Abstract
Objective
Acute traumatic injuries to the larynx, including fractures of the hyoid bone, cricoid, and thyroid cartilage, are uncommon injuries. The purpose of this study was to assess fracture and soft tissue patterns associated with laryngeal trauma.
Methods
This was a retrospective review of patients with laryngeal fractures who presented to two level I trauma centers and underwent CT imaging. Imaging findings, including fractures of the cartilaginous structures of the larynx and hyoid bone, and soft tissue abnormalities including focal hematoma, edema with non-focal hemorrhage, and additional penetrating injuries were recorded. Frequencies of fracture patterns were recorded.
Results
Thyroid cartilage fractures were most frequently observed occurring in 45/55 patients, followed by cricoid fractures in 13/55 patients. Hyoid fractures were encountered in 8/55 patients. Multi-site fractures were observed in 12/55 patients with thyroid-cricoid fractures occurring in 8/12 patients, followed by thyroid-hyoid fractures in 2/12 patients. Most multi-site fractures occurred in association with focal supraglottic hematomas (10/12), supraglottic edema and non-focal hemorrhage (11/12), and focal subglottic hematoma (5/12). All 13 cricoid fractures occurred with either focal supraglottic hematoma (7), focal subglottic hematoma (4), or edema with non-focal hemorrhage (13).
Conclusions
Thyroid cartilage fractures were the most frequently encountered fracture, followed by cricoid cartilage fractures. Cricoid fractures always occurred with soft tissue abnormalities. Recognition of fracture patterns in the setting of laryngeal trauma and associated patterns of soft tissue injury is important for practicing radiologists for early diagnosis of these conditions and reduction of associated morbidity.
Key Points
• Acute fractures to the larynx may be isolated fractures or occur as multi-focal fractures.
• Thyroid cartilage fractures are the most frequent fractures followed by cricoid cartilage fractures.
• Cricoid cartilage fractures always occurred in association with soft tissue abnormalities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute injuries to the larynx, including fractures of the hyoid bone, thyroid, and cricoid cartilages, are uncommon injuries occurring in approximately 1/5,000–30,000 emergency room visits in the USA [1,2,3]. Mortality has been associated with both blunt and penetrating traumatic injuries to the larynx related to acute airway obstruction. Morbidity from traumatic injuries to the larynx is associated with aspiration, inability to maintain an adequate airway, and phonation complications occurring in up to 37% of patients [4]. However, because these traumatic injuries to the larynx often occur with additional injuries, including intracranial and cervical spine injuries, traumatic injuries to the larynx are often overlooked [5].
Radiologists play an important role in the initial evaluation of patients with traumatic injuries to the head and neck. CT remains a conventional imaging approach for the evaluation of patients with traumatic injuries, particularly involving the head and neck. Prior publications on the imaging findings of laryngeal trauma and laryngeal fracture patterns have largely been through reports of limited case series and case reports, likely related to the uncommon incidence of these injuries [6,7,8,9,10,11,12,13]. Additional literature on laryngeal trauma and the detection of laryngeal fractures has focused on optimizing CT scanning parameters and reconstruction algorithms to improve the detection of these entities [14,15,16,17,18].
The purpose of this study was to perform a retrospective review of patients presenting to two level I trauma institutions with laryngeal trauma to assess the frequency of fracture injuries of the larynx on CT, and to assess patterns of soft tissue abnormality associated with fracture patterns involving the hyoid bone, thyroid cartilage, and cricoid cartilage. Knowledge of patterns of soft tissue abnormality associated with laryngeal trauma may help identify subtle fractures when assessing the larynx in the setting of acute trauma.
Materials and methods
Patients
This was a retrospective, IRB-approved study performed at two level I trauma centers in the same city in the Northeast United States.
