Abstract
The detection of circulating tumor cells (CTCs) plays a very important role in the prevention and treatment of cancer. However, because of the low content of tumor cells in peripheral blood, these cells have always been difficult to detect. An efficient and accurate imaging method, the dark-field scanning imaging method, was innovatively proposed for the detection of CTCs in filtered and colored peripheral blood specimens. Here, the original dark-field scanning system was improved. By introducing an ellipsoidal mirror system, the noise in the sampling process is greatly reduced, and the sampling accuracy is significantly improved. Meanwhile, an automatic identification algorithm was developed to identify and screen CTCs in a large number of blood samples. Comparing with the other CTC detection methods, this method does not require a complex biological enrichment process, which may cause loss and destruction of CTCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Circulating tumor cells (CTCs), which are the subgroups of cancer cells existing in the bloodstream, are key factors for the establishment of metastasis [1]. The detection of CTCs in the peripheral blood of cancer patients holds great promise. Furthermore, it has become increasingly important in noninvasive tumor diagnosis and efficacious for the real-time detection of cancer therapies [2,3,4,5].
In recent years, more than 40 techniques have been developed to detect circulating tumor cells, and new detection schemes are being proposed and tested continuously. Circulating tumor cells are extremely low in blood. Cristofanilli and others studied 177 breast cancer patients in 2004 [6]. Patients with more than 5 circulating tumor cells per 7.5 ml of whole blood had a shorter median progression-free survival (2.7 months vs. 7.0 months, P < 0.001) and shorter overall survival (10.1 months vs. 18 months, P < 0.001) compared patients with less than 5 circulating tumor cells per 7.5 ml of whole blood. Therefore, the enrichment of circulating tumor cells is a necessary condition for detecting circulating tumor cells. Common methods for the enrichment and detection of circulating tumors include immunomagnetic separation, fluorescence labeling, microfluidic devices, and fiber array scanning [7,8,9,10]. Many of these processes require multistep, labor-intensive processes, which may lead to adverse effects in the accuracy of detecting cancer cells in blood samples. Among the detection methods, only a handful of proposed methods reach the commercialization stage [11, 12], such as the CellSearch system. However, because only EpCAM+ cells can be detected in the process of immunomagnetic separation, there is a lack of detection of nonepithelial cancer cells that do not express EpCAM. Furthermore, the high cost of detection and unsatisfactory detection efficiency also pose challenges in their development processes.
In contrast, assays that combine single-step cell labeling technology and the noncontact detection method are able to identify CTCs in nondiluted whole blood sample within minutes. After screening, samples of suspected CTCs were further observed and judged by hematopathologist-trained technical analysts. First, CTCs from WBC can be enrichment by microsieve-defined differential separation, utilizing the size and deformability differences between the CTCs and normal blood cells [13, 14]. This size separation method provides the advantage of capturing both EpCAM-positive and EpCAM-negative CTCs without being limited by antigen expression on the cell membrane surface. Due to the physical separation principle, the destruction of cell structure and biological activity caused by the complex biological enrichment process is effectively avoided. Then, the enriched CTCs were stained for observation and detection.
In this paper, we propose a dark-field scanning imaging method for detecting CTCs. Dark-field imaging scattering microscopes (DSSM) have the ability to generate high-resolution images by collecting scattering signals [15]. Another advantage of the rotation scheme is its high readout speed, which can cover the whole sample in less than a minute [16]. The filtered and stained peripheral blood samples can be automatically identified and analyzed by scanning results. Suspicious CTC samples were screened from a large number of peripheral blood samples according to signal intensity and volume. Therefore, this recognition scheme has lower detection cost, faster detection speed, and higher detection efficiency.
2 Experiments and results
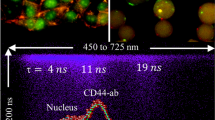
As shown in Fig. 1a, the optical detection system uses a 3.47 cm focal-length objective lens to focus a 405 nm wavelength laser diode to a diameter of approximately 20 μm. The scattered light is collected by an ellipsoidal mirror and detected by a photo multiplier tube (PMT). The light intensity illuminating the specimen can be controlled by adjusting the angle between two polarizers. A beam expander is used to expand the laser waist and fully fill the entrance pupil of the objective. An ellipsoidal mirror and a pinhole are used to form the dark-field light scattering system. The sample is placed on a stable spinner, which rotates at a constant frequency of 1000 Hz and produces a time-dependent scattering signal as the CTCs pass through the focused laser spot. By spinning the sample at high speed, static patterns are converted to high-frequency signals, which are away from 1/f noise and have higher signal-to-noise ratios than static measurements [17]. At the same time, the spinner is fixed on a one-dimensional linear translation stage. By combining with the translation stage and the high-speed spinner, the whole area of the sample can be scanned. During the scan, the output signals from the PMT are recorded by a DAQ card, which is triggered by a synchronizing signal from the spinner controller.
