Abstract
We aimed to investigate the characteristics of changes in amount of physical activity of patients with peripheral arterial disease (PAD) before/after endovascular treatment (EVT) combined with exercise training. Twenty-two patients with peripheral arterial disease at stage-II of the Fontaine classification who received EVT combined with exercise training were included in this study. A tri-axial accelerometer was used to record physical activity every day from the day before surgery to 3 months after discharge from hospital. The mean number of walking steps before surgery was 2664 steps (611 steps–5404 steps), whereas those after surgery was 3393 (567 steps–7578 steps). Ankle Brachial Index (from 0.69 to 1.03; p < 0.001), maximum walking distance (from 728.2 to 1271.8 m; p < 0.05) and Vascu-QOL (from 98.9 to 137.9; p < 0.01) showed improvement between before and after surgery. Physical activity of patients with PAD was still low at 3 months after surgery even though walking ability, QOL, and self-efficacy were improved after EVT combined with exercise training. Among the 22 patients, the number of walking steps increased in 17 of them and decreased in 5 of them. Compared with the patients in the increased-steps group, those in the decreased-steps group were significantly older (p < 0.05), and had a significantly higher cardiovascular event rate within the first 3 months after surgery (p < 0.05). These results suggested that, not only the improvement of walking ability, but increase in physical activity after EVT combined with exercise training is also important for short-term prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endovascular treatment (EVT), which is performed for patients with peripheral arterial disease (PAD), is minimally invasive and highly safe treatment approach and is rapidly increasing in number [1]. It is true that the maximum walking distance (MWD) will improve after EVT in a short period of time due to the improvement of blood circulation, but it is reported that walking ability will significantly improve in a mid- to long period of time with the concomitant use of supervised exercise training rather than EVT alone [2]. Recent studied have suggested that the improvement of walking ability with the concomitant use of supervised exercise training in patients with PAD is not because of a hemodynamic changes, but due to the improvement of cardiopulmonary function and skeletal muscle function [3, 4]. Frans et al. [5] conducted a systematic review and showed that EVT combined with exercise training was effective for improving not only walking ability but also quality of life (QOL), which means that continuing the exercise training even after EVT is effective for improving both walking ability and QOL.
On the other hand, it is reported that patients with PAD do less physical activity compared with healthy persons [6–8] and that those who do less physical activity in their daily life tend to have poor physical functions and have a high incidence of PAD progression and cardiovascular events [9, 10]. Although EVT is characterized by allowing early discharge to home owing to its minimal invasiveness, much remains unclear about the details of the changes in physical activity amount after EVT. EVT is beneficial not only for the improvement of walking ability of patients with PAD but also for the maintenance/improvement of their physical activity amount. This fact is important from the perspective that EVT will prevent cardiovascular events. Many studies have reported so far on the importance of increasing the physical activity amount for several diseases management, but studies reporting on the changes in the amount of physical activity at before/after EVT are scarce.
In this study, therefore, we aimed to investigate the characteristics of changes in amount of physical activity of patients with PAD before/after EVT combined with exercise training.
Methods
Participants
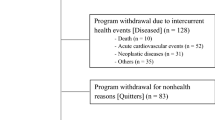
Of the 135 patients with PAD at stage-II of the Fontaine classification who received EVT at our hospital from January 2013 to August 2015, a total of 33 patients who agreed to participate in this study and received supervised exercise training by a physical therapist after EVT were enrolled. Patients who received invasive treatment such as thrombo-endarterectomy involving the skin incision were not included in this study. All patients received percutaneous transluminal angioplasty. Among them, 22 cases of 29 limbs were selected excluding those who were unable to walk since before surgery and those who withdrew their agreement. The mean age of the participants was 76.0 years (60–84; 17 men and 5 women). Table 1 shows the patient characteristics and treated regions.
Exercise therapy after EVT
After EVT, all the patients started standing and walking training from the day after surgery. Supervised exercise training was started when a patient was found to have no complications and became able to walk on level ground independently. One course of supervised exercise training was comprised of warm-up, treadmill walking (20 min) and cool-down, and was performed 5 times a week. The exercise prescription was compliant with the guidelines of TASC-II [11]. The speed of walking and the gradient load was increased gradually as the walking ability improved. The mean days of the exercise training was 6.87. On discharge from hospital, all the patients were given instructions to set a goal of doing exercise at least 3 times a week for more than 30 min.
Prior to hospital discharge, encouragement of walking from the medical doctor, medication instruction from the pharmacist, along with lifestyle guidance from nurse were carried out. ADL guidance was also given to prevent excessive flection at the stent insertion site. After discharged from the hospital in this study, all patients did not attend outpatient exercise rehabilitation program.
