Abstract
Objective
To assess the relationship between intravenous iodinated contrast media (ICM) administration usage and radiation doses for contrast-enhanced (CE) CT of head, chest, and abdomen–pelvis (AP) in international, multicenter settings.
Methods
Our international (n = 16 countries), multicenter (n = 43 sites), and cross-sectional (ConRad) study had two parts. Part 1: Redcap survey with questions on information related to CT and ICM manufacturer/brand and respective protocols. Part 2: Information on 3,258 patients (18–96 years; M:F 1654:1604) who underwent CECT for a routine head (n = 456), chest (n = 528), AP (n = 599), head CT angiography (n = 539), pulmonary embolism (n = 599), and liver CT examinations (n = 537) at 43 sites across five continents. The following information was recorded: hospital name, patient age, gender, body mass index [BMI], clinical indications, scan parameters (number of scan phases, kV), IV-contrast information (concentration, volume, flow rate, and delay), and dose indices (CTDIvol and DLP).
Results
Most routine chest (58.4%) and AP (68.7%) CECT exams were performed with 2–4 scan phases with fixed scan delay (chest 71.4%; AP 79.8%, liver CECT 50.7%) following ICM administration. Most sites did not change kV across different patients and scan phases; most CECT protocols were performed at 120–140 kV (83%, 1979/2685). There were no significant differences between radiation doses for non-contrast (CTDIvol 24 [16–30] mGy; DLP 633 [414–702] mGy·cm) and post-contrast phases (22 [19–27] mGy; 648 [392–694] mGy·cm) (p = 0.142). Sites that used bolus tracking for chest and AP CECT had lower CTDIvol than sites with fixed scan delays (p < 0.001). There was no correlation between BMI and CTDIvol (r2 ≤ − 0.1 to 0.1, p = 0.931).
Conclusion
Our study demonstrates up to ten-fold variability in ICM injection protocols and radiation doses across different CT protocols. The study emphasizes the need for optimizing CT scanning and contrast protocols to reduce unnecessary contrast and radiation exposure to patients.
Clinical relevance statement
The wide variability and lack of standardization of ICM media and radiation doses in CT protocols suggest the need for education and optimization of contrast usage and scan factors for optimizing image quality in CECT.
Key Points
-
There is a lack of patient-centric CT protocol optimization taking into consideration mainly patients’ size.
-
There is a lack of correlation between ICM volume and CT radiation dose across CT protocol.
-
A ten-fold variation in iodine-load for the same CT protocol in sites suggests a lack of standardization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Contrast media is widely used to enhance visualization and detection of vascular and parenchymal structures and abnormalities in computed tomography (CT) imaging. The use of contrast media in CT has spiked over the years [1]. In the year 2019, an estimated 54.4 million CT examinations were performed using iodinated contrast media (ICM) in the United States [2]. Although modern intravenous ICM is safe with a low frequency of serious adverse effects, they are not entirely without adverse side effects [3]. Besides reports on increased radiation absorption associated with CT performed ICM administration [4, 5], radiation dose in ICM-CT examinations can also be higher than in non-contrast CT examinations due to a greater number of scan phases and/or acquisition scan factors associated with higher radiation dose [6]. Such an increase in radiation dose with ICM-CT underscores the need for adopting policies compliant with the principles of as low as reasonably achievable radiation doses which ensure reliable diagnostic image quality and as safe as reasonably achievable ICM use [7].
There are guidelines and technologies available to help imaging personnel optimize and manage radiation doses for CT [8]. Additionally, there are referral guidance and software to help address the question of justification for the use of CT for different clinical indications and different types of examinations, first exams, follow-up, etc. [9]. Unlike automatic tube current modulation and tube potential selection techniques (in some scanner models) that automatically adapt tube current and potential to patient size from the planning radiographs or scout images [10], there are limited automatic weight or size-based selection techniques for ICM usage in CT. Prior studies have documented a close relationship between ICM and radiation dose in CT, although most focus on optimizing and/or regulating CT radiation doses rather than on optimal usage of ICM in CT [11]. This has contributed to a lack of clear consensus on protocols and recommendations for ICM dosing in CT practice. Inconsistent ICM usage can affect the diagnostic quality of CT images and might be associated with higher radiation doses than needed to obtain the required information.
We hypothesized that there are considerable inconsistencies in ICM usage and dosage in CT, which are related to variations in CT radiation dose. Therefore, we performed a multicenter, international study to explore the relationship between the administration of ICM, scan factors, and radiation doses associated with contrast-enhanced CT (CECT) exams of the head, chest, and abdomen–pelvis (AP).
