Abstract
Purpose
To assess the impact of dutasteride compared with placebo on nocturia in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia, using pooled data from dutasteride phase III studies.
Methods
Nocturia was assessed using Question 7 of the International Prostate Symptom Score questionnaire. Efficacy measures included: mean change in nocturia at 24 months; proportion of patients with improvement/worsening in nocturia; nocturnal voiding frequency at baseline and study end, overall and by baseline subgroups; and nocturnal voiding frequency <2 at study end in patients with baseline score ≥2.
Results
In total, 4,321 patients with a mean age of 66 years were evaluated. From month 12 onwards, mean nocturia improvements were significantly superior with dutasteride than with placebo (p ≤ 0.05). Reduction in nocturia was significantly better with dutasteride than with placebo across all baseline subgroups tested (p ≤ 0.05). Also at month 24, dutasteride therapy resulted in a greater proportion of subjects with nocturia improvement compared with placebo (p ≤ 0.05), with the largest treatment group differences in subjects with a baseline nocturia score of 2 or 3. Among patients with significant nocturia at baseline (score ≥2), significantly more subjects with dutasteride versus placebo had a score <2 at month 24 (26 vs. 19 %, p < 0.001).
Conclusions
After 24 months of treatment, dutasteride treatment provided significantly greater improvements in nocturia, and less worsening, compared with placebo, primarily in subjects with two or three nocturia episodes per night. Studies specifically designed to assess nocturia are required to prospectively confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Continence Society (ICS) defines nocturia as the complaint that an individual wakes at least once at night to void [1]. Frequently voiding twice or more per night can have a substantial impact on an individual’s quality of life (QoL), with sleep disruption leading to chronic fatigue [2, 3]. In addition, nocturia is associated with an increased risk of falls and fractures, as well as mortality [4, 5].
Nocturia is one of the most frequently reported and bothersome symptoms for patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH) [2, 3, 6]. Options for the medical management of LUTS/BPH include 5α-reductase inhibitors (5ARIs), either as monotherapy or in combination with α1-adrenoceptor antagonists (α1-blockers) [7]. Two 5ARIs are currently available for clinical use, finasteride and dutasteride. A 2010 systematic review reported that finasteride did not significantly reduce nocturia compared with placebo and that α1-blockers were significantly better than finasteride for improving nocturia [8]. Dutasteride is a 5ARI that has been shown in phase III studies to significantly improve LUTS/BPH [9, 10]. However, data on the impact of dutasteride on nocturia are limited. Here, we assess the impact of dutasteride on nocturia using Question 7 of the International Prostate Symptom Score (IPSS) and pooled data from 2-year phase III studies.
Patients and methods
Study designs and patient population
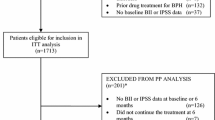
The dutasteride phase III programme consisted of three identical, randomised studies (ARIA3001, ARIA3002, ARIA3003) comparing dutasteride 0.5 mg (n = 2167) with placebo (n = 2,158); study designs were reported in detail previously [9]. Subjects eligible for inclusion in the trials were men aged ≥50 years with a confirmed clinical diagnosis of ‘BPH’, an IPSS ≥12, prostate volume ≥30 cc, PSA 1.5–10 ng/ml, a maximum urinary flow rate (Q max) ≤15 ml/s, and a minimum voided volume of ≥125 ml. Men with use of an α-blocker within 4 weeks of study start, or any prior use of a 5ARI, were excluded.
Assessments and statistical analysis
The prevalence of nocturia was assessed with Question 7 of the IPSS, which asks: During the last month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning? Responses range from 0 to 5, as follows: none (0), 1 time (1), 2 times (2), 3 times (3), 4 times (4), 5 or more times (5).
Dutasteride was compared with placebo for the following: mean changes in nocturia over time up to study end (24 months) using a generalised linear model; the proportion of patients with improvement or worsening (decrease/increase of ≥1 unit score) in nocturia (Fisher’s exact test), using the last observation carried forward (LOCF) approach; nocturnal voiding frequency at baseline and study end (24 months), overall and by various baseline subgroups (t tests from the general linear model), using the LOCF approach; and nocturnal voiding frequency <2 at study end in those patients with a baseline nocturia score ≥2 (Fisher’s exact test), using the LOCF approach. Statistical significance was defined as p ≤ 0.05. Safety data from these studies have been reported previously [9, 10].
Results
Patient demographics and baseline characteristics
In total, 4321 patients had an IPSS Question 7 score at baseline. Mean (SD) IPSS Question 7 score at baseline was 2.4 (1.21) in the dutasteride group and 2.4 (1.23) in the placebo group. Patient demographics and baseline characteristics across each IPSS Question 7 score category are shown in Table 1. Overall IPSS score rose according to increasing severity of nocturia, with a trend for increasing BPH Impact Index (BII) and decreasing Q max.