Patients were identified through a keyword search of our PACS system for “laryngeal trauma” and “laryngeal injury” over an 18-year period from January 2000 to December 2018. Inclusion criteria were patients who underwent a CT neck or cervical spine, in the form of contrast-enhanced neck CT, CT angiogram of the neck (CTA), and/or non-contrast-enhanced CT of the neck or cervical spine, for the evaluation of acute neck and laryngeal trauma at both institutions. Exclusion criteria included patients who had CT scans, which were limited by motion or other artifacts precluding a diagnostic assessment, as well as patients with laryngeal fracture patterns, which were determined not to be acute.
Basic demographic data, mechanism of trauma (blunt versus penetrating injury), and presenting symptoms including hoarseness, neck pain, neck contusions, stridor, difficulty breathing, dysphagia, and odynophagia occurring within 24-h of the trauma were obtained from the medical records and were recorded.
Imaging protocols
CT examinations were obtained on 64-slice MDCT scanners with slice thickens of 0.625–1.5 mm (LightSpeed VCT; GE Healthcare with slice thickness 0.625–1.25 mm (n = 27); Revolution CT; GE Healthcare with slice thickness 1.25–1.5 mm (n = 26), and Force; Siemens with slice thickness 1.5 mm (n = 2)).
Non-contrast-enhanced CT neck or cervical spine images were helically acquired (120-kV/auto-mAs) at 1.25-mm-thick slices obtained from the level of the skull base to the thoracic inlet. Soft tissue and bone algorithms were available for review with 1.5–2-mm-thick/interval coronal and sagittal reconstructions.
CTA neck images were obtained from the level of the aortic arch through the superior orbital rim at 0.625–1.25-mm-thick slices (120-kVp/auto-mAs), following a dose of 80–100 mL of iohexol (Omnipaque, GE Healthcare) or iopamidol (Isovue, Bracco), 370 mgI/mL administered by a power injector at a rate of 4–5 mL/s. Coronal and sagittal reformats at 2-mm-thick slices were reconstructed.
Contrast-enhanced CT neck images were helically acquired (120-kVp/auto-mAs) at 1.25-mm-thick slices obtained following a 60-s delay following intravenous contrast administration (80–160 mL of iohexol or iopamidol, 370 mgI/mL) extending from the level of the skull base to the thoracic inlet. Soft tissue and bone algorithms were available for review with 2-mm-thick/interval coronal and sagittal reconstructions.
All CT examinations were obtained on patients within the first 12-h of presentation to the emergency department.
Imaging-based assessment
All exams were reviewed on a PACS system by subspecialty trained neuroradiologists, including a neuroradiologist with 5 years of practice in neuroradiology and subspecialty training in neuroradiology, and two neuroradiologists with greater than 20 years of practice in neuroradiology and head and neck imaging.
All patients’ exams were reviewed with reference made to clinical presentation, and physical exam findings noted for each patient, as documented in the electronic medical record. Additionally, the reviewers were aware of the mechanism of injury. Reference was made to the radiology report that was dictated at the time of scan acquisition; however, a full review and re-interpretation of the imaging findings pertinent to laryngeal trauma was performed for each exam.
As previously mentioned, patients with fracture deformities which were deemed not to be acute were excluded from this study. Factors which excluded patients from a suspected acute injury included (a) those with prior imaging demonstrating the same fracture pattern, (b) those with evidence of healing in the form of bony callus formation, (c) those with no findings to suggest overlying soft tissue injury and annotations in the electronic medical record reflecting non-acute symptoms based on clinical exam.
Soft tissue assessment
Soft tissue abnormalities were also recorded including the presence of supraglottic edema with non-focal hemorrhage, focal supraglottic hematoma, subglottic edema with non-focal hemorrhage, focal subglottic hematoma, soft tissue swelling and injury to the epiglottis, medialization of the vocal cord, and laceration to the pharynx and larynx. Focal supra- and subglottic hematomas were defined as a focal/mass-like collection with Hounsfield units above 25 HU. Non-focal hemorrhage with edema was defined as fluid which was non-mass-like and had Hounsfield units at or less than 25 HU. The frequency of hematoma involving the supraglottic larynx and the subglottic larynx was reported. Similarly, the frequency of supra- and subglottic edema with non-mass-like/non-focal hemorrhage was also reported for each patient. These patterns of soft tissue abnormality were correlated with the sites and patterns of fractures involving the hyoid bone, thyroid cartilage, and cricoid cartilage.
