Abstract
Objectives
Bladder perforation is the second most common complication during transurethral resection of bladder tumours. It is unknown whether perforation affects the natural history of the tumour through cell seeding. The aim of this study was to study the impact of perforation on the oncologic outcomes of bladder carcinoma.
Materials and methods
Between 2003 and 2007, 926 consecutive patients underwent transurethral resection of bladder tumours at our institution; 327 cases were staged ≥pT2 and were treated immediately with cystectomy and/or multimodal therapy and therefore excluded from the study. An additional 34 cases without urothelial carcinoma were excluded. Of the remaining 565 patients with non-muscle invasive bladder cancer, 457 (80.8 %) were male and 108 (19.2 %) were female with a mean age of 69.5 years in men and 67.3 years in women. Thirty-seven patients (6.5 %) experienced bladder perforation at the time of tumour resection. This group of patients (Group 1) was compared to the remaining 528 patients (Group 2) who did not experience a bladder perforation.
Results
Patients with bladder wall perforation experienced a shorter disease-free survival in both univariate (p = 0.003) and multivariate analyses (p = 0.006). In addition, subsequent recurrences revealed stage progression of recurrent disease (p = 0.05) and trended to a higher number of cystectomies in the perforated group of patients (p = 0.06). Nevertheless, perforation did not appear to influence overall survival (p = 0.127) or cancer-specific survival (p = 0.141).
Conclusion
The results indicate that bladder perforation during resection of superficial bladder tumours is burdened by a shortened disease-free survival and T-stage progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The transurethral resection (TUR) is a standard urological procedure [1]. As bladder carcinoma (BC) is the second most common tumour of the genitourinary system, the TUR is a frequently performed intervention. Suspicious lesions within the bladder are resected, and importantly, underlying muscle is resected to allow for accurate pathological examination of the specimen [2]. Deep resection can result in bladder perforation (BP). The influence of BP on the natural history of the tumour is however unknown.
The most common complications are bleeding requiring transfusions in 3–13 %, perforation in 1––5 %, infection in up to 24 % and mortality in 1.3 % [3, 4]. One of the most significant complications is BP often associated with bleeding requiring transurethral revision and prolonged bladder drainage. An intraperitoneal perforation can lead to laparotomy, bladder repair and open drainage of the abdominal cavity. It is believed that the incidence of perforation correlates with the size and number of tumours, but not with tumour stage, grade or location of the tumours [3].
Theoretically, tumour cell seeding due to a BP could lead to subsequent disease recurrence and decreased survival. This occurrence is not well studied in the literature, and only a few case reports exist. Evaluating this data is difficult as surgical technique and recurrence rates vary widely [5], and perforations are not always recognized.
The aim of this study was to investigate the impact of BP on the natural history of BC following TUR.
Materials and methods
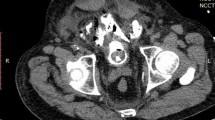
The BC database at our department includes the records of all consecutive patients with BC treated with TUR between March 2003 and November 2007. All procedures were done with video resection following the protocol publishing previously [1, 6]. A digital data sheet is filled in by the operating staff member. We prospectively recorded patient characteristics, risk factors, cystoscopic findings, number of previous TURs, number and location of resected BC, loop used, catheter used and intraoperative complications. Findings are also photographically documented as previously reported [6]. When the database was created, cases were either classified as controlled perforation by the surgeon or as an accidental perforation exceeding the required resection. When a BP was suspected due to symptoms such as peritoneal irrigation, increased abdominal girth and hypogastric pain, the patients underwent immediate cystography. Each patient’s data sheet was reviewed and updated prior to hospital discharge. All data were collected prospectively.
After discharge, the patients entered a routine follow-up programme as recommended [7]. The tumours were staged according to the 1992 International Union Against Cancer (UICC) [8] and WHO cell differentiation grade [9] classification criteria.
We evaluated disease-specific recurrence, overall survival (OS) and cancer-specific mortality (CSM) using univariate and multivariate analyses. Survival times were calculated from the day of TUR to the first recurrence (disease-free survival, DFS), to death (OS) and to cancer-related death (CSM). Cumulative recurrences over time were plotted as an inverse Kaplan–Meier curve. A p value <0.05 was considered statistically significant. The software package used for statistical analysis was the IBM SPSS v.17.0.1 (SPSS, Chicago, IL, USA).
