total of QRS amplitude), VAT, Tp-e of lead I, II, aVF, V5, V6, Cornell index, which were all analyzed by two separate electrophysiologists. Except for QRS duration, there existed no significant difference in HR, PR interval, QT, VAT, Tp-e, TWI and R wave migration lead between the two groups, no matter at rest or on exercise. Obviously, there existed evident difference in T wave amplitude in lead II, aVF, V5 and V6 at rest and on exercise, adds R wave in lead I, II and V6, R/T in lead V5 and V6. Furthermore, not like T and R wave amplitudes, R/T were all higher in group A, which indicated that smaller T wave or proper R wave amplitude got a relative higher R/T ratio was more easier to satisfy the template (Table 2, Fig. 2).
S-ICD vector morphology analysis
For a patient to be eligible for an S-ICD, more than one ECG vector need to pass the screening template. A total of 179 HCM patients, 91 (50.8%) satisfied at morphology analysis. Among the patients who passed screening, 43 (47.3%) had 3 vectors eligibility, the left 48 (52.7%) had 2 vectors satisfied; 64 (70.3%) screening qualified on both sides; 10 patients (11.0%) passed the screening while the electrodes located only on the left parasternal line, when the electrode was switched from the usual left parasternal position to the right, 18.7% (17 patients) of previously ineligible ECG turned eligible. On the contrary, 88 (49.2%) patients failed for S-ICD screening, including 37 (20.7%) patients with 1 eligible ECG vector and 51 (28.5%) patients with no qualifying ECG vectors (Fig. 3). Among the 88 screening failure patients, 62 (70.5%) with too high R wave resulted in screening ineligibility, 17 (19.3%) with wide QRS/QT interval and 9 (10.2%) with high T wave (Fig. 4). For every object, nearly 9–12 vectors were analyzed. Among a total of 3222 sensing vectors (three positions for each vector), 2.8% vectors were absent mostly because of inappropriateness for exercise ECG, such as severe obstruction, low LVEF, leg discomfort. No matter which screening gain satisfied, it was denoted as screening successfully for this vector. The secondary sensing vector (Lead III, 53.6%) was mostly appropriate, followed by the primary sensing vector (lead II, 53.1%) and the alternate vector (lead I, 46.9%). Among the screening gain of 20mm/mv, no obvious difference was observed between two groups, and most patients were satisfied for the gain of 5mm/mv and 10mm/mv, about 12.45 and 1.40 vectors to meet the needs of gains per one in group A separately, otherwise, only 3.67 and 0.56 in group B (P < 0.05) (Table 3).
Predictors of eligibility in HCM
ROC was used to detect the best index predicting the screening results according to the area of the curve (Fig. 5). The curve showed that the AUC of R/T in lead II, aVF, V5 and V6 was much bigger. Then the logistic model took into account the above 4 values. Obviously, R/T in lead V5 was left in the last equation, and the ratio of the cutoff point was 3.5. As a result, a multivariable logistic regression analysis was performed to identify that R/T ≤ 3.5 in V5 was independent factors to predict the screening ineligibility. Logistic analyze showed that odds ratio of the parameter was 3.648. Specifically speaking, if RV5 > 3.5, the screening success rate was 3.648 times than the group which RV5 ≤ 3.5.
Discussion
HCM is the most common genetically inherited cardiovascular disease. SCD due to sustained ventricular tachycardia (VT) or ventricular fibrillation (VF) is still the most common cause of mortality, accounting for nearly 51% of all HCM-related deaths. SCD is more common in younger patients, especially those under the age of 35. Fortunately, the advent of ICD therapy as a break-through effective measure could terminate life-threatening arrhythmias between 4 and 6% per year [9]. There is no doubt that ICD is efficacious in preventing SCD. The primary difficulty for the clinician lies in how weigh the risks and benefits of ICD implantation, since as many HCM patients are young and will have a device in place throughout their adult lives. Therefore, ICD-related complications in patients with HCM cannot be ignored. There are two particular risks which should cause great concern, that is, the risk of device-related complications/malfunction, and the risk of inappropriate ICD therapy. For example, young teenagers tend to have a higher incidence of lead fractures because of the increased strain by their growth and development; furthermore, the risk of device-related complications, between 4 and 6% per year, such as pneumothorax, pericardial effusion and haematoma or pocket infection, endocarditis and upper extremity venous thrombosis/occlusion is much higher, and they will also need multiple ICD generator changes throughout their life, which also increases the relevant complications [10,11,12].