Laryngeal perforations and lacerations were determined by defects or disruption of the mucosa present on at least 3 consecutive CT slices with associated submucosal and subcutaneous foci of air.
The assessment for soft tissue abnormality was performed using soft tissue algorithm reconstructed images and assessed in the axial, coronal, and sagittal planes.
Fracture assessment
All CT images were reviewed for fractures involving the hyoid bone, thyroid cartilage, and cricoid cartilage. The assessment for fractures was performed using bone algorithm reconstructed images and assessed in the axial, coronal, and sagittal planes. A fracture was defined as a displaced or non-displaced lucency extending through the hyoid bone, thyroid cartilage, or cricoid cartilage present on at least 2 consecutive CT slices.
The locations of these fractures were recorded for each patient.
Fractures of the thyroid cartilage were categorized as horizontally or vertically oriented with respect to the axial plane. For fractures which had both vertical and horizontal components, these were recorded separately.
Cricoid cartilage fractures were classified as occurring through the posterior lamina, lateral aspect of the cricoid arch, or anterior/midline aspect of the cricoid arch. Lateral cricoid arch fractures were determined as those occurring greater than 0.75 cm lateral to the midplane of the cricoid cartilage in the axial plane. An assessment for cricothyroid dislocation was also performed.
Fractures were classified as single-site versus multi-site and were described as a percentage of frequency.
All images were retrospectively reviewed by at least two neuroradiologists and evaluations were based on consensus agreement.
Statistical analyses
Mann–Whitney U test or one-way analysis of variance was used to compare patient’s age and Fisher’s exact test was used to compare the frequency of clinical features (gender, type of trauma, mechanism of injury, symptom) between imaging findings (location of hematoma [supraglottic vs. subglottic], location of edema [supraglottic vs. subglottic], fracture site [hyoid bone vs. thyroid cartilage vs. cricoid cartilage], and number of fracture sites [single or. multi-site]). Fisher’s exact test was also used to compare the frequency of soft tissue abnormalities between the fracture site (hyoid bone vs. thyroid cartilage vs. cricoid cartilage] or the number of fracture site [single or multi-site]). A p value < 0.05 was considered significant in all analyses. All statistical analyses were performed using SPSS, version 23.0 (SPSS Inc.).
Results
Patient demographics and scan type
A total of 64 patients were identified through our PACS keyword search; however, 9 patients were subsequently excluded with 8 patients found to have chronic fractures based on prior imaging demonstrating the same fracture pattern and/or evidence of bony callus formation. An additional patient was excluded secondary to severe motion artifact precluding a diagnostic assessment.
Fifty-five patients were included with 47 men and 8 women, ranging in age from 18–77 years (mean 42.4 years, SD 15 years). Of the 55 patients who underwent neck or cervical spine CT, 25 patients (45%) had CTA, 19 patients (35%) had non-contrast-enhanced CT, and 11 patients (20%) had contrast-enhanced CT.
Mechanisms of injury
Motor vehicle accidents were the most common mechanism of injury (n = 17), followed by assault (n = 15) and falls (n = 7). Additional data describing the observed mechanisms of injury is displayed in Table 1. Most mechanisms of injuries were blunt trauma (n = 49) with four patients with penetrating injuries. Two patients were found down, and the mechanism of trauma was not able to be classified.
Soft tissue abnormalities
Supraglottic soft tissue abnormalities
Supraglottic edema with non-focal hemorrhage was associated with blunt injuries in 34 patients (70%) and 3 patients with penetrating injuries (Table 1).
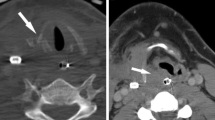
Focal supraglottic hematomas were more frequently seen in association with multi-site fractures compared to single-site fractures (83% versus 33%, p = 0.003) (Table 2). Focal supraglottic hematomas were seen in 24/55 patients with 19 (79%) occurring with thyroid cartilage fractures and 8 (33%) with cricoid fractures (Tables 1 and 2; Figs. 1, 2, and 3).