Results
This study was approved by the institutional review board. Between March 2003 and November 2007, 926 consecutive patients underwent a TUR for BC; 327 cases were staged pT2 or higher and were treated immediately after TUR with cystectomy and/or multimodal therapy and therefore excluded from the study. An additional 34 patients without BC were also excluded; 565 patients had a superficial BC (NMIBC); 457 (80.8 %) were men and 108 (19.2 %) were women. The average age was 69.5 years (range 37–97) for males and 67.3 years (range 48–91) for females.
BP occurred in 37 cases (6.7 %), of which 31 were extraperitoneal and 6 intraperitoneal. Group 1 consisted of 37 patients with a documented BP. This included 10 (37 %) females and 27 (63 %) males with a mean age of 70.6 years (range 47–86). Group 2 consisted of the remaining 528 patients without a BP. This Group 2 was the control group and had an average age of 67.5 years (range 37–97). In Group 2, 97 (18.4 %) patients were women and 431 (81.6 %) men.
All perforations were recognized intraoperatively and confirmed by a cystography. In none of the cases was open surgery revision necessary. The bladder was drained with a 20 Fr transurethral catheter. In 36 out of 37 cases, the catheter was removed after 7 days following a negative cystography. In six cases (16 %), the BC was not completely resected at the initial TUR due to bleeding following the perforation. Once the bleeding was controlled, the TUR was aborted. Six weeks later, these 6 patients underwent a second TUR to completely remove any residual tumour.
In one case, a catheter malfunction leads to overdistension of the bladder and recurrent bleeding. This patient underwent endoscopical revision twice due to recurring bleeding. He received a total of 8 blood units and required intensive care observation for 6 days. The catheter was removed after 15 days.
In Group 1, Ta tumour was seen in 24 patients, T1 in 12 patients and carcinoma in situ (Cis) in 1 patient. The grading was as follows: 8 (21 %) G1 tumours, 22 (60 %) G2 tumours and 7 (19 %) G3 tumours. In the Group 2, 370 (70 %) patients had a Ta tumour, 135 (25 %) a T1 tumour and 23 (5 %) Cis; 199 (38 %) patients had a G1, 184 (35 %) a G2 and 145 (27 %) a G3 tumour. Staging and grading for both Group 1 and 2 are shown in Table 1.
All patients with an intermediate risk BC received a course of 7 instillations with 80 mg Farmarubicin at weekly intervals starting 21 days after the TUR. The high-risk group was treated with BCG with a 18-month maintenance schedule as recommended by the EAU [7] with similar completion rates in both groups (26/37; 70 vs 351/528; 66 %).
The mean patient follow-up was 69 months, with a median of 59 months and a range from 1 to 291 months. The recurrence rate was 62.1 % (23/37 patients) in Group 1 and 50 % (264/528) in Group 2. The progression rate in Group 1 was 21.6 % (8/37) and 16.8 % (89/528) in Group 2. These observed differences were not statistically significant. From the seven T-stage progressions in group 1, six were observed at the perforation site whereas the 7th was a multifocal recurrence which included also the perforation site. In order to evaluate whether the cumulative relapse rate varied in a time-dependent manner, we plotted it as an inverse Kaplan–Meier curve (Fig. 1). Patients with a bladder perforation had significantly earlier bladder tumour relapses than patients without a bladder perforation (p = 0.002). Recurrences in the perforation group also revealed a significant T-stage progression (p = 0.025). In addition, nine patients from Group 1 (24 %) underwent subsequent cystectomy, whereas the cystectomy rate was 13.2 % (70/528) in Group 2. This did not reach but trended towards statistical significance (p = 0.06).
In Group 1, the overall mortality (OAM) was 40.5 % (15/37) and the CSM was 10.8 % (4/37). In Group 2, OAM was 34 % (180/528) and CSM was 6 % (32/528) (Table 2). Five-year estimated OS and CSM were 56 % and 87 % in Group 1 and 74 % and 94 % in Group 2, respectively. These differences were not statistically significant (p = 0.127 and p = 0.141). Independent predictors for OS were grade and focality (p < 0.05). Only grade 3 was an independent predictor for CSM (p = 0.025).
In univariate analysis, perforation and focality emerged as significant prognosticators for DFS with a p value of 0.002 and 0.004, respectively. Instate OS was influenced by T-stage (p < 0.001), grade (p < 0.001) and focality (p = 0.001). CSM was significantly shorter with higher T-stage (p < 0.001) and higher grade (p < 0.001).
Multivariate Cox regression model revealed perforation (p = 0.042 HR = 1.699) for DFS, grade 3 (p = 0.001, HR = 2.493) for OS, T-stage (p = 0.038, HR = 2.789) and grade 3 (p = 0.0037, HR = 6.138) for CSM as significant predictors. Thus, perforation had a significant impact on DFS, independently from stage and grade but did affect neither OS nor CSM.
