Abstract
Purpose
Retrograde transurethral anatomical enucleation of the prostate is gaining momentum as a new concept in transurethral surgery of benign prostatic hyperplasia. Its adaptation is boosted by the familiarity of urologists with the finger-assisted anatomical enucleation of the adenoma during open prostatectomy and the combination of this well-established concept with the minimal invasive characteristics of transurethral surgery. The thulium laser appears as an ideal energy source for such operation. In this work, current evidence on thulium laser-assisted anatomical enucleation of the prostate (ThuLEP) is being reviewed.
Materials and Methods
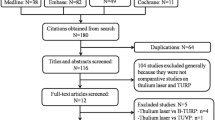
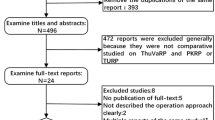
A comprehensive literature review was performed on Medline, PubMed, and Cochrane databases retrieving all literature on thulium laser-assisted prostatectomy between 2006 and 2015. Experimental studies, review articles and editorial comments as well as studies on thulium laser-assisted approaches other than ThuLEP (i.e., ThuVEP, ThuVAP or ThuVARP) were excluded from the analysis.
Results
In total, six original articles on either surgical technique or clinical outcomes were retrieved. With regard to functional results, ThuLEP presented no significant differences toward the standard treatment (TURP/HoLEP) arm in two randomized controlled trials and favorable outcomes in available prospective cohorts. Observed morbidity was minimum and comparable with the rest of transurethral literature.
Conclusions
ThuLEP literature is still very limited. Based on the available data, the approach is safe and effective, demonstrating favorable outcomes, comparable with the current standard treatment options. Further documentation of ThuLEP outcomes is necessary to define the optimum indications of this novel technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first clinical report on holmium laser treatment of benign prostatic enlargement (BPE) can be traced back to 1995 when Gilling et al. [1] documented the feasibility and safety of holmium laser application in prostatic ablation solely or in combination with Nd:YAG laser. Since then, various laser treatments of benign prostatic obstruction due to BPE have been developed and have become potent challengers of the gold standard surgical treatments, i.e., transurethral resection of the prostate (TURP) and open (simple) prostatectomy (OP) [2, 3].
Thulium (Tm:YAG) laser has been introduced into urological soft tissue surgery in 2005. It emits laser energy in a continuous wave fashion at a wavelength of 2013 nm. As in the pulsed Ho:YAG, the particular wavelength is close to the absorption peak of water, and thereby, Tm:YAG laser demonstrates a shallow tissue penetration, coagulation zone and necrotic tissue zone providing high surgical safety. In addition, Tm:YAG laser has an excellent hemostatic and vaporization efficiency that renders it a very appealing energy source for prostate surgery [2].
The surgical principles of all approaches using laser energy in transurethral prostatectomy can be divided into three categories: (1) vaporization/ablation, (2) resection and (3) enucleation with or without the aid of a mechanical tissue morcellator [4]. Accordingly, currently accepted international consensus nomenclature subdivides all Tm:YAG-assisted techniques into ThuVAP (Thulium:YAG vaporization of the prostate), ThuVARP (Thulium:YAG vaporesection of the prostate), ThuVEP (Thulium:YAG vapoenucleation of the prostate) and finally transurethral anatomical enucleation of the prostate with Tm:YAG support (ThuLEP) [3, 4].
ThuLEP was introduced in 2010 by Herrmann et al. [5], and in contrast to the rest of energy-based transurethral enucleating techniques, it is characterized by the blunt/mechanical enucleation of the adenoma without the use of energy (retrogradely separating the adenoma over its surgical capsule with the use of the tip of laserscope), in accordance with the finger preparation of the adenoma during OP. Following blunt dissection, punctual coagulation of capsular bleeding vessels with the use of Tm:YAG laser establishes a bloodless field and a minimum energy exposure on the pericapsular tissue. Available clinical data on ThuLEP are sparse, and thus in the present article, we aim to summarize the surgical outcomes and evidence from the literature.
Materials and methods
A comprehensive literature review was performed on Medline, PubMed, and Cochrane databases retrieving all literature on thulium laser-assisted prostatectomy between 2006 and 2015. Terms used in search engines were: ThuVAP, ThuVARP, ThuVEP, ThuLEP, TmLEP, thulium, thulium enucleation, prostate enucleation, thulium vapoenucleation, thulium vaporization, 2 micron, tangerine, TmLRP-TT and Revolix™. Experimental studies, review articles and editorial comments as well as studies on thulium laser-assisted approaches other than ThuLEP (i.e., ThuVEP, ThuVAP or ThuVARP) were excluded from the analysis.
