Abstract
Objectives
To retrospectively examine US, CT, and MR imaging examinations of missed or misinterpreted pancreatic ductal adenocarcinoma (PDAC), and identify factors which may have confounded detection or interpretation.
Methods
We reviewed 107 examinations in 66/257 patients (26%, mean age 73.7 years) diagnosed with PDAC in 2014 and 2015, with missed or misinterpreted imaging findings as determined by a prior study. For each patient, images and reports were independently reviewed by two radiologists, and in consensus, the following factors which may have confounded assessment were recorded: inherent tumor factors, concurrent pancreatic pathology, technical limitations, and cognitive biases. Secondary signs of PDAC associated with each examination were recorded and compared with the original report to determine which findings were missed.
Results
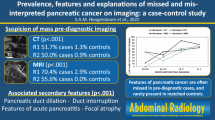
There were 66/107 (62%) and 49/107 (46%) cases with missed and misinterpreted imaging findings, respectively. A significant number of missed tumors were < 2 cm (45/107, 42%), isoattenuating on CT (32/72, 44%) or non-contour deforming (44/107, 41%). Most (29/49, 59%) misinterpreted examinations were reported as uncomplicated pancreatitis. Almost all examinations (94/107, 88%) demonstrated secondary signs; pancreatic duct dilation was the most common (65/107, 61%) and vascular invasion was the most commonly missed 35/39 (90%). Of the CT and MRIs, 28 of 88 (32%) had suboptimal contrast dosing. Inattentional blindness was the most common cognitive bias, identified in 55/107 (51%) of the exams.
Conclusion
Recognizing pitfalls of PDAC detection and interpretation, including intrinsic tumor features, secondary signs, technical factors, and cognitive biases, can assist radiologists in making an early and accurate diagnosis.
Key Points
• There were 66/107 (62%) and 49/107 (46%) cases with missed and misinterpreted imaging findings, respectively, with tumoral, technical, and cognitive factors leading to the misdiagnosis of pancreatic ductal adenocarcinoma.
• The majority (29/49, 59%) of misinterpreted cases of pancreatic ductal adenocarcinoma were mistaken for pancreatitis, where an underlying mass or secondary signs were not appreciated due to inflammatory changes.
• The most common missed secondary sign of pancreatic ductal adenocarcinoma was vascular encasement, missed in 35/39 (90%) of cases, indicating the importance of evaluating the peri-pancreatic vasculature.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is a devastating disease with a poor prognosis, often related to the advanced stage at diagnosis [1]. The 7% 5-year survival is the lowest of any solid malignancy, and it is projected to become the second leading cause of cancer-related death in the next decade [2, 3]. Surgical resection is the only curative treatment; however, more than half of patients with PDAC present with disseminated, advanced stage disease and are ineligible for surgery [4].
The clinical diagnosis of PDAC is challenging. Patients often present with non-specific symptoms, and up to one-third of patients are misdiagnosed clinically [5]. Because patients with PDAC that are initially misdiagnosed are associated with a higher risk of advanced disease at the time of diagnosis, early detection is essential for improving patient outcomes [5,6,7].
Imaging plays a crucial role in the diagnosis and staging of PDAC. In our experience, radiologists are often the first physician to raise the possibility of pancreatic malignancy. However, the imaging diagnosis of PDAC can be challenging. Imaging findings are often subtle, particularly when tumors are small or non-contour deforming or when there is a lack of pancreatic or biliary duct dilation. Tumors may be isoattenuating, with little contrast difference between tumor and normal pancreatic parenchyma [8]. Vascular involvement can be difficult to detect or differentiate from changes related to pancreatitis. Because of these challenges, the early imaging manifestations of pancreatic cancer can be missed, and diagnosis may be delayed. Indeed, studies have shown that subtle early imaging findings of PDAC, such as pancreatic duct dilation and abrupt cutoff, are often present on imaging examinations up to 18 months before the date of ultimate diagnosis [9,10,11,12].
