Abstract
Laser-accelerated electron pulses have been used to irradiate human tumors grown on mice’s ears during radiobiological experiments. These experiments have been carried out with the JETI laser system at the Institute of Optics and Quantum Electronics in Jena, Germany. To treat a total of more than 50 mice, a stable and reliable operation of the laser-electron accelerator with a dose rate exceeding 1 Gy/min was necessary. To achieve this, a sufficient number of electrons at energies in excess of 5 MeV had to be generated. The irradiation time for a single mouse was a few minutes. Furthermore, the particle pulses’ parameters needed to remain achievable for a time period of several weeks. Due to the online detection of the radiation dose, the unavoidable shot-to-shot fluctuations, currently still typical for laser-based particle accelerators, could be compensated. The results demonstrate that particle pulses generated with laser-based accelerators have the potential to be a future alternative for conventional particle accelerators used for the irradiation of tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Conventional radiotherapy using electrons or X-rays with energies up to 20 MeV from compact, electron linear accelerators is a well-established method in clinical radiooncology. In contrast, the usage of highly energetic ion beams (protons and heavier ions), which offers significant advantages for the treatment of deep-seated tumors [1], requires large-scale facilities. They are based on cyclotron- or synchrotron-accelerators and have large beam transport lines including gantry systems. Laser-based ion accelerators could provide a more compact and cost-effective alternative. Due to the substantial progress in laser-based particle acceleration which has been achieved during the last few years, the potential of its medical application has been considered for ion radiation therapy [2–5]. Moreover, laser-based electron radiation therapy is discussed as well [2, 6, 7]. The range of conventional clinical electrons (the therapeutic range of 20 MeV electrons in soft tissue is below 10 cm) is not sufficient for the treatment of deep-seated tumors. In contrast, laser-accelerated electron beams already reach maximum energies beyond 1 GeV [8], and the corresponding electron ranges exceed the thickness of the typical patient body. The potential clinical advantages of electron beams with energies above 100 MeV for radiotherapy purposes have already been identified by employing Monte Carlo simulations [9, 10] and dosimetric measurements [11].
Laser-accelerated particle beams, however, usually have a large beam divergence and a broad energy distribution. Moreover, they are also characterized by a very short pulse duration [12, 13] and a very high particle number per pulse. This leads to the possibility of achieving ultra-high dose rates per pulse, orders of magnitudes higher than what can currently be reached using conventional radiotherapy. Before these pulses can be applied in cancer therapy, however, beam transport and monitoring, irradiation field formation, and dosimetry have to be established. Moreover, the radiobiological effectiveness of these very intense pulses must be investigated thoroughly. Establishing the new laser-based irradiation technology requires translation from basic research to clinical application. In the first translational step, in vitro irradiation of human cell monolayers was performed with laser-accelerated electron [14, 15] and proton [16–19] pulses. The next translational step comprises the accomplishment of in vivo experiments. Post-irradiation dose analysis of radiobiological in vitro experiments was sufficient to determine dose-response-curves of irradiated cells of a monolayer. However, for in vivo irradiation and likewise future clinical application, the accurate delivery of a prescribed dose to the tumor’s volume using online beam monitoring is essential. Since acceleration and precise dose delivery is less challenging for electrons than for the much heavier protons, first in vivo experiments were performed with laser-driven electrons.
The first quasi-monoenergetic laser-accelerated electron pulses were experimentally measured in 2004 [20–22]. Here, a plasma wave generated by the driving laser pulse can be used as a co-propagating accelerating structure. When electrons are injected into this plasma wave, e.g., through self-injection induced by wave breaking, they can be accelerated to relativistic energies over distances of only a few millimeters. Since 2004, immense progress has been achieved in this field. The stability of the energy has improved [23, 24] as well as the stability in pointing [25]. Different influences like focusing geometry [26], plasma density, laser energy, and focus quality [27] were investigated. However, shot-to-shot and day-to-day fluctuations still remain the main challenge for the controlled application of these particle pulses.