The majority of patients in each treatment group (79–80 %) had an IPSS Question 7 score of 1–3; 18 % patients had a score of 4 or 5 (Fig. 1). Only 2–3 % of patients were free of nocturia at baseline. The proportion of patients with a baseline IPSS Question 7 score of ≥2 was 77 % in the dutasteride group and 75 % in the placebo group.
Improvements in nocturia
From month 12 onwards, mean improvements in nocturia were significantly superior (p ≤ 0.05) with dutasteride than with placebo (Fig. 2). At month 24, the mean (SD) IPSS Question 7 score was 2.1 (1.25) in the dutasteride group and 2.3 (1.24) in the placebo group (adjusted mean change from baseline was −0.28 in the dutasteride group and −0.11 in the placebo group; mean treatment difference −0.17, 95 % CI −0.24 to −0.10). Also at month 24, dutasteride therapy resulted in a greater proportion of subjects with nocturia improvement compared with placebo treatment (p ≤ 0.05), with the largest treatment group differences noted in subjects with a baseline nocturia score of 2 or 3 (Table 2). Among those with significant nocturia at baseline (score ≥2), 48 and 40 % of patients in the dutasteride and placebo groups, respectively, showed improvement at month 24 (p < 0.001). Also in this subgroup, significantly more subjects in the dutasteride group than in the placebo group had a score of <2 at month 24 (26 vs. 19 %, p < 0.001).
Worsening/no change of nocturia
Compared with placebo (26 %), dutasteride therapy (21 %) resulted in a significantly smaller (p ≤ 0.05) proportion of patients with worsening of nocturia (Table 2). The proportion of patients who experienced ‘no change’ of nocturia symptoms was numerically greater (p = 0.40) in the dutasteride group (43 %) than in the placebo group (41 %).
Treatment impact on nocturia score by baseline subgroups
At month 24, reduction in nocturia score was significantly better (p ≤ 0.05) with dutasteride than with placebo across all baseline subgroups tested (Fig. 3).
Discussion
These post hoc analyses indicate that the 5ARI, dutasteride, was superior to placebo for improving nocturia. Improvements were observed in the overall pooled population as well as in each baseline subgroup tested. In addition, more patients experienced improvement and fewer experienced worsening with dutasteride across the range of baseline IPSS Q7 scores.
These analyses show for the first time a small but significant benefit for dutasteride compared with placebo for improving nocturia, as assessed by the IPSS Question 7. Improvement in nocturia with dutasteride relative to placebo has been indicated in an earlier analysis of the dutasteride phase III studies [11]; this pooled data analysis showed a small but statistically significant improvement in nocturia as assessed by Question 3 of the Symptom Problem Index (‘Has getting up at night to urinate been a problem for you?’). However, other studies involving finasteride have not shown nocturia improvement relative to placebo [12, 13]. A post hoc analysis of randomised data comparing the plant extract PRO 160/120 and finasteride (see this journal issue) showed no significant difference between the treatments for effects on nocturnal voiding frequency [14].
The net improvement with dutasteride in our analyses was <0.3 episodes per night in the overall pooled population and <0.3 episodes per night in the various baseline subgroups. Although the differences between dutasteride and placebo were statistically significant, the differences between the two groups were small. Therefore, the clinical benefit of dutasteride on nocturia reduction in the overall population of LUTS/BPH patients is likely to be relatively modest. However, some patients experienced substantial improvements in nocturia, and 35 % of men in the dutasteride group had a nocturia score of 0 or 1 at the end of the study (29 % of the placebo group; data not shown).
The net improvement with dutasteride over placebo we report is similar to that observed for the α-blocker silodosin [15] and the PDE-5 inhibitor tadalafil [16] in post hoc analyses of placebo-controlled trials (see this journal issue). Also in this issue, combination therapy with dutasteride plus tamsulosin was shown to be significantly superior to either monotherapy in a post hoc analysis of effects on nocturia using data from the CombAT study [17].
Among subjects with a baseline IPSS Question 7 score ≥2, a significantly greater proportion of men treated with dutasteride reported improvement at the end of the study compared with those who received placebo. Also, significantly more of these patients who were treated with dutasteride had a score of <2 at study end compared with placebo. Waking to void twice or more per night can result in substantial QoL impairment [6, 18]. Therefore, patients who achieve <2 voids per night are likely to have less bother from nocturia and improved QoL.
The post hoc nature of the analyses represents a limitation of the data presented. An additional limitation is that nocturia was assessed using IPSS Question 7, rather than through voiding diaries (as recommended by the ICS); as a result, nocturnal polyuria or other urological and non-urological causes of nocturia could not be excluded. Future studies should therefore include voiding diaries and pressure flow analysis to determine the precise origin of nocturia. Also, use of the IPSS Q7 meant that it was not possible to assess the impact of the observed improvement with dutasteride on patients’ bother and QoL.
