Abstract
Purpose
Recent studies have expanded the concept that the systemic inflammatory response has an important role in the progression of several solid tumors. The neutrophil-to-lymphocyte ratio (NLR), an easily determinable marker of systemic inflammation, has been associated with clinical outcome in various cancer entities. In the present study, we validated the prognostic relevance of an elevated NLR in a cohort of European prostate cancer patients.
Methods
Data from 415 consecutive prostate cancer patients treated with 3D conformal radiotherapy at a single tertiary academic center from 1999 to 2007 were included in this retrospective study. Clinical progression-free survival (PFS), distant metastases-free survival (DMFS), and overall survival (OS) were assessed using the Kaplan–Meier method. To evaluate the prognostic relevance, univariate and multivariate Cox regression models were performed for each end point.
Results
Based on previously published studies, an NLR ≥ 5 was selected as cutoff value for external validation. Multivariate analysis identified an increased NLR as an independent prognostic factor for clinical PFS [hazard ratio (HR) 3.09, 95 % CI 1.64–5.82, p < 0.001], DMFS (HR 3.51, 95 % CI 1.80–6.85, p < 0.001), and OS (HR 2.16, 95 % CI 1.17–3.99, p = 0.013).
Conclusion
The NLR seems to represent an independent prognostic marker and should be considered for future individual risk assessment in patients with prostate cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, many efforts have been undertaken to identify novel immunological and histological prognostic markers in order to improve the prediction of the risk of prostate cancer recurrence. Although several potential molecular and cellular prognostic biomarkers have been detected, their widespread routine application has not yet been established due to lack of standardization and regional availability [1, 2].
Tumor progression and metastasization comprise a cascade of steps that involve the interaction between the tumor and the host-derived stromal microenvironment, which includes factors that support angiogenesis and inflammation [3, 4]. Recent studies have shown that the systemic inflammatory response which is usually measured by surrogate blood-based parameters, such as C-reactive protein or circulating inflammatory blood cells, has an important role in the progression of several solid tumors [4–7]. Of these inflammatory parameters, an increased neutrophil-to-lymphocyte ratio (NLR) has been proposed as an easily accessible and reliable marker to predict cancer patients’ survival [8–11].
Cumulating evidence suggests that a high NLR might represent an independent adverse prognostic factor in docetaxel-treated [12–14], abiraterone-treated [15], as well as in ketoconazole-treated [16] patients with metastatic castration-resistant prostate cancer (mCRPC).
In addition, the results of the Glasgow Inflammation Outcome Study demonstrated that an increased NLR had prognostic value in different types of cancer including localized prostate cancer [8, 17]. However, the study included a rather heterogeneous population of prostate cancer patients, and external validation of the NLR as a prognostic risk assessment tool in an independent cohort of prostate cancer patients has not yet been performed.
Therefore, the aim of the present study was to assess the prognostic significance of the pre-treatment NLR in a large cohort of European prostate cancer patients.
Methods
This retrospective study included data from 415 consecutive patients with histologically confirmed adenocarcinoma of the prostate treated at the Comprehensive Cancer Center Graz, Department of Therapeutic Radiology and Oncology, between 1999 and 2007. Eligible for inclusion in the present analysis were male patients with histologically confirmed prostate cancers who had neutrophil and lymphocyte counts recorded for any reason and underwent radiation therapy for prostate cancer.
Data on clinical characteristics including prostate specific antigen (PSA) at the time of diagnosis, tumor node metastasis (TNM) stage, histological grade, age at diagnosis, and family history were retrieved from electronic patient records of our institution. Prostate cancer patients were stratified into low-, intermediate-, and high-risk groups on the basis of pre-treatment PSA level, Gleason score (GS), and American Joint Commission on Cancer T stage. The patients were classified as high risk if they met any of the following criteria: T3–4, GS 8–10, or PSA > 20 ng/ml. The intermediate-risk group included stages T2b-2c, GS 7, or PSA 10–20 ng/ml; the low-risk group contained stages T1–T2a, GS ≤ 6, and PSA < 10 ng/ml.
Laboratory data, including neutrophil and lymphocyte counts, were obtained as part of routine clinical evaluation using standard clinical testing methodology.