Here, we report on an experiment in which laser-accelerated electron pulses have been used—to our knowledge for the first time—to irradiate human tumors grown on mice’s ears. The irradiation and dosimetry setup are presented by Schürer et al. [28]. A detailed description of the radiobiological results will be published elsewhere. In this paper, we concentrate on the description of the laser-based electron source. Its parameters and reliability will be analyzed as well as the online characterization of critical parameters and their applicability for the irradiation experiment.
2 Radiobiological considerations
To study the radiobiological effectiveness of laser-accelerated particle beams in vivo, and therefore of ultra-intense and ultra-short particle pulses, several beam requirements have to be fulfilled. With regard to patient irradiation, the radiation source has to provide a dose rate of 1 Gy/min or more. This dose rate is necessary to achieve a reasonably short irradiation duration of a few minutes, but also to exclude the influence of early repair mechanisms in the cells which would influence the result. A dose rate of 1 Gy/min corresponds to an electron flux of about 400 pC/min assuming a beam diameter of 10 mm. A prescribed dose needs to be delivered with high accuracy with respect to total dose and dose homogeneity in the target volume. This requires the online monitored application of multiple pulses in combination with a reasonably high shot-to-shot intensity stability. Only high power laser systems with a sufficiently high repetition rate of at least several pulses per minute have the potential of meeting these requirements.
Present-day high repetition rate, high power lasers can accelerate protons up to energies of 20 MeV. This corresponds to a penetration range of 4 mm in water. In preparation for the first in vivo proton experiments small human tumors grown on the ears of nude mice were established. In order to evaluate the tumor model and the handling procedure for a large number of animals with the challenging conditions of an experimental laser particle source, the experiments were first performed with electrons. Particle acceleration and homogeneous dose distribution in the target volume are easier to achieve for the lighter electrons than for protons. While the radiobiological effectiveness differs between electrons and ions, it is well understood for both types of particle pulses. Hence, the influence on the radiobiological effectiveness due to the higher dose rate per pulse could also be studied with electrons. The first radiobiological experiments with cells were therefore performed with electrons [14] before investigations with protons are carried out.
To be able to handle the irradiation of more than 50 mice, tumor transplantations were staggered. Between 5 and 20 days after the transplantation, the tumors had grown to a size of 2–3 mm in diameter, which is optimal for irradiation. Once this size was reached, the irradiation had to be carried out during a 1-day time window with the prescribed dose of 3 or 6 Gy. Due to this time constraint, a long-time stability and reproducibility of the laser system were crucial for the success of the experiment. An electron beam suitable for tumor irradiation had to be available on demand over a period of four weeks. This may still be a challenge for high-intensity laser systems and—as a consequence—for the laser-accelerated particle beams.
3 Setup
The experiments have been carried out using the JETI laser system, a 40 TW Ti:sapphire laser operated at the Institute of Optics and Quantum Electronics in Jena, Germany. The laser pulses have a duration of 30 fs (FWHM) and deliver an energy of approximately 700 mJ on target. The maximum repetition rate of the system is 10 Hz. During the experiment, the laser pulses were focused by an f/13 off-axis parabolic mirror to a focal spot with a diameter of 13 μm (FWHM) and an averaged intensity of 8 × 1018 W/cm2. A 2.4-mm-long supersonic hydrogen gas jet was used as a target. The gas in the focal volume was fully ionized by the laser pulse generating a plasma with an electron density of 1…2 × 1019 cm−3. The operation of the gas jet and the acceleration of the electrons were carried out in an evacuated interaction chamber. This was necessary to prevent unwanted self-modulation or self-focusing of the driving laser pulse prior to the interaction with the target gas. The limited available pump rate of the vacuum system restricted the repetition rate of the gas jet to a maximum of 1 Hz in this experiment.
In Fig. 1, the setup for the irradiation of the mice’s ears is shown. A magnetic energy filter was used directly behind the gas jet. It comprised two yokes with four counter-orientated neodymium magnets generating a magnetic field of about 60 mT between the poles and could be used to filter out electrons with kinetic energies below 5 MeV. Such low energy electrons would not have fully penetrated the beam line and the mice’s ears. Therefore, they would not have been detectable by either the online or the offline dose measurement devices positioned behind the mice’s ears. Moreover, the influence of the electron spectrum on the radiobiological results is minimized by filtering out the biologically more effective low energy electrons [29].
