Abstract
Despite rapid decompression of the upper urinary tract, some patients show signs of systemic inflammatory response syndrome (SIRS) or septic shock syndrome when infected hydronephrosis is diagnosed. Clinical and biological parameters were analyzed retrospectively in 189 patients diagnosed with hydronephrosis regarding disease severity as well as microbiological and antibiotic features. Fifty of the 189 patients had positive urine culture in the renal pelvis and were included in the study. Fifteen patients had to be placed in the intensive care unit and two patients developed severe septic signs. An initial body temperature above 38.5°C (P=0.0004) and an elevated BMI (P=0.002) were the only parameters that indicated a higher risk of developing SIRS or sepsis. Typical biological parameters were not helpful in differentiating patients who will develop urosepsis. Further research is necessary to provide conclusive evidence of the value of other early prognostic markers in patients with infected hydronephrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly every woman experiences at least one urinary tract infection (UTI) during her lifetime [1]. There are close to 7 million UTIs in the USA annually with about 1 million requiring hospitalization [2]. The uncomplicated lower urinary tract infection requires antibiotic treatment, usually as a 3-day regimen with trimethoprin-sulfamethoxazole (TMP-SMX) or fluoroquinolones (ciprofloxacin). Fluoroquinolones have to be considered second line chemotherapeutic agents due to their high costs and unproven benefits in uncomplicated UTI [3, 4].
Complicated UTIs almost always involve the upper urinary tract. Common symptoms of infected urine in the renal pelvis are flank pain, fever and chills, which can be treated with TMP-SMX or fluoroquinolones over a period of 10–14 days. Recent studies have found treatment with fluoroquinolones to be superior to the 14-day TMP-SMX regimen [5].
Infected hydronephrosis due to obstruction with infected resting urine in the renal pelvis requires prompt decompression of the renal pelvis. Standard treatment is drainage either by ureteral stent or nephrostomy tube placement (PCN), which is introduced percutaneously under ultrasound guidance. The advantages and disadvantages of the two methods have been the topic of various studies [6–9]. Since both are thought to have the same clinical efficacy, the clinical course has thus far not been considered for predicting further disease development or resolution.
Urosepsis is a severe course of infected hydronephrosis, but patients with urosepsis usually have a much less severe course than those with a septic focus in the gastrointestinal or pulmonary tract [10]. Since the clinical symptoms of urosepsis are bacterial manifestations in urine and blood (bacteremia), in combination with other symptoms like hypoxemia, oliguria and hypotension, they may lead to multiple organ failure syndrome (MOFS). Therefore, it is imperative to differentiate between patients showing three of the symptoms like hyperthermia, tachypnea, tachycardia, and an elevated white blood count, the so-called septic inflammatory response syndrome (SIRS) and severe sepsis [11].
Some patients with infected hydronephrosis develop urosepsis despite rapid decompression of the infected renal pelvis. The aim of this investigation was to find clinical parameters that help to distinguish this group of patients. In addition, we evaluated the time until recovery and hospitalization as well as the microbiological pattern of bacteria causing the infection or urosepsis. Finally, we compared nephrostomy and ureteral stent placement for efficacy and the possible effect on the course of infected hydronephrosis.
Materials and methods
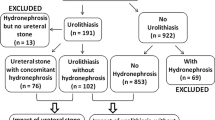
Data were collected retrospectively from 189 patients with hydronephrosis treated at one single institution between 1999 and 2002. The study has been approved by the appropriate ethics committee and is in accordance with the ethical standards of the Declaration of Helsinki. All patients gave informed consent prior to their inclusion in the study.
In the case of suspected infected hydronephrosis, rapid decompression of the collecting system was done by a urologist performing either nephrostomy tube or ureteral stent placement. The decision whether to insert a nephrostomy tube or ureteral stents was made individually by the treating physician. Radiographic imaging consisted of an initial ultrasound of the genitourinary tract and fluoroscopy during the procedure. Patients were followed up by monitoring body temperature, blood pressure and urinary output. We also monitored the white blood count, C-reactive protein levels and the time until normalization as well as the duration of hospitalization. Patients were transferred to the intensive care unit (ICU) if there were signs of SIRS or sepsis. Patients were transferred when at least three of the criteria were fulfilled or if the patient’s condition deteriorated and continuous monitoring, adrenergic drug treatment or mandatory ventilation was necessary.