Results
In total, six articles on ThuLEP were identified. One manuscript covered the description of the technique and did not include clinical outcomes [5]. As a result, only five studies provided surgical data for analysis. The latter studies include two prospective cohorts (level of evidence IIa) and three randomized controlled trials comparing ThuLEP with TURP or HoLEP (level of evidence 1b) [6–10]. The study of Shao et al. [8] was in Chinese, and data were extracted by the English abstract and after personal communication with the authors. Still, given that an updated review of the same patient cohort was available by the same group of authors, the particular publication was not reviewed in the current analysis [8, 9].
Patient selection, morcellation protocols and follow-up of included studies
Heterogeneity in patient selection within ThuLEP literature was evident. Iacono et al. [6] enrolled patients with prostate volumes (PV) larger than 75 cc (median 108.08 ml), whereas Zhang et al. [9] enrolled patients with PV < 80 ml (median 46.6 ml in the ThuLEP arm). In contrast, Świniarski et al. [10] and Rausch et al. [7] enrolled consecutive patients with PV of any size (28–126 and 17–180 ml accordingly) with a median of 62 and 85 ml for ThuLEP cases accordingly. The above heterogeneity should be taken into consideration when evaluating ThuLEP results given that prostatic volume is a well-established predictor of perioperative outcomes. Management of enucleated prostatic lobes was also different among studies. Tissue morcellation was performed either conventionally via a mechanical tissue morcellator or with a mushroom technique [6, 7, 9, 10]. The latter technique consists of fragmentation of the three enucleated mushroom-like pedicles (medial and lateral devascularized lobes, crowded at the bladder neck) with the use of the electrocautery loop [11]. Finally, follow-up periods varied among studies between short term (up to 3 months) and intermediate term with 12, 18 and 24 months of follow-up [6, 7, 9, 10]. Preoperative patient’s characteristics in each study are summarized in Table 1.
Perioperative outcomes of ThuLEP
Mean operative time including morcellation ranged between 70 and 102 min. Blood loss as documented by hemoglobin decrease was minimum ranging between 0.5 and 1.27 g/dl. Catheterization time ranged between 2.1 and 2.4 days, and hospitalization ranged between 2.1 and 6.5 days according to the hospitalization protocol of each department. Details on the perioperative outcomes of each study are presented in Table 2.
Efficacy of ThuLEP
Overall, ThuLEP demonstrated excellent efficacy in the relief of prostatic obstruction in all studies as documented by up to 87 % of prostatic volume reduction [6]. PSA reduction as an emerging indicator of efficiency in adenoma resection varied between 30.4 and 90 % [12]. In addition, functional outcomes were favorable with an improvement in Q max comparable with the HoLEP and TURP arms in the RCTs, minimum post-void residual volumes and excellent IPSS and quality of life improvement for the majority of patients. Functional and QoL outcome details of each study are presented in Table 3.
ThuLEP complications
Overall, ThuLEP demonstrated an excellent safety profile in all reported series. Lack of electrolyte imbalance was evident in all studies, and blood loss was generally minimum. Blood transfusion due to postoperative hematuria was deemed necessary only in 2.7 % of patients in the study of Iacono et al. [6] recruiting only large (> 75 ml) prostate sizes and in 0.9 % of patients in the prospective study of Rausch et al. [7] where a selection bias in favor of elder patients (mean patients age 73 years) with more comorbidities was evident. No transfusion was reported in the rest of the studies. Bladder wall injuries were reported in 1.3–5.6 % of patients in the studies where a mechanical morcellator was employed and in none of the studies where the mushroom technique was used. Recatheterization rates in the immediate postoperative period varied significantly among studies. Recatheterization due to residual adenoma was reported in 1.4 and 2.7 % in the studies of Zhang et al. [9] and Iacono et al. [6] accordingly, while no recatheterization was reported in the RCT of Swiniarski et al. [10]. In contrast, catheter replacement due to urinary or clot retention was reposted in 6.8 % in the study of Rausch et al. Of notice, 5.1 % of patients in the latter study were operated under ongoing oral anticoagulation. No clot retention was reported in the rest of the studies [7]. Finally, surgical capsule perforation was reported in the RCT of Zhang et al. [9] in one patient (1.4 %) similarly to the HoLEP arm of the study which was managed by suprapubic drainage, whereas no such complication was reported in the two other publications.