Measurement of PA
A waist-mounted physical activity monitor (Active style Pro HJA-350IT, Omron Co. Japan) was used to record the number of steps, time, and metabolic equivalents (METs) every day from before surgery to 3 months after discharge from hospital. The physical activity monitor was attached all the time from waking up to going to sleep except the time of bathing. Excluding data during days when the wearing time measured by a three-axis acceleration sensor was less than 480 min/day for some reason, the mean value such as the number of steps, time, and METs before admission and 3 months after discharge were adopted. The mean number of days when the physical activity monitor data were adopted was 11.6 days before admission and 49.4 days at 3 months after discharge.
Evaluation of PAD, walking ability, psychological state, and ADL
The following factors were evaluated at before admission and 3 months after discharge: Ankle Brachial Index (ABI) to evaluate arterial sclerosis; maximum walking distance (MWD) and Walking Impairment Questionnaire (WIQ) to evaluate walking ability [12]; Hospital Anxiety and Depression Scale (HADS) to evaluate anxiety/depression [13], Self-Efficacy for Physical Activity (SEPA) to evaluate subjective self-efficacy [14], and Vascular Quality of Life Questionnaire (Vascu-QOL) to evaluate activities of daily life [15].
Since not a few patients showed difficulty to walk on a treadmill in this patients population, we measured the field walking distance continued to walk as much as they can between the mark placed at 10 m intervals. We instructed before the test as follows; “Remember that the object is to walk as far as possible, but don’t run or jog.”
Analytical methods and statistical procedures
We compared the mean number of steps before surgery with those 3 months after discharge from hospital, and defined the patients with increased steps as the increased-steps group and patients with decreased steps as the decreased-steps group. Then we compared patients demographics, postoperative course, postoperative cardiovascular events, and METs hour (life activity, walking activity, total activity), and MWD, WIQ, HADS, SEPA, and Vascu-QOL between the two groups. SPSS (ver. 21.0; IBM, Tokyo, Japan) was used as statistical analysis software. Paired t test, unpaired t test, χ 2 test were used to compare the two groups. A two-sided test was used with p value of 0.05 defined as statistically significant.
Research ethics
This study was approved by the Ethical Committee of Jyuzenkai Medical Corporation Sakakibara Heart Institute of Okayama (approval number: 20140901). Written as well as oral informed consent was obtained from all patients prior to participation in this study.
Results
Neither death nor complications occurred to all the patients during hospitalization. The mean days of hospitalization after surgery were 6.9 ± 3.7 days, and all the discharged patients were able to walk home on their own.
-
1.
Comparison of PA between before and after surgery
The mean number of steps before surgery was 2664 steps (611 steps–5404 steps), whereas those after surgery was 3393 (567 steps–7578 steps). There was no statistical significance between them. Among the 22 patients, the number of steps increased in 17 of them and decreased in 5 of them. There was no significant difference in the METs hour between before and after surgery in all the items such as life activity, walking activity, and total activity (Table 2).
-
2.
Comparison of ABI, walking ability, psychological state, and ADL ability between before and after surgery
ABI showed a significant improvement between before and after surgery (0.69 vs. 1.03; p < 0.001). MWD (from 728.2 to 1271.8 m; p < 0.05) and WIQ (from 126.9 to 271.6; p < 0.001) showed a significant improvement after surgery. SEPA (from 36.1 to 61.3; p < 0.01) and Vascu-QOL (from 98.9 to 137.9; p < 0.01) also showed a significant improvement after surgery. HADS did not show any significant difference in all the sections of “anxiety”, “depression”, and “total score”.
-
3.
Comparison between the increased-steps group and the decreased-steps group
The rate of change increased by 42.3 % in the increased-steps group (n = 17) and decreased by 21.8 % in the decreased-steps group (n = 5), respectively, from before- to after surgery (Table 3). Compared with the patients in the increased-steps group, those in the decreased-steps group were significantly older (p < 0.05), and had a significantly higher cardiovascular event rate within the first 3 months after surgery (p < 0.05).
There was no significant difference in the mean walking steps at both before and after surgery, but a significant difference in the METs hour of walking activity was found between the increased-steps group (2.81 ± 1.12) and the decreased-steps group (1.50 ± 0.68) (Table 4). Although there was no significant difference in MWD between the increased-steps group and the increased-steps group, the former group showed a significant difference at 3 months after discharge (p < 0.05). While WIQ was significantly higher in the increased-steps group than in the decreased-steps group at 3 months after discharge (302.5 ± 95.5 vs. 163.3 ± 103.1, p < 0.05), there was no significant difference in SEPA, Vascu-QOL, and HADS between the two groups.