Patients were treated with three-dimensional conformal radiation therapy using high-energy photons (18 MV) to a total dose of 70 Gy delivered in 1.8–2.0 Gy per fraction. A total of 277 patients (66.7 %) received additional neo-adjuvant and/or adjuvant androgen deprivation therapy (ADT).
Follow-up examinations included PSA measurements and digital rectal examinations (3-month interval in years 1–3, 6-month interval in years 4–5, and 12-month interval in years 6–15 after diagnosis). Patients with PSA relapse, defined as a rise by ≥2 ng/ml above the nadir PSA, were regularly checked through diagnostic tests, comprising isotope bone scan, chest X-ray, and abdominal and pelvic computed tomography as well as magnetic resonance imaging studies to detect local recurrences and/or distant metastases.
Statistical analyses
The primary end point of the study was clinical progression-free survival (PFS) which was defined as the time from prostate cancer diagnosis to the occurrence of local recurrence and/or distant metastases. The secondary end points included distant metastases-free survival (DMFS) defined as the time between diagnosis and the occurrence of distant metastases and overall survival (OS) calculated from time of diagnoses to the date of death of any cause. The NLR was calculated as the absolute neutrophil count measured in G/l divided by the absolute lymphocyte count measured in G/l. According to previously published studies, an NLR ≥ 5 was selected as cutoff value for external validation [8, 17]. The NLR was correlated with the clinicopathological features by nonparametric tests. To analyze the association between the clinicopathological features and the NLR with clinical PFS, DMFS, and OS, we generated Kaplan–Meier curves and compared them by the log-rank test. Furthermore, the association of individual variables with clinical PFS, DMFS, and OS was assessed using Cox proportional hazards models. To determine the independent effect of the NLR on the study end points, multivariate Cox proportional hazards models including age at diagnosis, androgen deprivation therapy, and risk group were used. Hazard ratios (HRs) estimated from the Cox analysis were reported as relative risks with corresponding 95 % confidence intervals (CIs). All statistical analyses were performed using the Statistical Package for Social Sciences version 22.0 (SPSS Inc., Chicago, IL, USA). A two-sided p ≤ 0.05 was considered statistically significant.
Results
Baseline patient and tumor characteristics are shown in Table 1. The median age at time of diagnosis was 68.2 years (mean 69.9 ± 7.2 years). The median follow-up time was 87 months (95 % CI 82–92 months). None of the clinicopathological features were associated with the NLR (data not shown).
In our study cohort, we found a significant association of age, PSA level at initial diagnosis, tumor stage, Gleason score, risk group, and (neo-) adjuvant ADT with clinical PFS, and DMFS; furthermore, a significant association between intermediate-risk situation and OS was observed (Table 1). Since risk group derives from tumor stage, Gleason score, and PSA level at time of diagnosis, only risk group, age at diagnosis, and additional androgen deprivation treatment were included in further multivariate models.
Based on previous studies, an NLR cutoff value of 5 was applied to differentiate between a low (<5) and high (≥5) NLR. Overall, there were 350 patients (84.3 %) with a low NLR and 65 patients (15.7 %) with a high NLR. A high NLR ≥ 5 significantly correlated with high neutrophil counts (p < 0.001) as well as with low lymphocyte counts (p < 0.001).
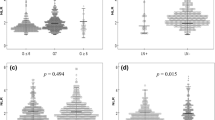
Of the 415 prostate cancer patients, 64 (15.4 %) developed local and/or distant tumor recurrence, 53 patients (12.8 %) developed distant metastases, and 60 (14.5 %) died within the follow-up period. Kaplan–Meier analyses show a significant association between an NLR ≥ 5 and decreased clinical PFS (p = 0.020, log-rank test; Fig. 1), DMFS (p = 0.015, log-rank test; Fig. 2), and OS (p = 0.011, log-rank test; Fig. 3).