Recently, we performed a retrospective study evaluating the extent and implications of imaging-related delays to diagnosis of PDAC [13]. In the process of reviewing US, CT, and MR imaging examinations of patients included in that study, we identified key tumoral, imaging, and cognitive factors related to cases where the diagnosis of PDAC was missed or misinterpreted. Because early detection is key to improving outcomes of patients with PDAC, the purpose of this article is to highlight factors that may have confounded detection of PDAC.
Methods
As part of our initial study and with ethics approval, we retrospectively reviewed the US, CT, and MRI examinations of 257 patients (mean age 71.8 years) diagnosed with PDAC in 2014 and 2015 [13]. Patients were identified by the Nova Scotia Cancer Registry. For each patient, the relevant images and reports performed within 5 years prior to the date of diagnosis were independently reviewed by two board-certified, fellowship-trained abdominal radiologists AFC and SEC. The radiologists used the 1–3 RADPEER scoring system from the American College of Radiology, which corresponds to the following definitions: score 1, concur with interpretation; score 2, discrepancy in interpretation but “an understandable miss”; and score 3, discrepancy in interpretation that would have been expected to be made [14]. Discrepancies in RADPEER scores between the two radiologists were resolved in consensus.
In this study, 107 examinations scored as RADPEER 2 or 3 from 66 patients (mean age 73.7 years) were re-assessed by the radiologists for any potential factors that may have confounded assessment of PDAC. This was done independently and then discrepancies were resolved in consensus. Note was made whether there was an issue with detection of findings, interpretation, or both. Of the misinterpreted cases, the reported diagnosis or differential diagnosis was recorded. Inherent tumor factors which may have confounded detection, such as small size (< 2 cm), isoattenuating tumors, non-contour deforming tumors, uncinate process tumors, and absence of secondary signs of PDAC, were recorded. The radiologists recorded the following secondary signs of PDAC for each case: vascular encasement; abrupt duct cutoff; loss of fatty atrophy; parenchymal atrophy; contour deformity (loss of the normal lobulation of the pancreas); duct dilation (main pancreatic duct dilated over 3 mm); and acute pancreatitis (defined as peri-pancreatic stranding and parenchymal edema). The radiologists’ findings were then compared with the report to determine which findings were missed. Any concurrent pancreatic pathology such as pseudocysts or intraductal papillary mucinous neoplasm (IPMN) was noted.
The following technical limitations were noted: imaging artifacts (motion artifact, streak artifact from positive oral contrast, and quantum mottle due to patient body habitus); poor or absent contrast enhancement (CT and MRI); and type of examination (CT chest, CT angiogram, unenhanced CT, CT abdomen and pelvis in the portal venous phase, CT pancreatic protocol, MR pancreatic and delayed phase, MRCP). Slice thickness were categorized for CT and MRI as either standard (3 mm or thinner) or substandard (over 3 mm) for contrast-enhanced phases according to the National Comprehensive Cancer Network Guidelines for optimal pancreatic imaging [15]. When contrast enhancement sequences were not available for MRI, T2 SSFSE sequence was used to assess slice thickness, with standard thickness of less than 6 mm [15]. Lastly, the radiologists noted whether any of the following cognitive biases may have affected interpretation: exams where PDAC was an incidental finding, based on the clinical history and type of imaging exam, as well as examinations where PDAC was identified on the last few images of a stack, or in the peripheral field of view (inattentional blindness); presence of concurrent extrapancreatic pathology (satisfaction of search); satisfaction of report (alliterative bias); and examinations where the impression of the exam was discordant with the provided clinical context (anchoring bias).
Results
A summary of imaging examinations is provided in Table 1. There were 66/107 (62%) examinations with missed findings and 49/107 (46%) examinations with misinterpreted findings. Of the misinterpreted examinations (Table 2), the majority 29/49 (59%) were reported as uncomplicated pancreatitis, where the underlying mass was not appreciated prospectively, but in retrospect evident. Other cases were misinterpreted as a pseudocyst (2/49, 4%) and IPMN (5/49, 10%) (Fig. 1).