The inclusion criterion was a positive urine culture from the renal pelvis. Urine collection from the renal pelvis was done by aspiration through the ureteral stent or the nephrostomy tube.
Intravenous antibiotics were administered immediately afterwards. The standard antibiotic regimen consisted of the intravenous administration of cephalosporin and aminoglycoside (cefazoline and gentamycin) for at least 3 days, which was then changed to oral treatment if the patient’s condition allowed. Antibiotic treatment was also changed if resistance was found in the urine culture. Antimicrobial therapy was established by recording typical profiles of the infecting microorganisms and susceptibility.
Statistical analyses were performed using the Fisher’s exact test, the Chi-squared test, and the Mann–Whitney rank sum test.
Results
A retrospective chart review was done for 189 patients with symptomatic hydronephrosis and subsequent drainage of the upper urinary tract. Ninety-two patients were diagnosed with infected hydronephrosis, presenting with flank pain, fever and dysuria. Forty-two (46%) of these patients had negative urine culture from the renal pelvis, as 38 (90%) had taken antibiotics prior to admission. Fifty patients (54%, 36 female and 14 male) were diagnosed with infected hydronephrosis and had a positive urine culture confirming bacterial infection of the upper urinary tract. In this group, eight patients (16%) had taken antibiotics prior to admission. Thirty-five (70%) patients received a nephrostomy tube, and 15 (30%) underwent ureteral stent placement using a mono-J or double-J stent.
Fifteen patients (32%) had to be transferred to the ICU. All of them had persisting hypotension, fever and tachycardia. Three patients (20%) had hypoxemia and two patients (13%) had disseminated intravascular coagulation (DIC). The median age of the ICU group was 73 years compared to 67 years for the non-ICU group. The average stay at the ICU was 2.8 days. Two ICU patients required adrenergic agents for blood pressure stabilization and mechanical ventilation for hypoxemia. The median hospital stay was 23 days for the ICU group compared to 9 days for the non-ICU group (P=0.02). The median hospital stay of non-ICU patients was 19.7 days in the nephrostomy group and 10.7 days in the ureteral stent group (P=0.02) (data not shown).
The median temperature on admission of patients later transferred to the ICU was 39°C and significantly higher than the non-ICU patient group with 37.2°C (P=0.0004). With a cut-off level of 38.5°C for initial temperature on admission, specificity was 93% and sensitivity was 85%. The average time to normal temperature was 2.1 days in the ICU group and 1 day in the non-ICU group (P=0.005). No significant difference was found in either group (ICU patients vs non-ICU patients) for initial white blood count (WBC), mean C-reactive protein (CRP), serum creatinine or time until normalization of these parameters (Table 1). The maximum values of the parameters mentioned also were not significantly different in both groups (data not shown). The distribution of coronary heart disease, hypertonia or diabetes did not significantly differ between the two groups, but obesity (a BMI over 30) was found four times more often in the ICU group and proved to be statistically significant (P=0.002).
Thirty-five of the 50 patients (70%) had typical signs of infected hydronephrosis without systemic inflammation, while 13 (26%) had signs of SIRS, and 2 (4%) were diagnosed with severe sepsis or urosepsis (Table 2). These two patients required adrenergic agents and mechanical ventilation but did not develop MOFS. Blood and urine cultures were positive (Gram–negative bacteria: Escherichia coli, Pseudomonas group) in three of the ICU patients but in none of the non-ICU group.
The main cause (52%) of obstruction was the stones located in the proximal (8%), middle (31%) or distal (61%) ureter. Malformations including narrowing of the ureteropelvic junction and Ormond’s disease were observed in 26% of the cases and extra-ureteral tumors in 12%.
Pathogens in the urine culture included E. coli in 53.3% (78% female, 22% male), Enterococcus in 20% (75% female, 25% male), the Pseudomonas group in 8.3% (60% female, 40% male), and Staphylococcus aureus in 6.6% of the patients (75% male, 25% female). Fungi (Candida albicans) were observed only in 2 cases (3.3%) and they did not belong to the ICU group. Two antibiotics were combined in 58% of the cases, three in 10% and four in 4%. See Table 3 for microbiological and antibiotic features.