Experimental setup. The laser pulses were focused into a supersonic hydrogen gas jet. Electrons with energies below 5 MeV were filtered out using a magnetic chicane. Behind this filter, the electrons had to pass through a collimator. A scintillating screen was positioned in front of the collimator to control the relative alignment of the electron beam and the collimator. A 4-mm-thick aluminum plate was positioned between the magnetic filter and the scintillating screen to shield the latter against laser light. The electrons left the vacuum through a 1-mm-thick aluminum plate, before they penetrated the tumor on the mouse’s ear. To determine the lateral dose distribution, radiochromic films were placed before and behind the mouse’s ear. For online dosimetry, an ionization chamber and a Faraday-cup were used. The entire setup after the vacuum window could be exchanged with a magnetic electron spectrometer
Behind the magnetic filter a collimator was positioned to block the low energy and large divergence electrons. In the collimator, we have used a rectangular aluminum prism (100 × 100 × 140 mm3) with an angled front side and a hole of 10 mm diameter. The residual length at the nominal beam path was 118 mm. The orifice confined the electron beam on the mouse, so that only the tumor on the ear was irradiated. A mini electron spectrometer measured the spectral distribution of the electrons behind the collimator to verify that only electrons above 5 MeV reached the mouse’s ear.
The front side of the collimator, i.e., the side facing the gas jet, was cut at an angle of 45°. On this tilted surface, a scintillating screen was mounted to align the collimator with respect to the electron beam. To shield the scintillator against laser light, a 4-mm-thick aluminum plate was fixed between the magnetic filter and the scintillating screen. This plate also helped to homogenize the electron beam.
A 1-mm-thick aluminum plate was placed behind the collimator acting as a vacuum window for the electrons. The holder, which was necessary to ensure a fixed position of the mice during the irradiation, helped to position the tumor 46 mm behind the window. Between the window and the mouse’s ear was another collimator, a lead plate of 10 mm thickness with a hole of 6 mm diameter. The adjustable collimator system together with the aluminum plates ensured a homogenous dose distribution over the tumor’s volume even with the slight lateral displacement of the electrons exiting the chicane filter.
The exact radiation dose was retrospectively determined using radiochromic films that were situated directly in front of each mouse’s ear. Analysis of the films also allowed the spatial dose homogeneity over the beam spot size to be measured for each tumor irradiation event. However, to allow for an online measurement of the applied dose, an ionization chamber and a Faraday-cup were used. The ionization chamber measured the accumulated dose. To verify that the dose rate was high enough, the bunch charge of single pulses were measured with the Faraday-cup. This cup could measure the charge of the electrons with kinetic energies of up to 170 MeV. This online measurement of the dose was pivotal for taking into account the unavoidable shot-to-shot fluctuations of the parameters of the electron pulses.
After the daily beam alignment, dosimetric measurements were performed using the mouse holder. Three identical sets of radiochromic films were irradiated and analyzed. Each set comprised a film at the dosimetric position, i.e., directly before the mouse’s ear, as well as a stack of films of 2 mm thickness situated at the mouse’s ear position. Using these measurements, the online measured values from the Faraday-cup and the ionization chamber were calibrated to the dose measured with the radiochromic films. The slight difference between the dose measured at the dosimetric position and the dose measured at the mouse’s ear position was included in the consideration. Moreover, the irradiation of the film stack allowed for the analysis of the dose’s homogeneity at the tumor’s position as a function of depth.
Irradiation of each tumor was then performed until the integrated online dose measured by the ionization chamber reached the prescribed dose. With this procedure, the relative deviation between the applied and the required dose was smaller than 6 %. This would not have been possible by using radiochromic films or any other offline diagnostic method alone.