A 45-year-old man with neck pain and difficulty swallowing following a motor vehicle accident. Coronal CT image demonstrates extensive supraglottic edema (arrows) and focal hematoma (arrowheads). There is also a complex fracture through the thyroid cartilage with both vertical and horizontal components
Subglottic soft tissue abnormalities
All patients with subglottic edema and non-focal hemorrhage also had supraglottic edema. Subglottic edema with non-focal subglottic hemorrhage was seen in 22/55 patients and was significantly associated with a multi-site fracture pattern (p < 0.001) (Table 2) with 15/22 (75%) cases occurring in conjunction with thyroid cartilage fractures. Additionally, all patients with cricoid fractures (13 patients) had associated subglottic edema and non-focal hemorrhage (100%, p = 0.003).
Seventeen patients (85%) with subglottic edema and non-focal hemorrhage also had focal supraglottic hematomas. Focal subglottic hematomas were seen in 7/55 patients (13%). Focal subglottic hematomas were most frequently associated with cricoid cartilage fractures (38%, p < 0.001) (Table 2).
Perforations/lacerations
Six of 55 (11%) patients had perforations or lacerations of the larynx with 5/6 having documented blunt mechanisms of injury and 1 patient with an unknown mechanism of injury (Table 1). Neck pain and difficulty swallowing were the most common associated symptoms documented in 4/6 patients (67%). The remaining 2/6 patients were non-responsive upon presentation. The mean age of patients with perforations/lacerations was 48 years (SD 22 years).
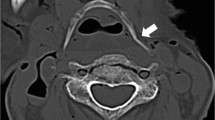
All 6 patients had associated thyroid cartilage fractures and multi-site fractures were encountered in 3/6 patients (50%), with one of the patients having fractures involving the thyroid cartilage and hyoid bone, and 2 patients with thyroid cartilage and cricoid cartilage fractures. Soft tissue abnormalities associated with these perforations/lacerations included supraglottic edema and non-focal hemorrhage in all patients, focal supraglottic hematomas in 5/6 patients (83%), subglottic edema with non-focal hemorrhage in 4/6 patients (67%), and subcutaneous emphysema in all patients (Fig. 4). Asymmetric thickening of a strap muscle was seen in approximately half of the patients.
A 34-year-old man with severe neck pain following a high-speed jet ski collision. a and b Axial CT images through the larynx are notable for subcutaneous emphysema related to a laryngeal penetration injury. A displaced, vertically oriented fracture involves the midline of the thyroid cartilage (white arrows), and a mildly displaced, vertically oriented fracture of the cricoid cartilage (arrowheads) is seen. Accompanying soft tissue abnormality includes supra- and subglottic edema and non-focal hemorrhage with extensive subcutaneous emphysema
Medialized vocal cord
Twelve out of 55 patients had medialization of one of the vocal cords; 11/12 patients had blunt traumatic injury (92%) with 1 patient having an unknown mechanism of injury.
All 12 patients had associated supraglottic edema with non-focal hemorrhage, 11/12(92%) of patients had subglottic edema with non-focal hemorrhage, and 10/12(83%) of patients had focal supraglottic hematomas. Asymmetric thickening of the ipsilateral strap muscle was seen in 9/12 (75%) of patients.
Thyroid cartilage fractures were most frequently associated with medialization of the vocal cord (9/12, 75%) followed by cricoid fractures in 7 patients (58%).
Fracture assessment
Hyoid fractures
Eight out of 55 patients (15%) had a hyoid bone fracture for which 3 of these 8 cases occurred as multi-site fractures. Of the 3 cases of multi-site fractures involving the hyoid bone, 2 occurred in conjunction with thyroid cartilage fracture, and 1 occurred in conjunction with a thyroid and cricoid cartilage fracture.