Postoperative irritative symptoms ranged between 6.7 and 18.5 % and were all transient with no patient reporting symptoms at the end of each study period. Urge urinary incontinence was reported in 6.7 % of patients in the study of Iacono et al. [6] recruiting patients with large prostate volumes, but none of patients had incontinence at 12 months. Rausch et al. [7] reported urge urinary incontinence in 3 % and stress incontinence in 0.5 % (one patient) of reviewed patients during the 24 months of follow-up without further definition on the course of these cases. Urethral or bladder neck strictures development was reported in 0–5.6 % of cases. Reoperation due to residual tissue during the 24 months of follow-up was reported in 1.7 % by Rausch et al. [7] and in 3.7 % (two cases) of patients in the RCT of Świniarski et al. [10]. Perioperative and postoperative complications of ThuLEP are summarized in Table 4.
Discussion
Retrograde transurethral anatomical enucleation of the prostate represents a new concept in transurethral surgery of BPH with very promising results as indicated by its rapid diffusion and adaptation by many urologists worldwide considering its recent introduction. Its adaptation is boosted by the familiarity of urologists with the finger-assisted anatomical enucleation of the adenoma during OP and the combination of this well-established concept with the minimal invasive characteristics of transurethral surgery. It should be stressed that only energy-free/blunt dissection following the plane over prostatic capsule is entitled anatomical enucleation as opposed to the rest of energy-based enucleating transurethral procedures where the plane is created by application of energy (e.g., HoLEP, ThuVEP, etc.) (Fig. 1). In addition, it should be emphasized that the concept of anatomical enucleation being a widely energy-free technique can be performed with any kind of energy for hemostasis and not only thulium laser. Accordingly, variations of anatomical transurethral enucleation have been developed with other energy sources such as GreenLight laser (GreenLEP) [13]. Still, thulium laser appears as an excellent energy source for retrograde anatomical enucleation of the prostate as it offers a clear and bloodless incision through prostatic tissue necessary in the initial steps of the operation when incision at 5 and 7 o’clock of bladder neck is performed. In addition, it demonstrates excellent hemostatic properties necessary for punctual coagulation of penetrating capsular vessels during enucleation. Finally, it has a narrow penetration depth protecting pericapsular tissue from unnecessary energy exposure [4].
Retrograde anatomical enucleation of the adenoma possesses several advantages over conventional transurethral resection. First of all, prostatic enucleation ensures a complete adenoma removal similar to OP ensuring excellent and long-term functional results and low recurrence rate. In addition, enucleation over surgical prostatic capsule provides a clear anatomical landmark throughout the procedure, assisting orientation, which is mostly important in the cases of large adenomas where consistent access to verumontanum or bladder neck might not be always possible. Finally, the blunt energy-free enucleation diminishes energy scattering to the periphery and potentially diminish postoperative irritative symptoms or damage to structures in close proximity.
Available cohorts on ThuLEP are still very limited and consisted of only five studies including two prospective cohorts, two short-term-follow-up RCTs and one intermediate-term RCT [6–10]. Extracting safe conclusion from the published literature on ThuLEP is hindered by the heterogeneity of studied populations in the published literature. Recruited prostatic volumes varied significantly from 17 to 210 ml, whereas predictors of adverse outcomes such as preoperative catheterization ranged notably from 26 % to nearly 40 % in the study of Rausch et al. The acknowledged by the authors bias in favor of an elder population (22 %; >80 years) with significant comorbidities (49 %; ASA 3 or 4) in the latter study might explain why functional treatment failure requiring permanent catheterization (8.1 %), or secondary surgery (0.9 %) was reported in up to 9 % of cases at 24 months of follow-up which is the longest follow-up in the published literature [7].
Current experience on ThuLEP indicates that the approach demonstrates favorable results in all prostatic sizes though small prostatic volumes (<50 ml) have been associated with a higher incidence of treatment failure. In addition, age >80 years and the presence of comorbidities as indicated by the American Society of Anesthesiologists (ASA) classification have also been identified as predictors of treatment failure [7]. In any case, results derived from the available RCTs define ThuLEP effectiveness as comparable with HoLEP in prostates <80 ml and TURP for any prostatic size volumes [9, 10]. Systematic reviews of the literature acknowledge the lack of evidence in thulium-assisted transurethral procedures. Still, based on current limited data, all thulium-based approaches are regarded as equal to the rest well-established procedures (e.g., monopolar and bipolar TURP, HoLEP, etc.) [3, 14].