An 82-year-old male with pancreatic ductal adenocarcinoma presenting with swelling and pain in his right abdomen. a, b Axial contrast-enhanced CT images in the portal venous phase show a hypoenhancing solid mass in the tail of the pancreas (arrow). There is invasion of the splenic vein by the tumor (b, arrowhead) which resulted in peri-gastric collaterals (not shown). The vascular findings were missed, and the solid pancreatic tail lesion was reported as an intrapapillary mucinous neoplasm (RADPEER 3). Follow-up in 6 months was recommended. c Axial contrast-enhanced CT in the portal venous phase performed 6 months after the examination in a and b shows interval increased size of the hypoenhancing mass with progression of local invasion, now extending to the left adrenal gland, which was reported by the interpreting radiologist (arrow). The patient underwent Whipple’s and left adrenalectomy for a T3N1 moderately differentiated pancreatic adenocarcinoma and received adjuvant chemotherapy. The patient passed away 2 years later from metastatic PDAC
Nearly half of the missed and misinterpreted exams had intrinsic tumor features potentially confounding detection of PDAC (Table 3): 44/107 (41%) of cases were non-contour deforming; 45/107 (42%) of cases had tumor sizes less than 2 cm; and 32/72 CTs (44%) were isoattenuating. Tumors arising from the uncinate process were seen in 14/107 (13%) of cases (Fig. 2).
A 78-year-old male with pancreatic ductal adenocarcinoma presenting with epigastric pain and white blood cell count of 19 × 109/L. a Coronal and (b) axial contrast-enhanced CT images in the portal venous phase show abnormal bulky contour of the pancreatic head and uncinate process (arrows) compared with the rest of the pancreatic parenchyma. There is no pancreatic duct dilation. The examination was reported as normal by the original interpreting radiologist (RADPEER 3). No acute pathology to account for the patient’s elevated white blood cell count was identified. c Coronal contrast-enhanced CT image in the portal venous phase was performed 7 months later when the patient presented with jaundice. There is interval enlargement of the mass at the uncinate process (arrow) with pancreatic duct dilation (arrowhead) and intrahepatic duct dilation. The patient had hepatic and lymph node metastasis (not shown), which precluded surgical resection. The patient received palliative chemotherapy and died 8 months later
Shown in Table 4 is a summary of secondary signs that were observed on a retrospective review, and how often these were missed prospectively. Importantly, almost all cases (94/107, 88%) demonstrated secondary signs of PDAC. The most common missed secondary finding was vascular encasement; this was retrospectively observed in 39/107 (36%) of cases, but went unreported in most instances (35/39, 90%). Pancreatic duct dilation and abrupt duct cutoff were the most commonly present secondary signs, seen in 65/107 (61%) and 59/107 (55%) of cases, respectively; these were missed in 28/65 (43%) and 42/59 (71%) of instances, respectively (Fig. 3). Other commonly missed secondary signs were loss of fatty atrophy (11/17, 65%), parenchymal atrophy (9/14, 64%), and contour deformity (23/47, 49%). Pancreatitis was seen in 29/107 (27%) cases, and other concurrent pancreatic pathologies, such as IPMNs and pseudocysts, were identified in 14/107 (13%) of cases.
A 58-year-old male with pancreatic ductal adenocarcinoma presenting with abdominal discomfort. a, b The same axial contrast-enhanced CT image in the portal venous phase is shown with respective window width and level settings of (a) 350 and 50 and (b) 116 and 108. The pancreas was reported as normal (RADPEER 3); however in retrospect, there is a subtle hypoenhancing mass at the pancreatic body (arrows) with duct dilation, abrupt duct cutoff, and mild peri-pancreatic stranding. Note how much more conspicuous the mass is in b using a narrower window and higher level. c Axial contrast-enhanced CT image performed 5 months later for unintentional 20 lb. weight loss shows progression of the PDAC, with invasion of the celiac axis (arrow), rendering the patient unresectable. There is peri-pancreatic stranding around the tail in keeping with secondary pancreatitis. The patient received palliative chemotherapy and died 9 months after the initial examination
Suboptimal intravenous contrast media (CM) dosing, owing to unenhanced exams or low contrast dose, was observed in 23/88 (26%) and 28/88 (32%) of CTs and MRIs, respectively (Fig. 4). A dedicated pancreatic CT protocol was used in only 9 cases out of 72 (13%) (Table 3). The majority (39/72, 54%) of CT cases were uniphasic examinations in the portal venous phase.