Thyroid cartilage fractures
Forty-eight patients (87%) had thyroid cartilage fractures (Fig. 1). Most were vertical in orientation, occurring in 36/48 (75%), with 6 being horizontal in orientation (13%). The remaining 6 patients (13%) had complex fractures containing both a horizontal and a vertical component.
Cricoid cartilage fractures
Thirteen patients (24%) had cricoid cartilage fracture of which 6 had fractures involving the posterior lamina of the cricoid cartilage, and 4 of these cases also occurred in conjunction with lateral arch fractures. Seven patients had only fractures involving the lateral arch of the cricoid cartilage. Seven patients had fractures involving more than 1 site of the cricoid cartilage (bilateral arch fractures, lateral arch fracture with lamina fracture), while 6 patients had a single-site of fracture involving the cricoid cartilage. None of the patients in this cohort had fractures involving the anterior/midline aspect of the cricoid cartilage.
Of the 13 patients with cricoid cartilage fractures, all had associated soft tissue findings, including 8 focal supraglottic hematoma, 11 supraglottic edema with non-focal hemorrhage, 5 focal subglottic hematoma, and 13 subglottic edema with non-focal hemorrhage (Fig. 2).
Additionally, none of the patients in this cohort demonstrated cricothyroid dislocation.
Multi-site fractures
Twelve out of 55 (22%) patients presented with multi-site fractures; 11 patients had a documented blunt trauma injury and one patient had no known mechanism of injury (Table 3).
In patients with multi-site fractures, 11 thyroid cartilage fractures were noted; 9 occurred in associated with a cricoid cartilage fracture and 3 occurred with a hyoid bone fracture. One patient had a hyoid bone fracture with a cricoid cartilage fracture without the presence of a thyroid cartilage fracture.
Most patients with multi-site fractures had associated focal supraglottic hematomas (10 patients, 83%), supraglottic edema with non-focal hemorrhage (11 patients, 92%), and subglottic edema and non-focal hemorrhage (10 patients, 83%). Focal subglottic hematomas were only seen in 5 patients (42%) (Table 3).
Single-site fractures
Forty-three out of 55 (78%) patients presented with single-site fractures; 38 patients had documented blunt trauma injury, 4 patients had penetrating injury, and one patient had no known mechanism of injury (Table 3).
Thirty-four isolated thyroid cartilage fractures, 5 isolated hyoid bone fractures, and 4 isolated cricoid cartilage fractures were noted.
Fractures with no associated soft tissue abnormality
A total of 13 patients had fractures with no associated discernible soft tissue abnormality. These included 1 patient with an isolated hyoid bone fracture and 12 patients with isolated thyroid fractures.
Discussion
Most of the imaging literature on traumatic injuries of the larynx is in the form of educational manuscripts describing imaging features of laryngeal trauma and small case reports [6,7,8,9,10,11,12, 14,15,16,17,18,19,20]. This study bridges current gaps in knowledge describing the relative frequency of fractures involving the hyoid bone, thyroid cartilage, and cricoid cartilage in patients with acute laryngeal trauma, as well as the frequency of fracture patterns and associated patterns of soft tissue abnormalities.
It is important for practicing radiologists to be aware of laryngeal fracture patterns and associated soft tissue abnormalities for the prompt diagnosis of these injuries. There is an associated estimated mortality rate of traumatic laryngeal injuries between 1 and 13% and a morbidity rate of up to 37% in these patients in the absence of other significant systemic injuries [5, 21].
The results of this dual institution retrospective study are concordant with previously published literature on this topic, noting a higher prevalence of laryngeal fractures occurring in men, predominately from blunt trauma mechanisms, with motor vehicle accidents and assaults being the most commonly reported mechanisms of injury in our cohort. These findings may be related to a higher tendency of men to engage in riskier behavior compared to women [22]. The increased incidence of laryngeal fractures in men may potentially be related to anatomic considerations such as the larger projection of the thyroid cartilage, the larger size of the larynx, and higher rigidity of the cartilage in men compared to women.