To measure the energy distribution of the electrons, a magnetic spectrometer could be attached to the vacuum system behind the collimator. This spectrometer resolves an energy range from 10 to 250 MeV and has a half acceptance angle of 10 mrad. Due to the divided scintillating screen, the measured electron spectra exhibit a gap in the region between 55 and 60 MeV.
4 Experimental results
4.1 Beam profile of the electron pulses
To ensure a controllable irradiation of the tumors with laser-accelerated electrons, the main task was to optimize the parameters of the electron pulses including their transverse charge distribution and the dose rate delivered by the pulses. The scintillating screen placed in front of the collimator was used to characterize the parameters of the electron pulses before the actual irradiation experiments started. The properties of the electron pulses could and had to be optimized on a daily basis. For this purpose, we varied the background pressure of the gas nozzle and the position of the gas jet with respect to the laser focus. Focusing into the leading edge of the gas jet resulted in highly energetic electron bunches exhibiting monoenergetic features. However, when the laser focus was shifted towards the center of the gas jet, electron bunches with a broader spectrum and much higher charge were generated. In addition to a high charge per pulse, it was important that the electron beam was collimated and had a high pointing stability.
Figure 2 shows images of the scintillating screen. The left side Fig. 2a–e presents the transverse electron beam profiles before the collimator was aligned. Here, the electron pulses were pointing slightly upwards, resulting only in a partial coverage of the 10-mm-diameter collimator hole. The small images Fig. 2a–d show representative single shots, indicating a stable pointing of the electrons better than 15 mrad. The beam profile in Fig. 2e, accumulated over approximately 30 consecutive shots, indicates that the averaged electron beam is smaller than the diameter of the hole.
Electron beam profiles. The scintillating screen was used to align the collimator with respect to the direction of the electron beam. The small pictures represent single-shot images of the scintillating screen. The large pictures were accumulated over approximately 30 consecutive shots and were normalized to the summed maximum value. The images in the middle columns f–j show aligned electron pulses, which were stable in pointing within 15 mrad and contained a high bunch charge. When the collimator was not well aligned, the electrons were not homogeneously distributed around the 10 mm hole. An example of such a case is shown in the images in the left columns, where the averaged transverse profile of the electron beam has its intensity maximum 10 mrad above the center of the hole. The black crosses in e mark the centers of intensity of the single pulses. Only the part of the electron pulses passing the collimator entrance hole could irradiate the mouse’s ear. Due to the degradation of some optical elements in the laser system the electron pulse parameters could not be kept stable over the entire campaign. The electrons shown in the right columns were less collimated, had fewer bunch charge and a less stable pointing. On average, they had a non-circular distribution around the collimator
After aligning the collimator with respect to the averaged electron beam direction, most of the electrons could pass the collimator. Due to this successful alignment, only a small signal remained visible in the images Fig. 2f–i. These few electrons caused only a weak, symmetrical halo in the accumulated image in Fig. 2j. However, a small signal like this could also be generated by pulses of very low bunch charge. Therefore, the online diagnostic behind the collimator was used to distinguish between the case where electrons had passed the collimator and the case where only few or no electrons at all were present. Both online diagnostics, the Faraday-cup and the ionization chamber, measured the dose per pulse. They could thereby determine unambiguously if the bunch charge of the electron pulses was high enough. The radiochromic films ensured that the spatial dose distribution at the tumor’s position was homogeneous across the beam’s transverse profile and that the collimator was aligned properly. The evaluation of the Faraday-cup data will be discussed in Sect. 4.3.
The laser ran fully amplified with a 10 Hz repetition rate for 5 to 6 days a week during this campaign. This caused a slight degradation of certain optical elements of the laser (e.g., compressor gratings, beam-line mirrors, etc.) during the course of the campaign. As a result, the parameters of the electron pulses were affected. Their degree of collimation, their bunch charge as well as their pointing stability degraded. As shown in Fig. 2k–n the single electron bunches were widely distributed over the scintillating screen. The actual shape varied strongly from shot to shot. Even the transverse profile in the accumulated image Fig. 2o does not show a symmetric distribution around the collimator hole any more. Due to this degradation the number of electrons reaching the mice’s ears decreased and, accordingly, the dose per pulse diminished. To maintain the threshold dose rate of 1 Gy/min for tumor irradiation, an increase of the repetition rate of the electron bunches from 0.5 to 1 Hz was necessary. The online diagnostics provided the essential tools to detect and counteract these inevitable variations and made it possible to keep the dose rate constant.