Published literature on ThuLEP reveals a favorable safety profile for the approach. During the operation, ThuLEP shares the same general challenges with all transurethral enucleation approaches which are the risk of surgical capsule perforation during enucleation and the chance of bladder wall laceration and/or perforation during morcellation. Surgical capsule perforation is generally avoided during ThuLEP as blunt dissection of adenoma over its capsule not only minimizes such a risk but also ensures proper capsule visualization during enucleation maneuvers [5]. Such a complication has been reported in only one patient throughout ThuLEP literature [9]. Bladder wall injury during morcellation has been reported in up to 5.56 % of cases when a mechanical tissue morcellator was employed [10].
The excellent hemostasis provided by thulium laser application is evidenced by a limited hemoglobin decrease (0.5–1.27 g/dl) in the vast majority of patients. This is consistent with reports for other Tm:YAG-based techniques. Available RCTs revealed that ThuLEP resulted in significantly lower blood loss and transfusion rates than TURP (0.95 vs 1.81 g/dl and 0 vs 3.85 % accordingly) and comparable outcomes with HoLEP [9, 10]. Recatheterization rates in the published literature varied significantly among studies (0, 1.4, 2.7 and 6.8 %) reflecting the heterogeneity of studied populations [6, 7, 9, 10]. However, reported rates are low and at least comparable with the rest of transurethral literature.
Conclusions
ThuLEP literature is still very limited. Based on the available data, the approach is safe and effective, demonstrating favorable outcomes, comparable with the current standard treatment options. Further documentation of ThuLEP outcomes is necessary to define the optimum indications of this novel technique.
References
Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR (1995) Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol 9(2):151–153
Teichmann HO, Herrmann TR, Bach T (2007) Technical aspects of lasers in urology. World J Urol 25(3):221–225
Herrmann TR, Liatsikos EN, Nagele U et al (2012) EAU guidelines on laser technologies. Eur Urol 61(4):783–795
Bach TL, Xia SJ, Yang Y et al (2010) Thulium: YAG 2 mum cw laser prostatectomy: where do we stand? World J Urol 28(2):163–168
Herrmann TR, Bach T, Imkamp F, Georgiou A et al (2010) Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol 28(1):45–51
Iacono F, Prezioso D, Di Lauro G et al (2012) Efficacy and safety profile of a novel technique, ThuLEP (Thulium laser enucleation of the prostate) for the treatment of benign prostate hypertrophy. Our experience on 148 patients. BMC Surg 12(Suppl 1):S21
Rausch S, Heider T, Bedke J et al (2015) Analysis of early morbidity and functional outcome of thulium: yttrium-aluminum-garnet laser enucleation for benign prostate enlargement: patient age and prostate size determine adverse surgical outcome. Urology 85(1):182–188
Shao Q, Zhang FB, Shang DH, Tian Y (2009) Comparison of holmium and thulium laser in transurethral enucleation of the prostate. Zhonghua Nan Ke Xue 15(4):346–349
Zhang F, Shao Q, Herrmann TR, Tian Y, Zhang Y (2012) Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology 79(4):869–874
Świniarski PP, Stępień S, Dudzic W et al (2012) Thulium laser enucleation of the prostate (TmLEP) vs. transurethral resection of the prostate (TURP): evaluation of early results. Cent European J Urol 65(3):130–134
Hochreiter WW, Thalmann GN, Burkhard FC et al (2002) Holmium laser enucleation of the prostate combined with electrocautery resection: the mushroom technique. J Urol 168:1470–1474
Tinmouth WW, Habib E, Kim SC et al (2005) Change in serum prostate specific antigen concentration after holmium laser enucleation of the prostate: a marker for completeness of adenoma resection? J Endourol 19(5):550–554
Gomez Sancha F, Rivera VC et al (2014) Common trend: move to enucleation—is there a case for GreenLight enucleation? Development and description of the technique. World J Urol [Epub ahead of print]
Cornu JN, Ahyai S, Bachmann A et al (2014) A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. doi:10.1016/j.eururo.2014.06.017
Conflict of interest
Authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Iason Kyriazis and Piotr P. Świniarski have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kyriazis, I., Świniarski, P.P., Jutzi, S. et al. Transurethral anatomical enucleation of the prostate with Tm:YAG support (ThuLEP): review of the literature on a novel surgical approach in the management of benign prostatic enlargement. World J Urol 33, 525–530 (2015). https://doi.org/10.1007/s00345-015-1529-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1529-0