Material and methods
Ethical considerations
Our cross-sectional study received institutional review board approval. The need for informed consent was waived since no patient identifiers were recorded, and the study was retrospective in nature.
Participating sites recruitment
We recruited the participating sites using either personal contacts and email communication (n = 6 sites) or through social media platforms (n = 37 sites). For the latter, the study information about ConRad was disseminated on Twitter, Facebook, and LinkedIn platforms. The communication with the interested sites shared a summary of the study aims and methods and requested them to register with the following information: name of the individual registering, institution name, country, and contact information. Then, a post-doctoral research fellow (L.K. with 5 years of research experience) screened the registered sites to remove duplicate registration (> 1 individual registrant from the same site) and sent a formal invitation and instructions via the provided contact information (email). Of the 200 registrations across 24 countries, after excluding the duplicate registrations (n = 156), we invited registrants from 44 imaging sites to partake in the study from 24 countries. Of the invited sites, 84% (n = 37/44 institutions from 16 countries) provided the data for the study. The other 16% were excluded since they did not meet the deadline for providing data or did not receive institutional approval on time. We invited six additional sites via personal email communication who contributed sufficient CT data. Thus, there were 43 total sites in the study with an overall response rate of 86% (43/50) to the RedCap survey.
Study design
The multicenter (n = 43 sites), international (n = 16 countries), cross-sectional, and retrospective study had two parts.
Part 1: A Redcap survey to collect information related to the participating institution, CT scanners, and ICM type and usage.
Part 2: Patient data (n = 3258 patients) on CECT of 6 different protocols: routine head (n = 456 patients), routine chest (n = 528), routine abdomen/pelvis (n = 599), head CT angiography (head CTA, n = 539), pulmonary embolism (CT-PE) (n = 599), or multiphase liver (n = 537) protocols at 43 sites across 16 countries between January 2020 to June 2022 (Fig. 1) were recorded.
Questionnaire design
We built a three-part questionnaire in the REDCap software (Vanderbilt University, version v11.0.3) with 41 questions pertaining to the participating site, ICM, and CT machines and applied CT protocols. The first part of on-site details included questions related to institution name, location, type (private vs public, academic vs nonacademic), and size of the hospital in terms of the number of beds. The second part of the questionnaire obtained information on ICM (types of ICM used in the hospital, IV–IV-contrast brand name, IV–IV-contrast concentration, the availability and use of pressure injectors for different CT protocols), and CT scanners (number of CT scanners, scanner manufacturer, type of scanner (single source or dual-source and number of slices), and scanner name]. The final part requested more specific information related to the determination of ICM dosage for each of the included acquisition protocols (fixed or adapted to patient size based on weight, age, or body mass index). Because of the effects of tube potential on contrast enhancement and radiation dose, the questionnaire also requested information on the tube potential applied in different CT protocols (fixed tube potential for all patients or modified manually based on patient size or automatic tube potential selection technique).
Furthermore, in response to the ICM shortage at several institutions, we added a fourth part to the questionnaire requesting information on the ICM shortage (yes or no). For sites with ICM shortages, we enquired about the impact of such shortages on patient care or the scheduling of CECT examinations. Participating sites who submitted an incompletely filled REDCap questionnaire were re-contacted via email and requested to provide the missing information.
Patient data collection
Two study coinvestigators (L.K. and M.K.K.) created a fillable, multi-sheet Excel file (Microsoft Inc.) for collecting patient examination data in a uniform format. Each participating site was asked to provide information on 90 consecutive patients for the following 6 CT protocols (15 patients per each type of examination): routine head CT, head CTA, routine chest CT, CT-PE, routine abdomen/pelvis CT, and multiphase liver CT. The following information was recorded from each participating site: hospital name, patient age, gender, weight (kg), height (cm), body mass index (BMI, kg/m2), clinical indication for each CT examination, scan parameters (number of scan phases and kV for each scan phase), contrast information [concentration (mgl/mL), volume (mL), flow rate (mL/s), and technique for estimating scan delay (fixed, test bolus, and bolus tracking)] and CT radiation dose descriptors (CT Dose Index volume for each phase (CTDIvol in mGy) and Dose Length Products (DLP in mGy·cm) for each scan phase. We estimated the total iodine load per CT examination (product of the volume of ICM and contrast concentration) and iodine delivery rate (IDR, production of the flow rate of ICM injection, Per the World Health Organization classification of patient size based on BMI, we divided the patientsinto four groups underweight (BMI < 18.5 kg/m2), normal range (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese groups (BMI > 30 kg/m2).