4.2 Electron energy
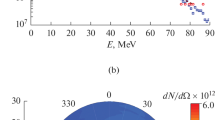
On some days of the campaign, the mouse’s ear irradiation setup behind the collimator was exchanged with the magnetic spectrometer to measure the energy distribution of the electrons. For this purpose, the block for the laser light in front of the collimator had to be removed to avoid scattering of the electrons. The magnetic energy filter was removed too. Some example spectra are shown in Fig. 3.
Four electron spectra are shown. The electron pulses during the campaign were optimized to have a high bunch charge of up to 250 pC. A large fraction of this charge was in the low energy range below 60 MeV. However, the electron energies also reached up to 170 MeV. As shown in Fig. 1, two scintillating screens were used for the electron detection, which caused the gap in the spectrum
The electron pulses were optimized to contain the maximum charge, i.e., to generate the brightest signals on the scintillating screen and the highest values as measured by the Faraday-cup. It turned out that the energy distribution of these electron pulses had a large amount of charge in the energy range below 50 MeV in the majority of cases. The charge varied strongly from shot to shot. For a few shots, the total electron charge reached values up to 250 pC, but there were also shots with very little charge.
The charge of the electron bunches was calculated from the brightness of the scintillating screens. In our energy range from 10 to 250 MeV the conversion efficiency of the scintillating screens is independent of the electron bunch energy and proportional to the charge. We used the Kodak Biomax MS for which an absolute calibration from charge to photon/sr is available [30]. The optical imaging system was calibrated using a helium–neon laser and a set of calibrated neutral density filters.
Figure 4a, b show the averaged spectra for a set from the beginning of the experimental campaign and one from the end, respectively. The total charge in Fig. 4a is a factor of 3.5 higher than in Fig. 4b. In Fig. 4c and d, the charge of every single pulse for the averaged sets in Fig. 4a, b are plotted. For the best set, the averaged charge per pulse was about 65 pC. However, the average charge of the electron bunches decreased toward the end of the campaign to 16 pC. Approximately 40–50 % of the charge is contained in the high energy part above 60 MeV. At the beginning of the campaign, about 20 % of all shots measured with the spectrometer contained no charge, e.g., due to a mispointed electron bunch or no injection of electrons into the plasma wave. This fraction increased toward the end of the campaign to more than 30 %.
Graph a shows the averaged electron spectrum for a data set from a day at the beginning of the experimental campaign. Here, the electron pulses were collimated, stable in pointing and had a high bunch charge as shown in Fig. 2. In c, the individual total bunch charges for all single shots from the data set in a are shown. The red diamonds mark the charge contained in the whole energy range from 10 to 200 MeV. The charge of the electrons above 60 MeV is shown by the blue triangles. Solid lines mark the averaged charge for the set. There was a decrease in bunch charge during the course of the campaign. The averaged electron spectrum in b, measured at the end of the campaign, contains a factor of 3.5 less charge than the spectrum in a. This decrease can also be seen in the charges of all the single shots from the same data set in d
4.3 Long-term stability
Using the data from the Faraday-cup, the evolution of the charge per pulse could be monitored over the course of a whole day. In Fig. 5, all shots from a single day at the beginning of the campaign and from a single day toward the end are displayed. There was a significant difference between shots with and without the mouse holder. When the mouse holder was inserted into the setup, the electrons were scattered and hence only a fraction of the charge reached the Faraday-cup.