In univariate analysis, the elevated NLR was significantly associated with decreased clinical PFS (HR 2.01, 95 % CI 1.10–3.67, p = 0.023; Table 1) that remained significant in the multivariate analysis (HR 3.09, 95 % CI 1.64–5.82, p < 0.001; Table 2). In a total of 212 patients (51.1 %), information on C-reactive protein (CRP) levels was available. After inclusion of CRP levels in our multivariate analysis in this subgroup of patients, the NLR ≥ 5 remained a significant predictor of clinical PFS (HR 2.86, 95 % CI 1.20–6.82, p = 0.018). Furthermore, we evaluated the combined effect of the NLR and GS on clinical PFS. For this analysis, patients were stratified into 4 groups on the basis of the NLR and GS as follows: GS < 7 and NLR < 5, GS < 7 and NLR ≥ 5, GS ≥ 7 and NLR < 5, and GS ≥ 7 and NLR ≥ 5. Patients with GS ≥ 7 and NLR ≥ 5 had a significantly shorter clinical PFS when compared to patients with GS < 7 and NLR < 5 (p < 0.001), GS < 7 and NLR ≥ 5 (p = 0.002), and GS ≥ 7 and NLR < 5 (p = 0.004, log-rank test; Fig. 4).
In DMFS analysis, we detected a significant correlation of an elevated NLR with decreased DMFS in univariate (HR 2.13, 95 % CI 1.14–4.00, p = 0.018; Table 1) and in multivariate analysis (HR 3.51, 95 % CI 1.80–6.85, p < 0.001; Table 2). In addition, the elevated NLR was significantly associated with decreased OS in univariate analysis (HR 2.10, 95 % CI 1.17–3.78, p = 0.013; Table 1) and multivariate analysis (HR 2.16, 95 % CI 1.17–3.99, p = 0.013, Table 2).
Subgroup analysis revealed a significant association between an elevated NLR and clinical PFS in intermediate-risk patients (HR 7.91, 95 % CI 1.57–39.7, p = 0.012) and high-risk patients (HR 2.61, 95 % CI 1.25–5.42, p = 0.010) after adjustment for age at diagnosis and additional androgen deprivation therapy.
Discussion
The present study was performed to validate the prognostic role of the NLR in patients with prostate cancer and demonstrated a significant association between an elevated NLR and poor clinical PFS, DMFS, and OS. The association with poor clinical outcome was independent of patient age, additional androgen deprivation therapy, and risk group that is based on tumor stage, Gleason score, and PSA level at diagnosis.
The NLR represents a marker of host inflammation that can easily be derived from the differential blood count. An elevation of the NLR may reflect both an elevated neutrophil-dependent inflammatory reaction and a lower lymphocyte-mediated antitumor immune response.
Neutrophils have been shown to promote tumor growth and metastasis by remodeling the extracellular matrix and releasing reactive oxygen species (ROS), nitric oxide (NO), and arginase which suppress the cytolytic activity of immune cells and increase the rate of mutagenesis [18–20]. In prostate cancer, tumor-associated neutrophils have been shown to contribute to enhanced angiogenesis and tumor cell intravasation by releasing matrix metalloproteinase-9 [25]. Additionally, circulating neutrophils have been found to produce inflammatory mediators, such as tumor necrosis factor, interleukin (IL)-1, and IL-6, which promote cancer cell proliferation and survival and angiogenesis [21].
Lymphocytes play a major role in cancer immune surveillance, which inhibits tumor cell proliferation and metastasization [22]. The importance of lymphocytes has been demonstrated in several studies in which an increased infiltration of tumors with lymphocytes has been associated with better prognosis in cancer patients [23]. Additionally, elevated circulating lymphocyte counts have been linked with prolonged survival in different types of cancer, and normalization of an initial lymphocytopenia has been associated with an improved clinical outcome [24–26].
A combined index using neutrophil and lymphocyte counts likely reflects a more aggressive behavior of tumors and has already been shown to predict prognosis in several studies for different solid tumors [8–17, 27]. Keizman et al. [16] found that an NLR > 3 is associated with a worse response rate and shorter PFS interval in patients with mCRPC treated with ketoconazole. A high NLR has also been shown to represent an independent poor prognostic marker in patients with mCRPC undergoing docetaxel therapy [12, 14]. Additionally, Leibowitz-Amit et al. [15] have demonstrated a significant role of an NLR > 5 in predicting response to abiraterone acetate and decreased OS in patients with mCRPC.
However, data on the role of the NLR in patients with non-metastatic prostate cancer are sparse. In the Glasgow Inflammation Outcome Study, 897 prostate cancer patients, who had a blood sample taken within a period of 2 years before or after prostate cancer diagnosis, were included and followed over a median time of 2.5 years [17]. Individuals that showed an elevated NLR of ≥5 measured within 2 years after initial diagnosis of prostate cancer had a higher risk of mortality. However, the study cohort comprised a rather heterogeneous patient population including localized and metastatic prostate cancer patients. Furthermore, information on treatment characteristics and other important prognostic factors such as disease stage and PSA level at diagnosis was not provided.