Statistical analysis
All descriptive statistics were derived from Microsoft EXCEL. The inferential statistics were obtained from SPSS statistical software (version 20, IBM Inc.). We performed the Kolmogorov–Smirnov test to determine the normal distribution of the data. The normally distributed continuous variables were assessed as the mean and standard deviations while the non-normal distributed variables were presented as median and interquartile range (IQR) values. We performed a one-way analysis of variance to compare the normally distributed continuous variables and the multiparametric Kruskal Wallis test for comparing the non-normal variables (ICM and radiation dose descriptors). When comparing between sites and body regions, we normalized the data for patients' age, weight and CT scanner technologies. Furthermore, categorical variables were presented as frequencies with their corresponding percentages and were compared using the Pearson Chi-square test. We generated a tabular summary of the median or 50th percentile (achievable doses) and 75th (diagnostic reference levels) percentiles of reported CTDIvol and DLP for each protocol and participating site.
Results
Redcap survey
Figure 2 summarizes the details of the RedCap survey. Of the 43 participating sites, only 13 (32%) sites had a shortage of ICM for CT scanning. At these sites, Omnipaque (Iopamidol, Amersham) was the most common ICM (69%) followed by Visipaque (Iodixanol), (23%), and Optiscan (Iohexol) (7.7%) which were in shortage. According to the RedCap answers, none of the sites with ICM shortage reported any impact of the shortage on patient care due to several practice changes such as the use of another available ICM, prioritization of ICM use in inpatient and/or emergency referrals, decreases in tube potential and ICM volume, and triaging patients to other imaging modalities such as MRI and US.
Patient-specific data
Individual CT protocols: contrast and radiation doses
Table 1 summarizes patients’ characteristics, contrast injections, and radiation dose indices for the six protocols included in our study. There were no differences in the study results when the analysis was limited to the sites (n = 38/43) that provided at least 15 CT exams per body region as opposed to all sites regardless of the number of CT exams per body region.
There was significant difference in kV used between < 64-slice vs 64 and higher detector row scanners where 1363/1604 (85%) of the cases in 64 and higher detector row were done with a 120 kV followed by 160/1604 (10%) with 100 kV whereas 674/1124 (60%) of the less than 64-slice detector where done with a 120 kV and 224/1124 (20%) with 130 kV. Furthermore, there was no significant difference in radiation doses CTDIvol and total DLP between < 64-slice vs 64 and higher detector row scanners.
Routine head CT
Between the examinations with fixed (n = 34/43) and weight-based (n = 9/43) contrast volume, there were significant differences in age (weight-based: 46 ± 19 years vs fixed: 53 ± 18 years; p = 0.001), BMI (weight-based: 24.4 ± 4.7 Kg/m2 vs fixed: 26.6 ± 6.0 Kg/m2; p = 0.01), total iodine load (weight-based: 21.0 g (17.5–26.2) vs fixed: 24.5 g (16–30); p = 0.001), and iodine delivery rate (weight-based: 1225 mg/s (700–1750) vs fixed: 750 mg/s (640–1050); p = 0.001).
Head CTA
Most sites used a weight-based ICM protocol (n = 23/43) as opposed to fixed ICM volume (n = 20/43) with significant differences across the two approaches in patients’ BMI (weight-based: 24.8 ± 3.2 kg/m2 vs fixed: 26.3 ± 4.7 kg/m2; p = 0.030] and iodine delivery rate (weight-based: 1575 (1400–1750) mg/s vs fixed: 1400 (1200–1400) mg/s; p = 0.001]. There were no differences in total iodine load or ICM concentrations between the two injection protocols (p > 0.05).
Routine chest CT
There was a similar distribution of weight-based ICM (n = 22) and fixed ICM (n = 21) volume protocols with significant differences between patients’ age (weight-based: 54 ± 17 years vs fixed: 57 ± 17, p = 0.025), iodine load [weight-based: 26.2 (24–31.5) g vs fixed: 22.5 (18–24.5), p = 0.001], and iodine delivery rate [weight-based: 750 (630–1050) mg/s vs fixed: 900 (689–1200), p = 0.001].
CT-PE
There was a similar distribution of weight-based ICM (n = 21) and fixed ICM (n = 22) volume protocols with significant differences between iodine delivery rates [weight-based: 1575 (1400–1575) mg/s vs fixed: 1400 (1280–1600) mg/s, p = 0.001], but not between patients’ age, gender, BMI, and total iodine load (p > 0.5).