A high-pass RC filter is used to remove low-frequency signal drifts, such as sample wobble or variation of translation stage.
Scanning systems can be categorized into two types based on their different imaging methods. One is the bright-field scanning system, and the other is the dark-field scanning system. The bright-field scanning system collects the reflected light and distinguishes surface information through different reflected light intensity. Unlike the bright-field scanning method, scattered light is collected by the dark-field scanning method. From the point of view of imaging, limited by the Rayleigh criterion, the bright-field scanning system is a low-pass filter, which means that the reflected light carrying low-frequency components can only image the background information. In contrast, a dark-field scanning system picks up the scattered light, which can be recognized as a high-pass filter. It filters the most background information (low-frequency components) and leaves the outline of the sample (high-frequency components are also our detection objective). Hence, it is more suitable for observing the prepared blood sample. In addition, the dark-field method provides high contrast and sensitivity, which plays a crucial role in the quality of the imaging.
Because the specimen is transparent, the scattering noise from the specimen’s back surface and metal chuck needs to be eliminated. Therefore, an ellipsoidal mirror system with a 20 µm pinhole is used to select the signal only from the sample plane and to filter the stray light (Fig. 1a). According to the rules of geometric optics, the light emitted from one focal point of the ellipsoidal mirror will be focused to the another focal point of the mirror. In this work, the sampling point is adjusted to the focal point of the ellipsoidal mirror. The pinhole is placed at the other focal point of the ellipsoidal mirror in front of the PMT, which is used to selectively pass the scattering signals through the focus point while blocking back-scattering signals. Using this method, the back-scattering noise can be reduced to 0.0046 V, as shown in Fig. 1b. However, without the ellipsoidal mirror system (Fig. 1c), the noise is up to 1.3 V from the PMT readout, as shown in Fig. 1d.
The knife-edge method is used to measure the diameter of a laser spot. From the differential result of the scattering light intensity profile shown in Fig. 2a, the diameter is estimated as ~ 10.7 µm (FWHM) and ~ 20.4 µm (1/e2). To verify the detection capability of this system, flat quartz coated with 150 nm microspheres (manufactured by Powder Systems Limited) was used as the calibration target. The SEM image and scanning image are shown in Fig. 2b, c; 150 nm microspheres can be clearly identified by the detection system.
There are a series of CTC detection methods that use the biological characteristics enrichment technology, which is mainly based on the detection of specific proteins expressed by CTCs and their invasive ability [6, 18]. For this dark-field scanning method, the peripheral blood samples do not have to undergo complex bioaccumulation.
First, freshly drawn whole blood samples were filtered by a filter cartridge housing a polycarbonate membrane with 8 µm pores [13]. In this process, the fluid flow rate was controlled by a peristaltic pump to ensure that the filtration is efficient enough, but does not squeeze and destroy the cell structure. Red blood cells, platelets, and the smaller white blood cells were filtered out into the waste bottle, and the larger white cells and CTCs were left on the film slide. After filtration, the membrane was removed, and the remaining large cells were fixed and dyed. Although the smaller CTCs cannot be separated from this method, the majority of the CTCs were found to be two times larger than white blood cells [19]. Affected by liquid flow pressure, most of the white blood cells tended to stick to the filter membrane or get stuck in the small pores, because the volume is similar than that of the small pores. The larger circulating tumor cells float on the surface of the sample (Fig. 3b). After that, the blood cells on the specimen are stained using silver staining [20] and Wright Giemsa staining [21, 22]. The stained samples were sealed with optical resin to avoid excess bubbling after the sample has passed the inspection. The stained biological sample and the schematic diagram of the specimen structure are shown in Fig. 3.
The scattered light carrying the information about the cells is collected by the ellipsoidal mirror, focused back through the pinhole, and eventually enters PMT. Other scattered light caused by defocused plane-like particles existing on the chunk will be filtered by the pinhole. The signal from the PMT is sent to a DAQ card, where direct time traces of the sample are monitored and captured. Figure 4a shows the signal captured as a function of intensity and position. To compare, a 60-fold magnification optical microscope image in the same region is shown in Fig. 4b. Most of the white blood cells stick to the filter membrane or get stuck in the pores; as such, they do not protrude from the sample due to their height, and they will not be detected by the scanning system. Therefore, the number of cells scanned will be less than the actual observations. However, because CTCs are larger, they will float on the surface of the sample, so any included white blood cells will not affect the results of CTC detection. It can be seen that the detecting system can image the surface of the specimens very well. Using this method, the quantity, position, and size of the CTCs in the specimen can be detected.