The present study was performed to externally validate the prognostic role of the pre-published NLR cutoff value of 5 and revealed a statistically significant association between NLR ≥ 5 and decreased PFS, DMFS, and OS in both univariate and multivariate analyses. Major strengths are the well-defined study cohort and the inclusion of information on treatment and important measures of prognosis such as tumor stage and PSA level.
Our study is not without limitations. Because of its retrospective design, we are unable to exclude the possibility of an unequal distribution of unidentified clinicopathologic parameters in our patient cohort that may have biased the observed results.
Furthermore, the present study included patients with NLR determined prior to the start of radiotherapy or neo-adjuvant ADT that might have caused changes in NLR. As the analysis of the NLR before, during, and after therapy was originally beyond the scope of our analysis, we were unfortunately not able to provide data concerning the influence of treatment on the NLR.
In addition, neutrophil and lymphocyte counts may be influenced by concurrent infection and drugs, which we could not account for in this analysis. Concurrent inflammatory diseases may underlie the increased overall mortality we observed in our cohort of prostate cancer patients with an increased NLR; however, a major effect on clinical PFS and DMFS is unlikely suggesting that an elevated NLR may independently influence prostate cancer prognosis and may serve as a cost-effective, readily available marker in daily clinical practice to guide individualized treatment decisions in prostate cancer patients.
References
Castelli T, Cimino S, Magno C, Morgia G (2010) Molecular markers for prostatic cancer. Front Biosci (Elite Ed) 2:641–656
Huang HC, Zheng S, VanBuren V, Zhao Z (2010) Discovering disease-specific biomarker genes for cancer diagnosis and prognosis. Technol Cancer Res Treat 9:219–230
Balkwill F, Mantovani A (2001) Inflammation and cancer: Back to Virchow? Lancet 357:539–545
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444. doi:10.1038/nature07205
Szkandera J, Gerger A, Liegl-Atzwanger B, Absenger G, Stotz M, Samonigg H, Maurer-Ertl W, Stojakovic T, Ploner F, Leithner A, Pichler M (2013) Validation of the prognostic relevance of plasma C-reactive protein levels in soft-tissue sarcoma patients. Br J Cancer. doi:10.1038/bjc.2013.595
Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, Kapp KS, Langsenlehner T (2014) The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer 110:2524–2530. doi:10.1038/bjc.2014.163
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O'Reilly DS, Foulis AK, Horgan PG, McMillan DC (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47:2633–2641. doi:10.1016/j.ejca.2011.03.028
Stotz M, Gerger A, Eisner F, Szkandera J, Loibner H, Ress AL, Kornprat P, AlZoughbi W, Seggewies FS, Lackner C, Stojakovic T, Samonigg H, Hoefler G, Pichler M (2013) Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br J Cancer 109:416–421. doi:10.1038/bjc.2013.332
Pichler M, Hutterer GC, Stoeckigt C, Chromecki TF, Stojakovic T, Golbeck S, Eberhard K, Gerger A, Mannweiler S, Pummer K, Zigeuner R (2013) Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer 108:901–907. doi:10.1038/bjc.2013.28
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, Leibowitz-Amit R, Sonpavde G, Knox JJ, Tran B, Tannock IF, Amir E (2014) Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst 106:dju124. doi:10.1093/jnci/dju124
Nuhn P, Vaghasia AM, Goyal J, Zhou XC, Carducci MA, Eisenberger MA, Antonarakis ES (2013) Association of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxel. BJU Int. doi:10.1111/bju.12531
Templeton AJ, Pezaro C, Omlin A, McNamara MG, Leibowitz-Amit R, Vera-Badillo FE, Attard G, de Bono JS, Tannock IF, Amir E (2014) Simple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratio. Cancer. doi:10.1002/cncr.28890