Routine AP CT
Twenty-four sites used weight-based ICM injection protocols and the remaining 19 sites had fixed ICM injection protocols with significant differences between iodine delivery rate [weight-based: 875 (690–1050) mg/s vs fixed: 900 (750–1050) mg/s, p = 0.006], but differences in patients’ age, BMI, gender, ICM concentration, and the iodine load (p > 0.05).
Liver protocol CT
For the liver protocol CT, 24/43 sites employed weight-based ICM injection protocols, and 17/43 sites used fixed ICM injection protocols with significant differences between iodine load [weight-based: 29.7 (25.6–34.8) g vs fixed: 28.0 (24.5–30), p = 0.022] and iodine delivery rate [weight-based: 1050 (1043–1400) mg/s vs fixed: 1000 (864–1200), p = 0.001], but no difference in patients’ age, BMI, and ICM concentrations (p = 0.05).
Individual CT protocols per site: contrast and radiation doses
There were significant differences in patient age, BMI, ICM concentration, volume, iodine load, iodine delivery rate, number of CT phases, and scan delays across individual CT protocols at the 43 participating sites (p = 0.001). There were no differences in patients’ gender distribution between the participating sites (p = 0.120).
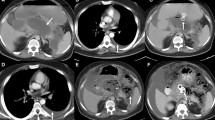
Table 2 summarizes CT radiation dose indices for the participating sites and CT protocols. institution and across different institutions for the same protocols (p < 0.001) (Fig. 3). Table 3 presents data on significantly different total iodine load and iodine delivery rates at different CT protocols across the 43 participating sites (p = 0.001). There was no significant difference between radiation doses for non-contrast (CTDIvol 24 [16–30] mGy; DLP 633 [414–702] mGy·cm) and post-contrast phases (22 [19–27] mGy; 648 [392–694] mGy·cm) (p = 0.142). Most sites with bolus tracking for chest and AP CT had lower CTDIvol than the sites with fixed scan delays (p < 0.001). Regardless of the CT vendor and model, body size, and scan protocols, most CT examinations were performed at 120 kV or 140 kV.
There was no significant correlation between patients’ size (BMI) and ICM or radiation doses for any of the six CT protocols included in our study (r2 ≤ − 0.1 to 0.1). When comparing median DLP and CTDIvol levels between different patient sizes, we noticed no significant difference between radiation doses for underweight-normal and overweight-obese patients (p > 0.05). Furthermore, in terms of total iodine load comparison in terms of different patient sizes, underweight-normal BMI patients received significantly lower total iodine load (p < 0.05) (Fig. 4). Regardless of the CT protocols, exams with bolus tracking and test bolus timing of scan delay had lower radiation doses (CTDIvol) as compared to the fixed scan delay (p < 0.001).
Box and whisker plots illustrate variations in CTDIvol and total iodine volume among patients in different BMI groups for routine head, head CTA, routine chest, PE protocol, routine AP and liver protocols. The bimodal distribution of radiation dose in underweight and obese patients (higher dose for smaller patients) for head CTA and chest CT could be related to a combination of variable and suboptimal acquisition factors
Discussion
CT technological advances and radiation dose awareness offer opportunities to optimize and reduce both ICM volume and radiation doses [12]. With improved detector efficiency, high X-ray tube power, automatic tube potential selection, automatic tube current modulation, and advanced reconstruction techniques, the use of lower tube potential (< 120 kV) can help improve contrast enhancement and lesion conspicuity, while enabling low ICM volume and radiation doses [13]. Despite the supporting scientific evidence in study settings [14], there is sparse data on whether and how advances and awareness of CT translate to real-world scanning practices. Our multicenter, international study in real-world settings provides anecdotal evidence on the appropriate use of scan factors, ICM volume, and radiation dose associated with head, chest, and AP CT examinations.
We report a lack of size-based differences in radiation doses across most CECT protocols. There were up to 10-fold inter-institution variations in radiation doses and total iodine load, which could be attributed to variations in scanner technologies and local practices. Furthermore, we employed a stratified analysis of doses by the scanner technology and found out that there was no difference with 4-fold interinstitutional variations in radiation doses among sites with both < 64-detector-row scanners and ≥ 64-detector row scanners. Multiple prior studies have reported on major variations in radiation doses in international settings with limited (such as in our study) and large clinical datasets [1, 6]. For example, Rebecca et al [1] reported on a large international registry of CT radiation doses from over 2 million CT examinations in adult patients across 151 institutions from seven countries. They documented major variations in radiation doses across countries despite controlling for patients, institutional, and scanner characteristics. The authors attributed such variations to the choice of technical parameters used during CT image acquisition [1].