Discussion
The TUR of NMIBC pursues a double goal: first to remove the entire tumour burden and second to provide appropriate histopathological staging information [2]. The strategy of resection depends on the tumour size and location, but finally, a complete TUR is vital in achieving a correct diagnosis and accurate staging.
Even though TUR is frequently performed, it is not without risk of complications [10]. BP is the second most common complication, and it is a consequence of inadvertent full-thickness bladder wall resection. Very rare causes are involuntary perforation with the resectoscope itself or rupture of the bladder due to overdistension [8]. Most BP can be handled conservatively, and long-term consequences are thought to be negligible. In this series, however, we observed an increase in T-stage progression rate in patients suffering a BP (p < 0.05).
The higher recurrence rates following perforation observed in this series could be the result of either tumour implantation or tumour seeding at the time of perforation. Tumour cell seeding outside the bladder wall could potentially lead to inadvertent progression of a formerly low-grade and stage tumour. Evidence exists for tumour seeding with transitional cell carcinoma and there are several reports of peritoneal or abdominal wall metastases after a BP [11]. Most of these are anecdotal or small series. Mydlo et al. [12] retrospectively evaluated 11 BP cases. In one case (9 %), a peritoneal metastasis was noted 4 months after a TUR perforation of a pTa G2 tumour. Breul et al. [13] reported a case where 8 weeks following suprapubic tube removal and TUR, the patient developed an implantation metastasis at the site of the suprapubic tube. In the 1950’s, Melicow described various implantation metastases after suprapubic cystostomy, partial cystectomy and bladder biopsies [14]. In a series from Boreham, tumour implantation following TUR was 3.4 % [15]. In contrast, Nieder noted a perforation rate of 3.5 % following TUR without any subsequent tumour implantation [11].
The surgical spread of BC is yet not enough understood. The process of seeding/metastatization requires circulating tumour cells (CTC) which have to home in their target tissue, disengage the normal cell cluster, engage in their new environment and get in contact with the blood supply [16]. The systemic dissemination of single malignant cells from a tumour cell cluster represents an early essential step in the metastatic cascade of solid tumours. After the neoplastic transformation of epithelial cells, the loss of adhesion is a precondition for the development of an invasive growth. This process is named epithelial-mesenchymal transition (EMT). The secretion of proteases leads to a degradation of the basal membrane, and the tumour is able to penetrate the underlying tissue of the “host” [16]. Through the penetration of lymphatic vessels and the vasculature single tumour cells or tumour cell cluster join the circulation. This is called leukaemic phase and followed by the tumour cell “homing” [16]. In breast cancer, the detection of CTC is associated with an unfavourable prognosis [17]. Jonasson could show that during a TUR in 37.5 % of the cases, CTC are detectable in the peripheral blood [18] whereas Desgrandchamps could not find any CTC during TUR in 24 consecutive patients [19]. A TUR could potentially cut short the process of EMT pushing neoplastic cells into the circulation via simple pressure or micro perforations, but even more if the complete bladder wall is perforated and a substantial number of blood and lymphatic vessels are opened.
The second possibility to explain a higher recurrence rate following TUR with perforation is the possibility that an inadequate initial tumour resection was performed because of the perforation. If the tumour is not completely resected prior to the perforation, residual disease may be left behind that is not visualized secondary to bleeding or difficulties maintaining bladder distension. In our series, every patient suffering a BP prior to a complete resection was re-resected within 6 weeks to minimize this possibility.
We recognize the retrospective nature of this study, but to our knowledge, this is the first report where patients with a documented BP are compared to another cohort without BP. In our series, BP significantly affected DFS in both univariate (p = 0.003) and multivariate analyses (p = 0.006), with relapses occurring in 62 % of perforation cases and only 50 % of non-perforation cases resulting in a higher TUR rate in the Group 1 (Table 1). Perforation did not however influence OS (p = 0.074) or CSM (p = 0.194). In addition, we observed evidence for earlier relapses and T-stage progression in perforated patients, and these patients trended to more frequent rates of subsequent cystectomy (24 vs 13 %; p = 0.06).
As it is well documented that late recurrences are thought to be caused by genetic instability of the urothelium [20], the high rate of early relapses in the patients with BP in our series suggests the possibility of iatrogenic seeding of neoplastic cells. No impact on OS and CSM was observed in our cohort; however, most cystectomy is a very efficient salvage treatment and we would not expect a significant impact on OS and CSM for NMIBC. These trends in cystectomy rates could only be answered in a larger, multi-institutional study.