Discussion
Previous studies have reported the respective effects of EVT and supervised exercise training in patients with PAD. Timothy et al. [16] reported the effect on maximum walking time on the treadmill after EVT alone and alone after exercise therapy for 6 months. EVT alone increased 169 % of the maximum walking time compared to the pre-EVT, and exercise training alone increased 211 % of the maximum walking time compared to the pre-exercise training. Furthermore, there are many reports that EVT combined with exercise training improved maximum walking distance and QOL compared with EVT alone and exercise training alone [5, 17, 18].
Walking ability, QOL, and self-efficacy significantly improved after EVT combined with exercise training in this study as similarly as previous studies. It can be inferred that the improvement of walking ability is attributable to the improvement of blood supply to the lower limb skeletal muscles during walking due to revascularization by EVT in addition to the improvement of blood flow redistribution and oxygen utilization efficiency in the skeletal muscles due to supervised exercise training. Moreover, since there is a report that SEPA and Vascu-QOL will increase along with the improvement of the postoperative walking ability [18, 19], QOL and self-efficacy of the patients in this study may also have improved along with improvement of walking ability.
Although walking ability, QOL, and self-efficacy showed an improvement after EVT combined with exercise training, no significant improvement was observed in the mean number of walking steps at 3 months after surgery. In addition, the mean number of walking steps decreased in 5 out of 22 patients since before surgery. Compared between the cases that increased the number of walking steps after surgery and those that decreased the number of walking steps after surgery, the decreased-steps group was significantly older in age and lower in preoperative WIQ, MWD, and self-efficacy. It can be inferred that because of the deterioration of the walking function since before surgery due to the effect of aging, the obtained mean number of walking steps fell short of improvement although there was an improvement in MWD, WIQ, and SEPA after surgery. In this study, we did not investigate into the physical functions. However, the fact that all the patients in the decreased-steps group had previous history of coronary artery disease and a high rate of history of cerebrovascular disease and motor organ disease leads to a possibility that physical functions and exercise intolerance had already been deteriorated since before surgery.
In the decreased-steps group, physical activity decreased significantly after surgery although MWD and WIQ showed a significant improvement after surgery. As is reported in a study [7], PAD patients with low physical activity are susceptible to cardiovascular events and will have a poor prognosis. In our study, too, the incidence of cardiovascular event was significantly high in the first 3 months after surgery in the decreased-steps group. Therefore, not only the improvement of walking ability, but also the increase in physical activity is important after the EVT. In the increased-steps group, on the other hand, the number of walking steps significantly increased after surgery, which was relatively less than the age-specific mean walking steps reported in the National Health Survey [20, 21]. The mean number of walking steps of men in their 70s or over was 5393. Based on this, it was revealed that the mean number of walking steps in the increased-steps group was about 70.5 % and that physical activity of patients with PAD was still low at 3 months after surgery even though walking ability, QOL, and self-efficacy were improved. Taken together, postoperative follow-up of physical activity by the quantitative evaluation is required even for minimally invasive EVT.
The major limitation of this study is the lack of the number of subjects. In addition, we did not perform a power analysis before starting this study as it was designed as a longitudinal observational study to evaluate natural recovery of physical activity after EVT. Future randomized controlled trials are needed to help critically evaluate the effects of specific intervention on recovery of physical activity after EVT.