The advent of the fully subcutaneous ICD (S-ICD) avoids lead and venous-related complications, besides cardiac perforation and endocarditis since the system has no access to the heart, only implanted below the subcutaneous layer of the chest. However, the S-ICD owns several indications, containing those without a need for pacing because of bradycardia or stable regular ventricular tachycardia. Thus, S-ICD is particularly practical in younger patients for primary or secondary prevention, with no need of pacing, which could avoid the relevant complications—mentioned above as well as the potential procedural risks related to the removal of existing transvenous lead. The EFFORTLESS study [4] showed that the HCM cohort was younger and more likely to receive a primary-prevention S-ICD (88.5% vs 67.5%, P < 0.001), and its efficacy and safety was similar to non-HCM patients, which indicated the S-ICD was safe and effective in patients with HCM who were at high risk of ventricular arrhythmias and could pass preimplantation electrocardiogram screening. Inappropriate shocks were mainly due to T-wave oversensing [13]. Unfortunately, pre-screening test was not satisfactory in HCM patients, mainly because of its special ECG characteristic, such as high R wave in V5 and V6 because of LV hypertrophy, high T voltage resulted in T oversensing, wide QRS interval as a result of conduction disorders induced by myocyte hypertrophy. Louise et al.[14] reported that in patients without an indication for pacing, 7.4% would be not suitable for a S-ICD according to the QRS-T morphology screening (TMS). HCM, a heavy weight, a prolonged QRS duration and a R:T ratio<3 in the ECG lead with the largest T wave were independently associated with TMS failure, because they may not satisfy ECG criteria for adequate sensing.
In our single-center observational study, S-ICD screening failure in HCM patients was about 49.2%, which was much higher than other studies reported 7.0% and 15% [5, 15, 16]. In addition, the presence of higher R wave, T wave voltage and wide QRS/QT interval was major causes for screening failure. Just as the above mentioned, their target heart rate was (132.70 ± 21.85) vs (134.75 ± 21.94) beats per minute, respectively, both of which were similar to the maximum heart rate on exercise. Consequently, both groups of patients achieved the target exercise metabolic equivalent. Since in the previous studies [5, 14, 15], screening successfully was defined as a single ECG vector satisfied the screening template, while according to 2014 ESC guidelines, we consider each patient should have more than one ECG vector passed screening to allow alternative programming to avoid inappropriate shocks from T-wave oversensing, which resulted in a higher ineligibility rate than other studies. Second, unlike other studies [14, 16], patients in our study were defined passed successfully in both supine and standing positions at rest as well as on exercise, which might partly contribute to the higher ineligibility rate. Third, in the latter study [16], HCM patients only accounted for 12.8% of all screening subjects versus 100% of ours, which may explained its lower ineligibility. Finally, IVS and LVmax walls were all much bigger than 17mm, resulted in high R and T wave or wide QRS interval, which partly explained its high screening ineligibility. In our study, those screening successfully had less LBBB, narrower QRS interval, higher R/T ratio, and less T wave amplitude in lead V5 and V6, which all existed evident differences between two groups either at rest or on stress ECG. This was in accordance with other studies, larger T wave lead to T wave oversensing or small R/T ratio resulted in failed screening. However, VAT and Tp-e had no obvious impact on screening results, which indicated the initial ventricular depolarization and end of the ventricular repolarization had little effect on the screening results.
We could see that 91 patients (50.8%) satisfied at morphology analysis, and among those with successful screening, screening of 64 (70.3%) patients qualified on both sides; 17 patients (18.7%) whose electrode placement was switched from the usual left parasternal position to the right parasternum, making the previously ineligible ECG turning into eligible ECG; and the left 10 patients (11.0%) satisfied on single side. Thus the right side screening was so important for patients especially those screening failure on left side. Furthermore, the secondary sensing vector (Lead III, 53.6%) was mostly appropriate, followed by the primary sensing vector (lead II, 53.1%) and the alternate sensing vector (lead I, 46.9%). Between the two groups, most patients were satisfied with the gain of 5 mm/mv and 10 mm/mv, and almost 12.45 and 1.40 vectors vs 3.67 and 0.56 met the needs of gains separately (P < 0.05).
ROC curves showed that R/T II, R/T aVF, R/TV5, R/TV6 may all had more important effect on screening results. According to the data, we set the values as 1 if it is larger than the cut-off point, otherwise, as 0. Logistic regression showed that among these data, only R/TV5 entered the equation, which bigger than the cut-off point was more liable to pass the screening test than the smaller one. In other words, the patients whose R/TV5 > 3.5 was over 3.648 times easier to pass the screening compared with those ≤ 3.5. T wave amplitude less, proper R wave voltage got a bigger R/T, which indicated the possibility of screening eligibility. Otherwise, T wave oversensing will lead to screening ineligibility. It is showed that obstructive severity of HCM patients seemed to have little conquence on the screening, unlike the R/T ratio.
Limitations
This was our initial, single-center study with limited samples about S-ICD screening for HCM patients, so there is a need to enlarge the sample size in the future study. Furthermore, it is much better to perfect relevant gene tests to analyze if the gene type will affect the last results.
Conclusions
This is our initial single-center conventional study to evaluate SICD screening in HCM patients in China; the eligibility rate was 50.8%, much lower than reported data. Furthermore, 12-lead surface ECG could predict the screening results, R/T ≤ 3.5 in lead V5 was the independent predicting factor for screening failure to some degree.