It is important to highlight that both isolated laryngeal fractures as well as multi-site fractures were encountered in our study. Thyroid cartilage fractures were the most frequently fractured site occurring in 80% of patients, followed by cricoid fractures in 24% of patients. Multi-site fracture patterns most frequently involved thyroid and cricoid cartilage fractures in 72% of patients of multi-site fractures.
Associated soft tissue abnormalities were more frequent with multi-site fractures noting focal supraglottic hematomas in 82% of patients, supraglottic edema with non-focal hemorrhage in 91% of patients, and subglottic edema with non-focal hemorrhage (82%) and focal subglottic hematoma (46%). Focal subglottic hematomas were significantly associated with multi-site fractures involving the cricoid cartilage. Subglottic edema with non-focal hemorrhage was significantly more frequently associated with cricoid cartilage fractures and multi-site fracture patterns.
Laryngeal perforations and lacerations were less common and occurred in 11% of patients (6/55), mostly occurred with blunt trauma mechanisms, and always occurred with thyroid cartilage fractures.
All patients in this cohort with cricoid fractures had associated soft tissue abnormalities. Perhaps the absence of supra- or subglottic hematoma and edema with non-focal hemorrhage can be utilized as a reassuring sign for intact cricoid cartilage in the setting of traumatic laryngeal injury; however, this observation would need to be further investigated in a larger cohort.
Fractures of the laryngeal structures are often subtle and may be overlooked in the setting of a major traumatic injury; however, knowledge of frequent laryngeal fracture patterns may help practicing radiologists identify all injuries involving the osseous and cartilaginous structures of the larynx. Additionally, knowledge of patterns of soft tissue abnormality associated with fracture patterns may be an additional clue for radiologists for the accurate and comprehensive description of laryngeal trauma.
This study has several limitations. It is a small sample size despite inclusion from two level I trauma institutions spanning an 18-year period. This is reflective of the relatively rare incidence of laryngeal trauma and laryngeal fractures. This study was performed as a retrospective study design rather than a prospective evaluation. Patients were identified for inclusion into this study based on a keyword search in the PACS system. This may potentially introduce a selection bias based on this keyword recognition. Given the extensive number of studies acquired at our two institutions over the past 18 years, it was not feasible to review all trauma studies performed over this interval to identify patients with acute laryngeal trauma and fractures which may have been missed on initial interpretation or may have been overlooked by the clinical team based on other sites of severe traumatic injury. Data was collected from two level I trauma institutions within the same city, and scanning protocols varied slightly between institutions. While this heterogeneity in CT scan type is not ideal, it is reflective of trauma severity, concern for additional sites of injury, including vascular structures, and may also reflect some degree of variations in practice patterns. There were varied degrees of ossification involving the cartilaginous structures of the larynx encountered in our patient population. For patients with little-to-no ossification of these structures, the assessment for a fracture is perhaps more difficult and may potentially be underestimated. Additionally, the classification of focal hematoma versus non-focal hematoma with edema may not be accurate in all cases. The classification “hematoma” was reserved focal mass-like foci of hemorrhage with Hounsfield units greater than 25. Non-focal hematoma with edema was reserved for other cases of lower density fluid. We recognize that the time from the initial trauma to imaging varied amongst patients. Additionally, lower Hounsfield units would occur when hemorrhage is mixed with low density edema in the setting of trauma.
In conclusion, it is important for practicing radiologists to be aware of the frequency of isolated and multi-site laryngeal fractures and patterns of soft tissue abnormality for recognition of these injuries and decreasing morbidity associated with breathing, swallowing, and phonation difficulties. The patterns of soft tissue abnormality may help direct clinicians to scrutinize adjacent cartilaginous structures of the larynx to identify subtle fractures.