Sümbül AT, Sezer A, Abalı H, Köse F, Gültepe I, Mertsoylu H, Muallaoğlu S, Ozyılkan O (2014) Neutrophil-to-lymphocyte ratio predicts PSA response, but not outcomes in patients with castration-resistant prostate cancer treated with docetaxel. Int Urol Nephrol 46:1531–1535. doi:10.1007/s11255-014-0664-7
Leibowitz-Amit R, Templeton AJ, Omlin A, Pezaro C, Atenafu EG, Keizman D, Vera-Badillo F, Seah JA, Attard G, Knox JJ, Sridhar SS, Tannock IF, de Bono JS, Joshua AM (2014) Clinical variables associated with PSA response to abiraterone acetate in patients with metastatic castration-resistant prostate cancer. Ann Oncol 25:657–662. doi:10.1093/annonc/mdt581
Keizman D, Gottfried M, Ish-Shalom M, Maimon N, Peer A, Neumann A, Rosenbaum E, Kovel S, Pili R, Sinibaldi V, Carducci MA, Hammers H, Eisenberger MA, Sella A (2012) Pretreatment neutrophil-to-lymphocyte ratio in metastatic castration-resistant prostate cancer patients treated with ketoconazole: association with outcome and predictive nomogram. Oncologist 17:1508–1514. doi:10.1634/theoncologist.2012-0125
Shafique K, Proctor MJ, McMillan DC, Qureshi K, Leung H, Morrison DS (2012) Systemic inflammation and survival of patients with prostate cancer: evidence from the Glasgow Inflammation Outcome Study. Prostate Cancer Prostatic Dis 15:195–201. doi:10.1038/pcan.2011.60
De Larco JE, Wuertz BRK, Furcht LT (2004) The potential role of neutrophils in promoting the metastatic phenotype of tumors releasing interleukin-8. Clin Cancer Res 10:4895–4900
Rodriguez PC, Ernstoff MS, Hernandez C, Atkins M, Zabaleta J, Sierra R, Ochoa AC (2009) Arginase I-producing myeloid-derived suppressor cells in renal cell carcinoma are a subpopulation of activated granulocytes. Cancer Res 69:1553–1560
Müller I, Munder M, Kropf P, Hänsch GM (2009) Polymorphonuclear neutrophils and T lymphocytes: Strange bedfellows or brothers in arms? Trends Immunol 30:522–530
An X, Ding PR, Li YH, Wang FH, Shi YX, Wang ZQ, He YJ, Xu RH, Jiang WQ (2010) Elevated neutrophil to lymphocyte ratio predicts survival in advanced pancreatic cancer. Biomarkers 15:516–522
Vesely MD, Schreiber RD (2013) Cancer immunoediting: antigens, mechanisms, and implications to cancer immunotherapy. Ann N Y Acad Sci 1284:1–5
Gooden MJ, de Bock GH, Leffers N, Daemen T, Nijman HW (2011) The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer 105:93–103
Ege H, Gertz MA, Markovic SN, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Porrata LF (2008) Prediction of survival using absolute lymphocyte count for newly diagnosed patients with multiple myeloma: a retrospective study. Br J Haematol 141:792–798
Leitch EF, Chakrabarti M, Crozier JE, McKee RF, Anderson JH, Horgan PG, McMillan DC (2007) Comparison of the prognostic value of selected markers of the systemic inflammatory response in patients with colorectal cancer. Br J Cancer 97:1266–1270
Nieto Y, Nawaz S, Shpall EJ, Bearman SI, Murphy J, Jones RB (2004) Long-term analysis and prospective validation of a prognostic model for patients with high-risk primary breast cancer receiving high-dose chemotherapy. Clin Cancer Res 10:2609–2617
Sonpavde G, Pond GR, Armstrong AJ, Clarke SJ, Vardy JL, Templeton AJ, Wang SL, Paolini J, Chen I, Chow-Maneval E, Lechuga M, Smith MR, Michaelson MD (2014) Prognostic Impact of the neutrophil-to-lymphocyte ratio in men with metastatic castration-resistant prostate cancer. Clin Genitourin Cancer 12:317–324. doi:10.1016/j.clgc.2014.03.005
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The study was complied with the Declaration of Helsinki and has been approved by the local Ethical Committee (EK 27-032 ex 14/15). As this is a retrospective nonintervention study, the institutional review board waived the need for written informed consent from the participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Langsenlehner, T., Thurner, EM., Krenn-Pilko, S. et al. Validation of the neutrophil-to-lymphocyte ratio as a prognostic factor in a cohort of European prostate cancer patients. World J Urol 33, 1661–1667 (2015). https://doi.org/10.1007/s00345-015-1494-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1494-7