The charge per pulse was measured with the Faraday-cup over the course of the experimental campaign. The plots show all measured data points for a single day at the beginning of the campaign (a) and for one at the end of the campaign (b). The green triangles and blue squares represent shots recorded with and without the mouse holder, respectively. When the mini electron spectrometer was included in the setup, the data acquisition with the Faraday-cup was disturbed leading to slightly lower values. The corresponding data points are marked by violet diamonds. The red dots represent the mean charge per pulse for every set
A large difference in the charge per pulse between the pulses generated during the earlier and the later part of the experimental campaign is apparent in the Faraday-cup signals. This difference was also clearly visible in the electron spectra. As mentioned above, this was most likely due to the degradation of certain optical elements in the laser chain.
In Fig. 5a, a strong increase in charge up to 60 pC per pulse is visible. This was achieved by optimizing the position of the gas jet with respect to the laser focus, by varying the backing pressure of the gas nozzle and by aligning the collimator. This optimization process was unfortunately not sufficient to significantly improve the relevant parameters of the electrons in Fig. 5b. After the parameters of the electron pulses were optimized, the mouse holder was inserted into the setup. The averaged electron bunch charge then remained constant throughout the day within a relative deviation of ±4 % (standard deviation).
For all dosimetry measurements including the irradiation of the radiochromic film stacks, the experimental setup was not changed. However, for measuring the spectral distribution of the beam the mini electron spectrometer was additionally inserted into the setup replacing the mouse holder.
In Fig. 6, the evolution of the averaged charge during the course of the whole campaign is shown. For this purpose, the measurements done with the electron spectrometer and the Faraday-cup were evaluated.
Since both diagnostics could not be used simultaneously, there are no correlated data sets. In Fig. 6a, the charge determined by the spectrometer is shown. It was only used on some days of the campaign. However, the large difference in charge between the beginning of the campaign and the end is obvious. On the first day, when the electron pulses were optimized, the averaged charge increased up to 65 pC per bunch in the energy range above 10 MeV. This value remained almost constant in the first part of the campaign until day 12. However, during the middle of the campaign, the charge per pulse strongly decreased, again most likely due to degeneration of the laser’s compressor gratings. As a consequence, the energy transmission of the compressor decreased. This loss in laser energy on target led to a degradation of the electron pulse parameters. The averaged charge per pulse dropped during the second part of the experiment to between 7 and 16 pC per pulse.
The degeneration over time is visible in the data of the Faraday-cup too, which is shown in Fig. 6b. In the first 2 weeks of the campaign, the dose per pulse was sufficiently high. Consequently, a repetition rate of 0.5 Hz was enough to achieve a considerably higher dose rate than the required 1 Gy/min. At this point in the experiment, the electron pulses were well collimated, stable in pointing, and had a high bunch charge. As previously mentioned, during the second half of the experiment, the dose rate was lower. Accordingly, the repetition rate had to be increased to 1 Hz to still reach the minimum dose rate.
5 Summary
In summary, we reported on the first in vivo irradiation using laser-accelerated particles. Human tumors grown on mice’s ears were treated with electrons accelerated by the JETI laser system. This system ran stable enough to provide electron pulses suitable for the irradiation on almost every day during a 4-week campaign. The combination with the online dose measurements ensured the treatment of the tumors with a prescribed dose and at a constant averaged dose rate. Even though the single-pulse dose varied significantly from shot to shot, the online measurements considerably relaxed the stability requirements. It is obvious that any improvement concerning the laser parameters, especially regarding long-term stability, will immediately be beneficial for further improvement of the measurements. However, during our measurements, the variations could be compensated immediately, e.g., by increasing the repetition rate of the electron pulses. Our results mark an important milestone for further tumor irradiation experiments with laser-driven particle accelerators.