Abbreviations
- CT:
-
Computed tomography
- CTA:
-
Computed tomography angiogram
- MDCT:
-
Multidetector-row CT
- PACS:
-
Picture archiving and communication systems
References
Eliachar I (1996) Management of acute laryngeal trauma. Acta Otorhinolaryngol Belg 50:151–158
Bent JP III, Silver JR, Porubsky ES (1993) Acute laryngeal trauma: a review of 77 patients. Otolaryngol Head Neck Surg 109:1–9
Schaefer SD (1992) The acute management of external laryngeal trauma. A 27-year experience. Arch Otolaryngol Head Neck Surg 11:598–604
Madani A, Pecorelli N, Razek T, Spicer J, Ferri LE, Mulder DS (2016) Civilian airway trauma: a single-institution experience. World J Surg 40:2658–2666
Lee WT, Eliashar R, Eliachar I (2006) Acute external laryngotracheal trauma: diagnosis and management. Ear Nose Throat J 85:179–184
Kuniyoshi Y, Kamura A, Yasuda S, Tashiro M, Toriyabe Y (2017) Laryngeal injury and pneumomediastinum due to minor blunt neck trauma: case report. J Emerg Med 52:e145–e148
Trinidade A, Shakeel M, Stickle B, Ah-See KW (2015) Laryngeal fracture caused by a lacrosse ball. J Coll Physicians Surg Pak 25:843–844
Becker M, Leuchter I, Platon A, Becker CD, Dulguerov P, Varoquaux A (2014) Imaging of laryngeal trauma. Eur J Radiol 83:142–154
Narcı A, Embleton DB, Ayçiçek A, Yücedağ F, Cetinkurşun S (2011) Laryngeal fracture due to blunt trauma presenting with pneumothorax and pneumomediastinum. ORL J Otorhinolaryngol Relat Spec 73:246–248
Fitzsimons MG, Peralta R, Hurford W (2005) Cricoid fracture after physical assault. J Trauma 59:1237–1238
Chowdhury R, Crocco AG, El-Hakim H (2005) An isolated hyoid fracture secondary to sport injury. A case report and review of literature. Int J Pediatr Otorhinolaryngol 69:411–414
Humenansky KM, Harris TM, Hoffman DM (2017) Laryngotracheal separation following blunt neck trauma. Am J Emerg Med 35:669.e5–669.e7
Kragha KO (2015) Acute traumatic injury of the larynx. Case Rep Otolaryngol 2015:393978
Becker M, Duboé PO, Platon A et al (2013) MDCT in the assessment of laryngeal trauma: value of 2D multiplanar and 3D reconstructions. AJR Am J Roentgenol 201:W639–W647
Kuttenberger JJ, Hardt N, Schlegel C (2004) Diagnosis and initial management of laryngotracheal injuries associated with facial fractures. J Craniomaxillofac Surg 32:80–84
Shi J, Uyeda JW, Duran-Mendicuti A, Potter CA, Nunez DB (2019) Multidetector CT of laryngeal injuries: principles of injury recognition. Radiographics 39:879–892
Robinson S, Juutilainen M, Suomalainen A, Makitie A (2009) Multidetector row computed tomography of the injured larynx after trauma. Semin Ultrasound CT MR 30:188–194
Parida PK, Gupta AK (2008) Role of spiral computed tomography with 3-dimensional reconstruction in cases with laryngeal stenosis-a radioclinical correlation. Am J Otolaryngol 29:305–311
Sethi RKV, Khatib D, Kligerman M, Kozin ED, Gray ST, Naunheim MR (2019) Laryngeal fracture presentation and management in United States emergency rooms. Laryngoscope 129:2341–2346
Gussack GS, Jurkovich GJ, Luterman A (1986) Laryngotracheal trauma: a protocol approach to a rare injury. Laryngoscope 96:660–665
Jewett BS, Shockley WW, Rutledge R (1999) External laryngeal trauma analysis of 392 patients. Arch Otolaryngol Head Neck Surg 125:877–880
Eaton DK, Kann L, Kinchen S et al (2012) Youth risk behavior surveillance-United States, 2011. MMWR Surveill Summ 61:1–162
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Osamu Sakai.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buch, K., Takumi, K., Curtin, H.D. et al. CT-based assessment of laryngeal fracture patterns and associated soft tissue abnormality. Eur Radiol 31, 5212–5221 (2021). https://doi.org/10.1007/s00330-020-07548-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07548-4