References
Baudhuin LM, Kotzer KE, Kluge ML, Maleszewski JJ (2015) What is the true prevalence of hypertrophic cardiomyopathy? J Am Coll Cardiol 66(16):1845–1846
Maron BJ, Rowin EJ, Casey SA, Link MS, Lesser JR, Chan RH, Garberich RF, Udelson JE, Maron MS (2015) Hypertrophic cardiomyopathy in adulthood associated with low cardiovascular mortality with contemporary management strategies. J Am Coll Cardiol 65(18):1915–1928
Rhyner J, Knight PB (2014) Totally subcutaneous implantable defibrillator. Cardiol Clin 32(2):225–237
Lambiase PD, Gold MR, Hood M, Boersma L, Theuns DA, Burke MC, Weiss R, Russo AM, Kaab S, Knight BP (2016) Evaluation of subcutaneous ICD early performance in hypertrophic cardiomyopathy from the pooled EFFORTLESS and IDE cohorts. Heart Rhythm 13(5):1066–1074
Maurizi N, Olivotto I, Olde Nordkamp LR, Baldini K, Fumagalli C, Brouwer TF, Knops RE, Cecchi F (2016) Prevalence of subcutaneous implantable cardioverter-defibrillator candidacy based on template ECG screening in patients with hypertrophic cardiomyopathy. Heart Rhythm 13(2):457–463
Weinstock J, Bader YH, Maron MS, Rowin EJ, Link MS (2016) Subcutaneous implantable cardioverter defibrillator in patients with hypertrophic cardiomyopathy: an initial experience. J Am Heart Assoc 5(2):e002488
Authors/Task Force members, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J Nihoyannopoulos P, Nistri S, Pieper PG Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H (2014) 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy. The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 35(39):2733-2739.
Ip JE, Wu MS, Kennel PJ, Thomas G, Liu CF, Cheung JW, Markowitz SM, Lerman BB (2017) Eligibility of pacemaker patients for subcutaneous implantable cardioverter defibrillators. J Cardiovasc Electrophysiol 28(5):544–548
Maron BJ, Olivotto I, Spirito P, Casey SA, Bellone P, Gohman TE, Graham KJ, Burton DA, Cecchi F (2000) Epidemiology of hypertrophic cardiomyopathy-related death: revisited in a large non-referral-based patient population. Circulation 102(8):858–864
Thavikulwat AC, Tomson TT, Knight BP, Bonow RO, Choudhury L (2016) Appropriate implantable defibrillator therapy in adults with hypertrophic cardiomyopathy. J Cardiovasc Electrophysiol 27(8):953–960
Maron BJ (2010) Risk stratification and role of implantable defibrillators for prevention of sudden death in patients with hypertrophic cardiomyopathy. Circ J 74(11):2271–2282
O'Mahony C, Lambiase PD, Quarta G, Cardona M, Calcagnino M, Tsovolas K, Al-Shaikh S, Rahman SM, Arnous S, Jones S, McKenna W, Elliott P (2011) The long-term survival and the risks and benefits of implantable cardioverter defibrillators in patients with hypertrophic cardiomyopathy. Heart 98(2):116–125
Lin G, Nishimura RA, Gersh BJ, Phil D, Ommen SR, Ackerman MJ, Brady PA (2009) Device complications and inappropriate implantable cardioverter defibrillator shocks in patients with hypertrophic cardiomyopathy. Heart 95(9):709–714
Olde Nordkamp LRA, Warnaars JLF, Kooiman KM, de Groot JR, Bram Rosenmoller, Wilde AAM, Knops RE (2014) Which patients are not suitable for a subcutaneous ICD: incidence and predictors of failed QRS-T-wave morphology screening. J Cardiovasc Electrophysiol 25(5):494–499
Francia P, Adduci C, Palano F, Semprini L, Serdoz A, Montesanti D, Santini D, Musumeci B, Salvati A, Volpe M, Autore C (2015) Eligibility for the subcutaneous implantable cardioverter-defibrillator in patients with hypertrophic cardiomyopathy. J Cardiovasc Electrohpysiol 26(8):893–899
Randles DA, Hawkins NM, Shaw M, Patwala AY, Pettit SJ, Wright DJ (2014) How many patients fulfil the surface electrocardiogram criteria for subcutaneous implantable cardioverter-defibrillator implantation? Europace 16(7):1015–1021
Acknowledgements
We specifically thank Professor Changsheng Chen for his guidance and support mainly in statistical analysis.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Guo, L., Zhang, M., Hu, M. et al. Prevalence of subcutaneous implantable cardioverter-defibrillator based on template ECG screening and ineligible surface ECG predicting factors in patients with hypertrophic cardiomyopathy in China. Heart Vessels 34, 851–859 (2019). https://doi.org/10.1007/s00380-018-1300-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1300-8