3 Automatic identification
In Fig. 1a, the sampling points remain unchanged; the sample table moves while rotating, so the sampling points are distributed in Archimedes spirals on the surface of the sample. According to the voltage sequence of the sampling point and the coordinates of each point corresponding to the biological disk, the scanning results are plotted.
To demonstrate the potential of implementing the dark-field detection as a fast screening method, automatic identification of the CTCs is performed. The automatic identification is realized by a programming algorithm that identifies and counts the CTCs [23–25]. For different scanning images, the intensity of the spot is not enough to identify CTCs. However, for the same image, the intensity of the spot is an important feature to distinguish whether the spots are CTCs. A biological sample made from the peripheral blood of a cancer patient can be scanned to obtain a sequence of light intensity, as shown in Fig. 5c, which can be processed to obtain the light intensity distribution on the surface of the sample. Figure 5a shows a partial plotting result, which can be magnified again to observe a clearer image, as shown in Fig. 5b. We can calculate the number of suspected CTCs in the sample based on the light intensity and the size of the spot. The automatic recognition process is mainly composed of two steps.
First, the threshold is found. The dark-field scanning optical path is very sensitive, and the intensity of the scanning changes greatly; therefore, the critical value of cell determination in each scan result is determined by the percentage. As mentioned in the introduction of the experimental device, the scanning points are spirally distributed on the surface of the sample, and the sampling intervals between the two adjacent points are equal; as a result, the sampling points are not evenly distributed on the surface of the sample. Therefore, we cannot directly determine the critical value by directly performing a percentage determination on the scanning intensity. The first step is to resample the whole intensity map to get a uniform spatial distribution of the intensity matrix, which is also the basis of all subsequent automatic identification procedures. After arranging all the points by light intensity from strong to weak, threshold I is obtained: the points larger than I account for 0.0001% of the total number of points, and the corresponding intensity of the remaining points is less than I. The determination of 0.0001% is based on the calculation of the number of cells left in the sample corresponding to the surface area of the sample, which is then adjusted by experiment. The scanning results for other samples are equally effective. If the threshold value is greater than 0.0001%, the threshold value is too small, and the number of points to be analyzed after binarization is too large (Fig. 5e), which affects the detection efficiency. In contrast, if the threshold is less than 0.0001%, the threshold is too small (Fig. 5f), and binarization cannot completely retain the information of circulating tumor cells, affecting the accuracy of detection. In the scan result of Fig. 5d, we take the strength ranked 0.0001% point corresponding to the voltage value of the critical value to obtain an ideal two-level result; the critical value is 3.2 V.
The diameter of small cells in blood, such as red blood cells and platelets, is less than 8 μm; the size of large cells, such as white blood cells, is approximately 10–15 μm, but the size of CTCs is greater than 15 µm [6]. Here, 15 µm was taken as the determined threshold, and a cell diameter of greater than 15 µm was determined as a suspected CTC. Combined with the resampling resolution, this corresponds to 25 pixels in the graph. Using the light intensity threshold obtained in the previous step, the scan result is binarized. After binary processing, the corresponding pixels of the light spot in the image are counted, and a light spot larger than 25 pixels is judged as a suspected CTC. The result of scanning (Fig. 5d) shows a suspected CTC after calculation.
The samples were pathologically stained after filtration in the experimental process; as a result, we observed and counted the number of circulating tumor cells in each sample using an optical microscope before scanning. The numbers are always approximately 4–7 in patient bloods and 0 in the blood samples of healthy patients. After scanning, the count result was compared with the scanned image, and the number of suspected circulating tumor cells identified automatically; these two values are always consistent.
4 Conclusion
In conclusion, an ellipsoidal mirror dark-field scanning method was successfully applied to screen samples containing suspected CTCs from a large number of samples and greatly improved the detection efficiency. Through the use of a filter, an automatic scanning method was combined with the identification of circulating tumor cells in blood samples, and cells were successfully detected. This detection method has the following advantages: (a) size-based enrichment methods have been selected to reduce cost and avoid complex enrichment via a combination of fluorescent antibody and antigen, which reduces the damage to the sample structure and biomolecular specificity. (b) The ellipsoid reflector scattering light and dark-field scanning device realizes high-speed, low-noise, high-resolution imaging of the prepared blood samples. (c) The automatic recognition program can automatically recognize the number of suspected CTCs in the scanned image, thus further improving the detection efficiency of this experimental method. In summary, we have successfully proposed a low-cost, fast, and efficient method for identifying circulating tumor cells using a scattering light–dark-field scanner with an ellipsoidal mirror.