We also found a lack of any correlation between ICM volume and CT radiation dose descriptors across any CT protocol. Given that most non-contrast and post-contrast phases were acquired at a tube potential of 120 kV regardless of the anatomic regions and CT protocols, the scope for use of lower ICM volume or total iodine load and radiation doses is limited. If other scan factors are constant, lower tube potentials (< 120 kV) reduce radiation doses and allow users to decrease ICM volume and/or total iodine load. Conversely, a higher tube potential (≥ 120 kV) is associated with higher radiation dose and reduces CT attenuation values of ICM, thus requiring higher contrast volumes and iodine loads. Our study suggests an unfulfilled gap between research studies on the benefits of adjusting tube potential and current based on the body region, size, and clinical indications, and a lack of its real-world use. Sadly, a few sites used extremely low and fixed ICM volume (< 50 mL) for AP CT examinations at 120–130 kV, which highlights harsh economic and political disparities between developing and developed countries around the world. Although image quality or diagnostic adequacy evaluation was not part of our study, future studies should target the implication of such low ICM volume, particularly for an exam that contributes to the bulk of overall diagnostic medical radiation doses.
On the upside, a few sites that used weight-based ICM dosage had expected variations in radiation doses. Other sites could emulate such protocols to improve their practices. Likewise, sites that used bolus tracking or timing bolus, had lower ICM usage and radiation doses than sites with fixed ICM volume. Most sites used bolus tracking or timing bolus techniques to trigger scanning for CTPE, as opposed to head CTA and biphasic liver protocol CT where fixed scan delay was frequent. The latter can result in suboptimal contrast enhancement and require either additional scan phases or repeat acquisition if the initial scan timing yields an insufficient contrast enhancement. Another aspect of our study pertains to the size-based ICM usage at most participating sites, which resulted in expected differences in total iodine load between patients of different body habitus for all CT protocols. However, up to 10-fold variation in iodine load for the same CT protocol from different sites suggests a lack of standardization with at least some sites using higher and others using much lower ICM protocols.
Our study has several implications. First, high variability in all CT protocols for both ICM injection and radiation doses underscores the need for education and practice improvement at several sites. Second, despite significant differences in ICM parameters across different protocols for patients in different BMI groups, there was major variability in ICM injection within each BMI group. This suggests the need for the development of standard guidance for weight and clinical indication-based contrast injection protocols. Also, the lack of radiation dose differences across different CT protocols and patients’ body habitus at most sites suggest the need for optimizing CT acquisition parameters. Although contradictory to the laws of medical physics and fixed tube current/automatic exposure control (AEC) and automatic tube potential selection techniques, a lack of correlation between radiation dose and body size could be related to data inhomogeneity but was more likely related to either the random/suboptimal use of acquisition factors or the narrow range of BMI variation across different sites. For example, fixed tube current and tube potential will deliver the same radiation doses across different BMI patients, and suboptimal choice of reference image quality parameters (with high image quality demand) will lead to the use of higher tube current near the maximum allowed regardless of patient size. Third, despite the advantages of better contrast enhancement and lower radiation dose with lower tube potential, most sites use either 120 kV or 140 kV regardless of CT vendor, model, patient weight, or protocol type. Fourth, sites do not modify scan parameters between non-contrast and post-contrast CT. Fifth, multiphase is common for both the routine chest (58.4%) and AP (68.7%) CT protocols. Sixth, despite the risk of suboptimal contrast enhancement, a substantial number of CT-PE and liver protocol CTs are performed with a fixed scan delay. Lower radiation doses for sites with these observations will enable us to derive site-specific educational initiatives and recommendations for achieving best practices in CT scanning at the participating sites and beyond. We have summarized potential opportunities to optimize radiation dose and ICM use in Table 4.