References
Annual report on national survey for number of vascular surgery in Japan 2012. http://www.jsvs.org/ja/enquete/aggregate_2012-2.pdf
Greenhalgh RM, Belch JJ, Brown LC, Gaines PA, Gao L, Reise JA, Thompson SG, Participants Mimic Trial (2008) The adjuvant benefit of angioplasty in patients with mild to moderate intermittent claudication (MIMIC) managed by supervised exercise, smoking cessation advice and best medical therapy: results from two randomised trials for stenotic femoropopliteal and aortoiliac arterial disease. Eur J Vasc Endovasc Surg 36(6):680–688
Parmenter BJ, Dieberg G, Smart NA (2015) Exercise training for management of peripheral arterial disease: a systematic review and meta-analysis. Sport Med 45:231–244
Kruidenier LM, Nicolai SP, Rouwet EV, Peters RJ, Prins MH, Teijink JAW (2011) Additional supervised exercise therapy after a percutaneous vascular intervention for peripheral arterial disease: a randomized clinical trial. J Vasc Interv Radiol 22:961–968
Frans FA, Bipat S, Reekers JA, Legemate DA, Koelemay MJ (2012) Systematic review of exercise training or percutaneous transluminal angioplasty for intermittent claudication. Br J Surg 99(1):16–28
McDermott MM, Liu K, O’Brien E, Guralnik JM, Criqui MH, Martin GJ, Greenland P (2000) Measuring physical activity in peripheral arterial disease: a comparison of two physical activity questionnaires with an accelerometer. Angiology 51(2):91–100
Lauret GJ, Fokkenrood HJ, Bendermacher BL, Scheltinga MR, Teijink JA (2014) Physical activity monitoring in patients with intermittent claudication. Eur J Vasc Endovasc Surg 47(6):656–663
Gardner AW, Montgomery PS, Scott KJ, Afaq A, Blevins SM (2007) Patterns of ambulatory activity in subjects with and without intermittent claudication. J Vasc Surg 46(6):1208–1214
Garg PK, Liu K, Tian L, Guralnik JM, Ferrucci L, Criqui MH, Tan J, McDermott MM (2009) Physical activity during daily life and functional decline in peripheral arterial disease. Circulation 119(2):251–260
Leeper NJ, Myers J, Zhou M, Nead KT, Syed A, Kojima Y, Caceres RD, Cooke JP (2013) Exercise capacity is the strongest predictor of mortality in patients with peripheral arterial disease. J Vasc Surg 57(3):728–733
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, TASC II Working Group (2007) Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg 45(Suppl S):S5–67
Hiatt WR, Hirsch AT, Reqensteiner JG, Brass EP (1995) Clinical trials for claudication. Assessment of exercise performance, functional status, and clinical end points. Vascular Clinical Trialists. Circulation 92(3):614–621
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6):361–370
Ewart CK, Taylor CB, Reese LB, DeBusk RF (1983) Effects of early postmyocardial infarction exercise testing on self-perception and subsequent physical activity. Am J Cardiol 51(7):1076–1080
Morgan MB, Crayford T, Murrin B, Fraser SC (2001) Developing the Vascular Quality of Life Questionnaire: a new disease-specific quality of life measure for use in lower limb ischemia. J Vasc Surg 33(4):679–687
Murphy TP, Hirsch AT, Ricotta JJ, Cutlip DE, Mohler E, Regensteiner JG, Comerota AJ, Cohen DJ, CLEVER Steering Committee (2012) Supervised exercise vs primary stenting for claudication due to aortoiliac peripheral disease: 6-month outcomes from the CLEVER Study. Circulation 125(1):130–139
Fakhry F, Spronk S, van der Laan L, Wever JJ, Teijink JA, Hoffmann WH, Smits TM, van Brussel JP, Stultiens GN, Derom A, den Hoed PT, Ho GH, van Dijk LC, Verhofstad N, Orsini M, van Petersen A, Woltman K, Hulst I, van Sambeek MR, Rizopoulos D, Rouwet EV, Hunink MG (2015) Endovascular revascularization and supervised exercise for peripheral artery disease and intermittent claudication. A randomized clinical trial. JAMA 314(18):1936–1944
Spronk S, Bosch JL, den Hoed PT, Veen HF, Pattynama PM, Hunink MG (2009) Intermittent claudication: clinical effectiveness of endovascular revascularization versus supervised hospital-based exercise training—randomized controlled trial. Radiology 250(2):586–595
Lundgren F, Dahllöf AG, Lundholm K, Scherstén T, Volkmann R (1989) Intermittent claudication—surgical reconstruction or physical training? A prospective randomized trial of treatment efficiency. Ann Surg 209(3):346–355
Koba S, Tanaka H, Maruyama C, Tada N, Birou S, Teramoto T, Sasaki J (2011) Physical activity in the Japan population: association with blood lipid levels and effects in reducing cardiovascular and all-cause mortality. J Atheroscler Thromb 18(10):833–845
National Health and Nutrition Examination Survey in Japan (2013). http://www.mhlw.go.jp/stf/houdou/0000067890.html
Acknowledgments
This work was supported by JSPS KAKENHI Grant Number 26670964.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interests to disclose.
Rights and permissions
About this article
Cite this article
Otsuka, S., Morisawa, T., Yuguchi, S. et al. Clinical importance of change in physical activity after endovascular treatment combined with exercise training in patients with peripheral arterial disease. Heart Vessels 32, 143–148 (2017). https://doi.org/10.1007/s00380-016-0856-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0856-4