Discussion
Infections of the upper urinary tract require antimicrobial agents. This situation is complicated by infected urine that cannot be drained from the renal pelvis due to ureteral obstruction, which may eventually lead to infected hydronephrosis. After rapid decompression by percutaneous nephrostomy tube insertion or retrograde stent placement, the reduction in intrarenal pressure improves renal perfusion and function which enables the effective application of systemic antibiotics.
The clinical course of most patients is favorable, but some require more than decompression, antibiotic treatment and fluid substitution. These patients are commonly diagnosed as having urosepsis. Urosepsis is bacteremia originating from the urinary tract and patients suffering from urosepsis require intensive care in most cases. Clinical manifestations of this condition vary from SIRS to septic shock with MOFS and death. One of the aims of this study was to analyze the incidence and the clinical course of patients with infected hydronephrosis leading to urosepsis. To identify patients who are at risk of developing urosepsis, we focused on easily assessable parameters that are routinely monitored.
C-reactive protein has been the subject of a variety of investigations in urology and intensive care medicine. Wu et al. [12] demonstrated that the plasma levels of C-reactive protein and the erythrocyte sedimentation rate in patients with pyonephrosis are higher than those in patients with infected hyronephrosis. Reny et al. [13] reported that a decrease in CRP of more than 50 mg/l within 4 days after admission was the best predictor of recovery. Their study included patients from all departments of a university hospital with various diseases such as pneumonia, mediastinitis or urinary tract infections who had to be admitted to the ICU. In comparison with our study patients, neither the initial CRP level nor the reduction velocity within the first 10 days was predictive of the clinical course. Moreover, comorbidity rate with diabetes mellitus, cancer or coronary heart disease was not higher in the ICU group, but obese patients were at a significantly higher risk to develop SIRS and septic syndrome. The duration of symptoms until first clinical presentation did not significantly affect the clinical course either. Thus, we can exclude treatment delay as an explanation for the septic course of infection. Nevertheless, the initial temperature was higher in patients later transferred to the ICU, and there was a statistical correlation between a severe course and an initial temperature of over 38.5°C.
PCN application carries a higher risk of bacterial dissemination throughout the vascular system, especially if antibiotic treatment is delayed until puncture in order to obtain a positive urine culture. In the study presented, the two groups with ureteral stent or nephrostomy tube placement were compared to evaluate whether the decompression method increases the risk of urosepsis. We have to mention that the patient number was not balanced as 70% of the patients in our study received nephrostomy tube and 30% ureteral stent placement. Moreover, the design of this retrospective study does not allow a valid conclusion about effectiveness of either method, which has been the issue of the aforementioned studies [6–9]. Our patient selection was not random and therefore, comparing the advantages of percutaneous and internal drainage of the renal collecting system, we were not able to classify one method as superior to the other. Nevertheless, no significant difference in clinical course was found, confirming the results from other studies. In a study with 42 patients, Pearle et al. [6] showed that both procedures are equally effective, leading them to recommend PCN, since ureteral stent placement is twice as expensive. In their study, 62% of the patients underwent ureteral stent placement under general anesthesia, which may be a nation-specific modus operandi, since stent placement in Germany is almost always performed with intravenous sedation alone.
In our study, patients with retrograde stent placement left hospital much earlier than patients with nephrostomy. We avoid discharging patients with a nephrostomy tube due to the higher rate of known discomfort. During recovery, patients receive a double-J stent, and the cause of obstruction, usually stones, is eliminated.
Addressing the question of why only 54% of the patients with infected hydronephrosis had a positive urine culture from the renal pelvis, we argue that the majority of the patients received antibiotic treatment days before admission to the hospital. At first presentation, patients are seen by their family doctor and antibiotics are prescribed, when presenting with typical symptoms such as flank pain and dysuria. Usually, ultrasound is not performed at initial evaluation and hydronephrosis due to obstruction might be overlooked. If the symptoms do not, or only slightly resolve after antibiotic treatment, the patient will finally present at the hospital.