For the group of patients with NMIBC, our observations have significant implications. TUR should remove the entire tumour and provide adequate material for proper staging which is pivotal for tailored therapy and follow-up. At the same time, NMIBC has a favourable prognosis and therefore treatment should not have a negative impact. The results of this study suggest that BP at the time of TUR may adversely affect patient outcome and should be avoided. In addition, patients suffering a perforation should be considered at higher risk for recurrence and T-stage progression and should be monitored appropriately.
References
Pycha A, Palermo S (2007) How to teach the teacher to teach the TUR. Int J Surg 5(2):81–85
Babjuk M, Oosterlinck W, Sylvester R, Kaasinen E, Böhle A, Palou J (2008) Guidelines on TaT1 (non muscle invasive) bladder cancer. Eur Urol 54:303–314
Collado A, Chechile GE, Salvador J et al (2000) Early complications of endoscopic treatment for superficial bladder tumors. J Urol 164:1529–1532
Dick A, Barnes R, Hadley H et al (1980) Complications of transurethral resection of bladder tumors: prevention, recognition and treatment. J Urol 124:810–814
Kurth KH, Bouffioux C, Sylvester R, van der Meijden AP, Oosterlinck Brausi M (2000) Treatment of superficial bladder tumors: achievments and needs. The EORTC Genitourinary-Group. Eur Urol 37(Suppl 3):1–9
Pycha A, Palermo S (2005) Chapter: transurethral resection of bladder tumors. In: Hohenfellner R, Stolzenburg JU (eds) Manual endourology, 1st edn. Springer, New York
Oosterlinck W, Lobel B, Jackse G, Malmström PU, Stöckle M, Sternberg C (2002) Guidelines on bladder cancer. Eur Urol 41:105–112
Greene FL, Page DL, Fleming ID, et al (eds) (2002) In: AJCC cancer staging manual, 6th edn. Springer, New York, pp 335–340
Epstein JI, Amin MB, Reuter VR, Mostofi FK (1998) The world health organization/international society of urological pathology consensus classification of urothelial/transitional cell) neoplasm of the urinary bladder. Bladder consensus confewrence committee. Am J Surg Pathol 22(12):1435–1448
Traxer O, Pasqui F, Gattegno B, Pearle MS (2004) Technique and complications of transurethral surgery for bladder tumors. BJU Int 94:492–496
Nieder AM, Meinbacvh DS, Kim SS, Soloway MS (2005) Transurethral bladder tumor resection: intraoperative complications in a residency setting. J Urol 174:2307–2309
Mydlo JH, Weinstein R, Shah S, Solliday M, Macchia RJ (1999) Long term from bladder perforation and/or violation in the presence of transitional cell carcinoma: results of a small series and a review of the literature. J Urol 161:1128
Breul J, Block T, Breidenbach H, Hartung R (1992) Implantation metastasis after a suprapubic catheter in a case of bladder cancer. Eur Urol 22:86–88
Melicow MM (1955) Tumors of the urinary bladder: a clinico-pathological analysis of over 2500 specimens and biopsies. J Urol 74:498–521
Boreham P (1956) The surgical spread of cancer in urology. Br J Urol 28:163–175
Arya M, Bott SR, Shergill IS et al (2006) The metastatic cascade in prostate cancer. Surg Oncol 15:117–128
Schilling D, Todenhöfer T, Taran FA, Hartkopf A, Stenzl A, Fehm T (2011) Mechanism of tumour cell dissemination and methods for detection of circulating tumour cells in transitional cell carcinoma. Aktuelle Urol 42(2):122–127
Jonasson O, Long L, Roberts S, McGrew W, McDonald JH (1961) Cancer cells in the circulating blood during operative management of genitourinary tumors. J Urol 85:1–12
Desgrandchamps F, Teren M, Dal Cortivo L et al (1999) The effect of transurethral resection and cystoprostatectomy on dissemination of epithelial cells in the circulation of patients with bladder cancer. Br J Cancer 81:832–834
Pycha A, Mian Ch, Hofbauer J, Brössner C, Haitel A, Wiener H, Marberger M (1999) Multifocality of transitional cell carcinoma results from genetic instability of entire transitional epithelium. Urology 53:92–97
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Comploj, E., Dechet, C.B., Mian, M. et al. Perforation during TUR of bladder tumours influences the natural history of superficial bladder cancer. World J Urol 32, 1219–1223 (2014). https://doi.org/10.1007/s00345-013-1197-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1197-x