References
D. Schardt, T. Elsasser, D. Schulz-Ertner, Rev. Mod. Phys. 82, 383 (2010)
K.W.D. Ledingham, W. Galster, New J. Phys. 12, 045005 (2010)
M. Martin, J. Natl. Cancer Inst. 101, 450 (2009)
V. Malka, J. Faure, Y.A. Gauduel, E. Lefebvre, A. Rousse, K.T. Phuoc, Nat. Phys. 4, 447 (2008)
T. Tajima, D. Habs, X. Yan, Rev. Accel. Sci. Tech. 02, 201 (2009)
C. Chiu, M. Fomytskyi, F. Grigsby, F. Raischel, M.C. Downer, T. Tajima, Med. Phys. 31, 2042–2052 (2004)
V. Malka, J. Faure, Y.A. Gauduel, Mutat. Res. 704, 142–151 (2010)
W.P. Leemans, B. Nagler, A.J. Gonsalves, C. Toth, K. Nakamura, C.G.R. Geddes, E. Esarey, C.B. Schroeder, S.M. Hooker, Nat. Phys. 2, 696–699 (2006)
Y. Glinec, J. Faure, V. Malka, T. Fuchs, H. Szymanowski, U. Oelfke, Med. Phys. 33, 155–162 (2006)
T. Fuchs, H. Szymanowski, U. Oelfke, Y. Glinec, C. Rechatin, J. Faure, V. Malka, Phys. Med. Biol. 54, 3315–3328 (2009)
O. Lundh, C. Rechatin, J. Faure, A. Ben-Ismail, J. Lim, De C. Wagter, De W. Neve, V. Malka, Med. Phys. 39, 3501–3508 (2012)
A. Buck, M. Nicolai, K. Schmid, C.M.S. Sears, A. Sävert, J.M. Mikhailova, F. Krausz, M.C. Kaluza, L. Veisz, Nat. Phys. 7, 543 (2011)
O. Lundh, J. Lim, C. Rechatin, L. Ammoura, A. Ben-Ismail, X. Davoine, G. Gallot, J.P. Goddet, E. Lefebvre, V. Malka, J. Faure, Nat. Phys. 7, 219 (2011)
L. Laschinsky, M. Baumann, E. Beyreuther, W. Enghardt, M. Kaluza, L. Karsch, E. Lessmann, D. Naumburger, M. Nicolai, C. Richter, R. Sauerbrey, H.P. Schlenvoigt, J. Pawelke, J. Radiat. Res. 53, 395 (2012)
O. Rigaud, N.O. Fortunel, P. Vaigot, E. Cadio, M.T. Martin, O. Lundh, J. Faure, C. Rechatin, V. Malka, Y.A. Gauduel, Cell Death Dis. 1, e73 (2010)
S.D. Kraft, C. Richter, K. Zeil, M. Baumann, E. Beyreuther, S. Bock, M. Bussmann, T.E. Cowan, Y. Dammene, W. Enghardt, U. Helbig, L. Karsch, T. Kluge, L. Laschinsky, E. Lessmann, J. Metzkes, D. Naumburger, R. Sauerbrey, M. Schürer, M. Sobiella, J. Woithe, U. Schramm, J. Pawelke, New J. Phys. 12, 085003 (2010)
K. Zeil, M. Baumann, E. Beyreuther, T. Burris-Mog, T.E. Cowan, W. Enghardt, L. Karsch, S.D. Kraft, L. Laschinsky, J. Metzkes, D. Naumburger, M. Oppelt, C. Richter, R. Sauerbrey, M. Schürer, U. Schramm, J. Pawelke, Appl. Phys. B 110, 437 (2013)
A. Yogo, T. Maeda, T. Hori, H. Sakaki, K. Ogura, M. Nishiuchi, A. Sagisaka, H. Kiriyama, H. Okada, S. Kanazawa, T. Shimomura, Y. Nakai, M. Tanoue, F. Sasao, P.R. Bolton, M. Murakami, T. Nomura, S. Kawanishi, K. Kondo, Appl. Phys. Lett. 98, 053701 (2011)
A. Yogo, K. Sato, M. Nishikino, M. Mori, T. Teshima, H. Numasaki, M. Murakami, Y. Demizu, S. Akagi, S. Nagayama, K. Ogura, A. Sagisaka, S. Orimo, M. Nishiuchi, A.S. Pirozhkov, M. Ikegami, M. Tampo, H. Sakaki, M. Suzuki, I. Daito, Y. Oishi, H. Sugiyama, H. Kiriyama, H. Okada, S. Kanazawa, S. Kondo, T. Shimomura, Y. Nakai, M. Tanoue, H. Sasao, D. Wakai, P.R. Bolton, H. Daido, Appl. Phys. Lett. 94, 181502 (2009)