References
P. Paterlinibrechot, N.L. Benali, Cancer Lett. 253, 180 (2007)
M. Alunnifabbroni, M.T. Sandri, Methods 50, 289 (2010)
S. Maheswaran, D.A. Haber, Curr. Opin. Genet. Dev. 20, 96 (2010)
F. Tanaka, K.N. Yoneda, Clin. Cancer Res. 15, 6980 (2009)
V. Hofman, M.I. Ilie, E. Long, E. Selva, C. Bonnetaud, T. Molina, N. Vénissac, J. Mouroux, P. Vielh, P. Hofman, Int. J. Cancer 129, 1651 (2011)
M. LS Lim, M.C. Hu, W.C. Huang, A.T. Cheong, Gan, X.L. Looi et al., Lab Chip 12(21), 4388–4396 (2012)
S. Carroll, M. Alrubeai, J. Immunol. Methods 296(1), 171 (2005)
T.G. Ntouroupi, S.Q. Ashraf, S.B. McGregor, B.W. Turney, A. Seppo, Y. Kim, X. Wang, M.W. Kilpatrick, P. Tsipouras, T. Tafas, W.F. Bodmer, Br. J. Cancer 99, 789 (2008)
H. Ben Hsieh, D. Marrinucci, K. Bethel, D.N. Curry, M. Humphrey, R.T. Krivacic, J. Kroener, L. Kroener, A. Ladanyi, N. Lazarus, P. Kuhn, R.H. Bruce, J. Nieva, Biosens. Bioelectron. 21(10), 1893 (2006)
B. Fuchs, A. Romani, D. Freida, G. Medoro, M. Abonnenc, L. Altomare, I. Chartier, D. Guergour, C. Villiers, P.N. Marche, Lab Chip 6(1), 121 (2005)
L. Wang, P. Balasubramanian, A. Chen, S. Kummar, Y.A. Evrard, R. Kinders, Semin. Oncol. 43(4), 464 (2016)
K.C. Andree, G.V. Dalum, L.W.M.M. Terstappen, Mol. Oncol. 10(3), 395 (2016)
J. Lorincik, D. Marton, R.L. King, J. Fine, J. Vac. Sc. Technol. B 14(4), 2417 (1996)
D.D. Nolte, M. Zhao, X. Wang, J. Opt. Commun. 5(4), 456 (2009)
L. Peng, Diss. Abstr. Int. 66–10(B), 5471 (2005)
R. Königsberg, E. Obermayr, G. Bises, G. Pfeiler, M. Gneist, F. Wrba, M.D. Santis, R. Zeillinger, M. Hudec, C. Dittrich, Acta Oncol. 50, 700 (2011)
M. Borgatti, N. Bianchi, I. Mancini, G. Feriotto, R. Gambari, Int. J. Mol. Med. 21(1), 3 (2008)
L. Zabaglo, M.G. Ormerod, M. Parton, A. Ring, I.E. Smith, M. Dowsett, Cytom. A 55A(2), 102–108 (2010)
S.J. Hao, Y. Wan, Y.Q. Xia, X. Zou, S.Y. Zheng, Adv. Drug Deliv. Rev. 125, 3–20 (2018)
H. Busch, Y. Daskal, F. Gyorkey, K. Smetana, Can. Res. 39(3), 857–863 (1979)
P.V. Asharani, G.L.K. Mun, M.P. Hande, S. Valiyaveettil, Arch. Toxicol. 85, 743 (2011)
F. Vari, K. Bell, Electrophoresis 17, 20 (1996)
M. Gong, Z. Zhou, J. Ma, IEEE Trans. Image Process. Publ. IEEE Signal Process. Soc. 21, 2141 (2012)
A. Rodriguez, A. Laio, Science 344, 1492 (2014)
Y.J. Cha, W. Choi, O. Büyüköztürk, Comput. Aided Civ. Infrastruct. Eng. 32, 361 (2017)
Acknowledgements
This work is supported by the Project of Natural Science Foundation of Anhui Province of China (no. 1808085MF207). The fabrication work was partially carried out at the USTC Center for Micro and Nanoscale Research and Fabrication.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, C., Xu, K., Qin, J. et al. Ellipsoidal mirror dark-field scanning for detection of circulating tumor cells. Appl. Phys. B 125, 38 (2019). https://doi.org/10.1007/s00340-019-7143-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00340-019-7143-x