Conclusions
After 24 months, treatment with dutasteride provided significantly greater improvements in nocturia, and less worsening, compared with placebo, primarily in subjects with 2 or 3 nocturia episodes per night. Further studies, specifically designed to assess nocturia, are required to prospectively confirm these findings, and to assess the ultimate benefits for QoL and other outcomes associated with nocturia.
References
Abrams P, Cardozo L, Fall M et al (2002) The standardization of terminology in lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
Schulman CC, Asplund R, Desgrandchamps F, Jonas U (2005) The impact of nocturia on health status and quality of life in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH). Eur Urol Suppl 4:1–8
van Dijk MM, Wijkstra H, Debruyne FM, de La Rosette JJ, Michel MC (2009) The role of nocturia in the quality of life of men with lower urinary tract symptoms. BJU Int 105:1141–1146
Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC (2011) Association of nocturia and mortality: results from the Third National Health and nutrition Examination Survey. J Urol 185:571–577
Galizia G, Langellotto A, Cacciatore F et al (2012) Association between nocturia and fall-related long-term mortality in the elderly. J Am Med Dir Assoc 13:640–644
Tikkinen KA, Johnson TM II, Tammela TL et al (2010) Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol 57:488–496
Oelke M, Bachman A, Descazeaud A et al (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64:118–140
Tacklind J, Fink HA, Macdonald R et al. (2010) Finasteride for benign prostatic hyperplasia. Cochrane Database Syst Rev, CD006015
Roehrborn CG, Boyle PJ, Nickel JC, Hoefner K, Andriole G (2002) Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology 60:434–441
Debruyne F, Barkin J, van Erps P, Reis M, Tammela TLJ (2004) Efficacy and safety of long-term treatment with the dual 5α-reductase inhibitor dutasteride in men with symptomatic benign prostatic hyperplasia. Eur Urol 46:488–495
O’Leary M, Roehrborn CG, Black L (2008) Dutasteride significantly improves quality of life measures in patients with enlarged prostates. Prostate Cancer Prostatic Dis 11:129–133
Johnson TM II, Jones K, Williford WO, Kutner MH, Issa MM, Lepor H (2003) Changes in nocturia from medical treatment of benign prostatic hyperplasia: secondary analysis of the Department of Veterans Affairs Co-operative Study trial. J Urol 170:145–148
Johnson TM 2nd, Burrows PK, Kusek JW et al (2007) The effect of doxazosin, finasteride and combination therapy on nocturia in men with benign prostatic hyperplasia. J Urol 178:2045–2051
Oelke M, Berges R, Schläfke S, Burkart M (2014) Fixed-dose combination PRO 160/120 of sabal and urtica extracts improves nocturia in men with LUTS suggestive of BPH: re-evaluation of four controlled clinical studies. World J Urol. doi:10.1007/s00345-014-1338-x
Eisenhardt A, Schneider T, Cruz F, Oelke M (2014) Consistent and significant improvement of nighttime voiding frequency (nocturia) with silodosin in men with LUTS suggestive of BPH: pooled analysis of three randomized, placebo-controlled, double-blind phase III studies. World J Urol. doi:10.1007/s00345-013-122-7
Oelke M, Weiss JP, Mamoulakis C, Cox D, Ruff D, Viktrup L (2014) Effects of tadalafil on night-time voiding (nocturia) in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia: analyses of pooled data from four randomized, placebo-controlled clinical studies. World J Urol. doi:10.1007/s00345-014-1255-z
Oelke M, Roehrborn CG, D’Ancona C, Wilson TH, Castro R, Manyak M (2014) Nocturia improvement in the Combination of Avodart® and Tamsulosin (CombAT) study. World J Urol. doi:10.1007/s00345-014-1296-3
Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E (2003) The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int 92:948–954
Acknowledgments
Medical writing support was provided by Tony Reardon of Spirit Medical Communications Ltd, funded by GlaxoSmithKline. The three studies on which these analyses were based were funded by GlaxoSmithKline.
Conflict of interest
Matthias Oelke has been a speaker, advisor and/or trial participant for Allergan, Apogepha, Astellas, Bayer, Ferring, GlaxoSmithKline, Lilly, Mundipharma, Pfizer and Recordati. Claus G. Roehrborn has been a speaker, advisor and/or trial participant for GlaxoSmithKline. Carlos D’Ancona has been a speaker and trial participant for GlaxoSmithKline and Astellas. Timothy H. Wilson, Ramiro Castro and Michael Manyak are employees of GlaxoSmithKline.
Ethical standard
The original dutasteride phase III studies were approved by the appropriate ethics committees and performed in accordance with the ethical standards defined by the 1964 Declaration of Helsinki and later amendments. All participants provided written informed consent prior to inclusion in the studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oelke, M., Roehrborn, C.G., D’Ancona, C. et al. Impact of dutasteride on nocturia in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH): a pooled analysis of three phase III studies. World J Urol 32, 1141–1147 (2014). https://doi.org/10.1007/s00345-014-1316-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1316-3