There are limitations to our study. First, this is a retrospective survey-based study. Second, although we followed previously published guidelines and requested data on a minimum of 20–30 CT exams per body region, some institutions have provided fewer data for some regions compared with others which results in heterogeneity in case distribution. Furthermore, the heterogeneous distribution of CT datasets across different sites was attributed to the variations in practices and protocol usage across the participating sites. Third, in some countries, we have included only one institution and in others, two/three institutions, but the number of participating sites represents only a small fraction of imaging hospitals in each country. Therefore, the data cannot be generalized as the participation of additional sites could have led to different conclusions regarding contrast and radiation dose variations. Fourth, all sites recorded the data manually and manual data entry can lead to errors. Fifth, we did not include pediatric data in our project since there are separate protocols that are based on patients’ size and age. Sixth, we did not assess image quality which would have been an added value as some institutions were using very low contrast volume which could potentially be impacting the diagnostic appropriateness of image enhancement. However, image quality evaluation would likely not affect the results since such evaluation would not explain the over-use of multiphase CT (for example in chest CT) and the lack of difference in radiation doses between patients in different BMI groups which would have resulted in higher than needed quality in smaller patients and lower quality images in larger patients. Regardless of the CT vendor and model, body size, and scan protocols, most CT examinations were performed at 120 kV or 140 kV.
In conclusion, our multicenter, international ConRad study demonstrates substantial variability in ICM injection protocols and radiation doses across the included six CT protocols that were included in the study. Our findings suggest that further investigation is needed to fully understand the relationship between ICM usage and radiation doses, with the ultimate goal of optimizing CT scanning protocols to improve diagnostic quality and minimize unnecessary radiation exposure to patients.
Abbreviations
- AP:
-
Abdomen–pelvis
- CECT:
-
Contrast-enhanced CT
- CT:
-
Computed tomography
- CTA:
-
CT angiography
- CT-PE:
-
Pulmonary embolism
- ICM:
-
Iodinated contrast media
References
Smith-Bindman R, Wang Y, Chu P et al (2019) International variation in radiation dose for computed tomography examinations: prospective cohort study. BMJ 364:k4931
Davenport MS, Chu P, Szczykutowicz TP, Smith-Bindman R (2022) Comparison of strategies to conserve iodinated intravascular contrast media for computed tomography during a shortage. JAMA 328:476–478
Matamoros A (2009) Contrast Media: Safety Issues and ESUR Guidelines. J Nucl Med 50:1912–1912
Sahbaee P, Abadi E, Segars WP, Marin D, Nelson RC, Samei E (2017) The effect of contrast material on radiation dose at CT: part II. A systematic evaluation across 58 patient models. Radiology 283:749–757
Mazloumi M, Van Gompel G, Kersemans V, de Mey J, Buls N (2021) The presence of contrast agent increases organ radiation dose in contrast-enhanced CT. Eur Radiol 31:1–10
Rastogi S, Singh R, Borse R et al (2021) Use of multiphase CT protocols in 18 countries: appropriateness and radiation doses. Can Assoc Radiol J 72:381–387
Conway S (2016) Going beyond ALARA: Let’s keep contrast “ASARA”. Appl Radiol 45:38–40
Greffier J, Macri F, Larbi A et al (2015) Dose reduction with iterative reconstruction: optimization of CT protocols in clinical practice. Diagn Interv Imaging 96:477–486
Bang TJ, Chung JH, Walker CM et al (2023) ACR Appropriateness Criteria® routine chest imaging. J Am Coll Radiol 20:S224–S233
Mayer C, Meyer M, Fink C et al (2014) Potential for radiation dose savings in abdominal and chest CT using automatic tube voltage selection in combination with automatic tube current modulation. AJR Am J Roentgenol 203:292–299
Kalra MK, Becker HS, Enterline DS et al (2019) Contrast administration in CT: a patient-centric approach. J Am Coll Radiol 16:295–301
McCollough CH (2019) Computed tomography technology—and dose—in the 21st century. Health Phys 116:157–162
Lira D, Padole A, Kalra MK, Singh S (2015) Tube potential and CT radiation dose optimization. AJR Am J Roentgenol 204:W4–W10
Samei E, Pelc BJ (eds) (2020) Computed tomography. Springer, Berlin
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr Mannudeep Kalra
Conflict of interest
Two study coauthors (Mannudeep K. Kalra and Subba R. Digumarthy) have received unrelated research grants from Coreline Inc., Qure AI, Riverain Tech, Siemens Healthineers, and Vuno Inc. The remaining co-authors have no financial disclosures. All coauthors had independent access to the study data and the manuscript.
Statistics and biometry
One of the authors has significant statistical expertise: Dr. Lina Karout.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
None.
Methodology
-
Retrospective
-
Cross-sectional study
-
Observational
-
Multicenter study
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karout, L., ConRad Working Group. & Kalra, M.K. Survey of CT radiation doses and iodinated contrast medium administration: an international multicentric study. Eur Radiol (2024). https://doi.org/10.1007/s00330-024-11017-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-024-11017-7