Establishing the differential diagnosis between infected hydronephrosis, SIRS and sepsis is extremely important, and various serological parameters like C-reactive protein have been evaluated, but specificity was limited. Procalcitonin, a novel inflammatory marker, is commonly used in intensive care medicine for defining the prognosis and further treatment of the disease [14]. It has been accepted as an early prognostic marker that is augmented upon worsening of the septic syndrome. Procalcitonin decreases with the resolution of the syndrome. Giamarellos-Bourboulis et al. [15] demonstrated that it is highest in critically ill patients with multiple organ dysfunction syndrome. However, there are still no data describing the effect of this inflammatory marker on infected hydronephrosis, SIRS or septic syndrome with an infectious focus in the urinary tract. Further studies must clarify whether it is a potential marker for predicting the clinical course of patients with diagnosed infected hydronephrosis.
Conclusion
It is only in rare cases that infected hydronephrosis leads to urosepsis with septic shock or MOFS. In our retrospective study, only two patients (4%) suffered from severe sepsis requiring adrenergic agents and mandatory ventilation, but they did not develop multiple organ failure syndrome. Nevertheless, SIRS was seen in nearly one-third (26%) of the patients. Infected hydronephrosis is a serious situation for any patient but the severe course of the disease can be avoided with the available methods of rapid decompression.
Based on the parameters examined in our study, we cannot predict which patient will suffer from urosepsis and require cost- and time-consuming intensive care medicine, but can conclude that patients with initial temperature above 38.5°C or obesity are at higher risk.
References
Talan D (2000) Short-course therapy for acute uncomplicated cystitis and pyelonephritis. Infect Urol 13(Suppl):S14
Roberts JA (1999) Management of pyelonephritis and upper urinary tract infections. Urol Clin North Am 26:753–763
Gossius G, Vorland L (1984) A randomised comparison of single-dose vs. three-day and ten-day therapy with trimethoprim-sulfamethoxazole for acute cystitis in women. Scand J Infect Dis 16:373–379
McCarty JM, Richard G, Huck W et al (1999) A randomized trial of short-course ciprofloxacin, ofloxacin, or trimethoprim/sulfamethoxazole for the treatment of acute urinary tract infection in women. Ciprofloxacin Urinary Tract Infection Group. Am J Med 106:292–299
Talan DA, Stamm WE, Hooton TM et al (2000) Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis pyelonephritis in women: a randomized trial. JAMA 283:1583–1590
Pearle MS, Pierce HL, Miller GL et al (1998) Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol 160:1260–1264
Lee WJ, Patel U, Patel S et al (1994) Emergency percutaneous nephrostomy: results and complications. J Vasc Interv Radiol 5:135–139
Pocock RD, Stower MJ, Ferro MA et al (1986) Double J stents. A review of 100 patients. Br J Urol 58:629–633
Watson RA, Esposito M, Richter F et al (1999) Percutaneous nephrostomy as adjunct management in advanced upper urinary tract infection. Urology 54:234–239
Gross AJ, Hummel G (1999) Goethe almost died of urosepsis. World J Urol 17:421–424
Bone RC, Balk RA, Cerra FB et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care. Chest 101:1644–1655
Wu TT, Lee YH, Tzeng WS et al (1994) The role of C-reactive protein and erythrocyte sedimentation rate in the diagnosis of infected hydronephrosis and pyonephrosis. J Urol 152:26–28
Reny JL, Vuagnat A, Ract C et al (2002) Diagnosis and follow-up of infections in intensive care patients: Value of C-reactive protein compared with other clinical and biological variables. Crit Care Med 30:529–535
Ugarte H, Silve E, Mercan D et al (1999) Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med 27:498–504
Giamarellos-Bourboulis E, Mega A, Grecka P et al (2002) Procalcitonin: a marker to clearly differentiate systemic inflammatory response syndrome and sepsis in the critically ill patient ? Intensive Care Med 28:1351–1356
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christoph, F., Weikert, S., Müller, M. et al. How septic is urosepsis? Clinical course of infected hydronephrosis and therapeutic strategies. World J Urol 23, 243–247 (2005). https://doi.org/10.1007/s00345-005-0002-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-005-0002-x