S.P.D. Mangles, C.D. Murphy, Z. Najmudin, A.G.R. Thomas, J.L. Collier, A.E. Dangor, E.J. Divall, P.S. Foster, J.G. Gallacher, C.J. Hooker, D.A. Jaroszynski, A.J. Langley, W.B. Mori, P.A. Norreys, F.S. Tsung, R. Viskup, B.R. Walton, K. Krushelnick, Nature 431, 535 (2004)
J. Faure, Y. Glinec, A. Pukhov, S. Kiselev, S. Gordienko, E. Lefebvre, J.P. Rousseau, F. Burgy, V. Malka, Nature 431, 541 (2004)
C.G.R. Geddes, C. Toth, van J. Tilborg, E. Esarey, C.B. Schroeder, D. Bruhwiler, C. Nieter, J. Cary, W.P. Leemans, Nature 431, 538 (2004)
J. Osterhoff, A. Popp, Z. Major, B. Marx, T.P. Rowlands-Rees, M. Fuchs, M. Geissler, R. Hörlein, B. Hidding, S. Becker, E.A. Peralta, U. Schramm, F. Grüner, D. Habs, F. Krausz, S.M. Hooker, S. Karsch, Phys. Rev. Lett. 101, 085002 (2008)
J. Faure, C. Rechatin, A. Norlin, A. Lifschitz, Y. Glinec, V. Malka, Nature 444, 737 (2006)
A. Popp, J. Vieira, J. Osterhoff, Z. Major, R. Hörlein, M. Fuchs, R. Weingartner, T.P. Rowlands-Rees, M. Marti, R.A. Fonseca, S.F. Martins, L.O. Silva, S.M. Hooker, F. Krausz, F. Grüner, S. Karsch, Phys. Rev. Lett. 105, 215001 (2010)
A.G.R. Thomas, Z. Najmudin, S.P.D. Mangles, C.D. Murphy, A.E. Dangor, C. Kamperidis, K.L. Lancaster, W.B. Mori, P.A. Norreys, W. Rozmus, K. Krushelnick, Phys. Rev. Lett. 98, 095004 (2007)
S.P.D. Mangles, G. Genoud, M.S. Bloom, M. Burza, Z. Najmudin, A. Persson, K. Svensson, A.G.R. Thomas, C.G. Wahlström, Phys. Rev. ST AB 15, 011302 (2012)
M. Schürer, M. Baumann, E. Beyreuther, K. Brüchner, W. Enghardt, M. Kaluza, L. Karsch, L. Laschinsky, E. Lessmann, M. Nicolai, M. Oppelt, M. Reuter, C. Richter, A. Sävert, M. Schnell, J. Woithe, J. Pawelke, Biomed. Tech. 57, 62 (2012)
E. Beyreuther, W. Enghardt, M. Kaluza, L. Karsch, L. Laschinsky, E. Lessmann, M. Nicolai, J. Pawelke, C. Richter, R. Sauerbrey, H.P. Schlenvoigt, M. Baumann, Med. Phys. 37, 1392 (2010)
A. Buck, K. Zeil, A. Popp, K. Schmid, A. Jochmann, S.D. Kraft, B. Hidding, T. Kudyakov, C.M.S. Sears, L. Veisz, S. Karsch, J. Pawelke, R. Sauerbrey, T. Cowan, F. Krausz, U. Schramm, Rev. Sci. Instrum. 81, 033301 (2010)
Acknowledgements
We gratefully acknowledge the support by the BMBF (contracts 03ZIK445, 03Z1N511, 03Z1H531 and 05K10SJ2) and by the DFG (TR18).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nicolai, M., Sävert, A., Reuter, M. et al. Realizing a laser-driven electron source applicable for radiobiological tumor irradiation. Appl. Phys. B 116, 643–651 (2014). https://doi.org/10.1007/s00340-013-5747-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00340-013-5747-0