A 47-year-old female with pancreatic ductal adenocarcinoma, unable to eat, emesis, 100 lb. weight loss for 3 months. a Axial contrast-enhanced CT image in the portal venous phase with suboptimal low IV contrast media dose of 321 mg of iodine per kilogram. There is a small, ill-defined region of hypoattenuation in the pancreatic head near the pancreaticoduodenal groove (arrow) which was missed on the initial CT. Prior to the CT, the patient had multiple trips to the emergency department resulting in trial of reflux medications with no relief. As no cause for the patient’s symptom was identified, the patient had a small bowel follow-through study, where persistent stricturing involving the 2nd portion of the duodenum was seen. A repeat CT was recommended. b Axial and (c) coronal contrast-enhanced CT image in the portal venous phase performed 6 weeks after the examination in a, with administration of oral water, 2 packets of gas granules, and optimal dosing of intravenous iodinated contrast at 516 mg of iodine per kilogram. A pancreatic head mass is seen to much better advantage (arrows), with invasion of the duodenum and obstruction of the stomach and first duodenal segment (arrowhead). Note the difference in depiction of the gastroduodenal mucosal and hypoenhancing pancreatic head mass as compared with the image in a. The patient underwent surgical resection and was found to have moderately differentiated pancreatic ductal adenocarcinoma, T3N1. The patient received chemotherapy and died 2 years after her initial exam
Suboptimal slice thickness was identified in 56/72 (78%) cases and 15/16 (94%) cases for CT and MRI, respectively. DWI sequence was not included in 6 out of 16 MRI cases (40%). A dedicated MRI of the pancreas was seen in most of the cases (12/16, 75%). There were a small number (6/88, 7%) of CT and MRI examinations that were confounded by imaging artifact (Table 3).
A total of 155 potential instances of cognitive biases were identified. Of the 55/107 (51%) cases where inattentional blindness was recorded, most (41/55, 75%) were considered incidental to the study indication. A total of 14/107 (13%) of cases were identified in the peripheral field of view, including three US examinations which, in retrospect, demonstrated a mass arising from the pancreatic tail on images of the spleen (Fig. 5). Of the 14 cases of PDAC identified in the peripheral view of the exam, ten PDACs (71%) were identified in the inferior-most images of a CT chest.
A 75-year-old male with pancreatic ductal adenocarcinoma presenting with newly diagnosed diabetes mellitus, abdominal pain, and weight loss. a Ultrasound image of the spleen shows a hypoechoic lesion at the splenic hilum (arrow), which was missed by the interpreting radiologist (RADPEER score of 3). Images of the pancreas proper were poor due to overlying bowel gas. An outpatient CT was recommended to further characterize multiple hypoechoic hepatic lesions (not shown). b Axial contrast-enhanced CT image in the portal venous phase obtained 3 weeks after the examination in a shows a hypoenhancing mass at the pancreatic tail (arrow), corresponding to the lesion seen at the splenic hilum on the ultrasound. Due to the presence of liver metastases, the patient was ineligible for surgery and underwent chemotherapy and radiation therapy and died 7 months later
There were 27/107 (25%) cases of potential alliterative bias, where the reported impression was propagated from the previous imaging examination. The most common example was misinterpretation of PDAC as pancreatitis (Fig. 6).
A 78-year-old male with pancreatic ductal adenocarcinoma presenting with epigastric pain for 4 months, 15 lb. weight loss and weakness. a Axial and (b) coronal contrast-enhanced CT images in (a) arterial and (b) portal venous phases. Shown in a is infiltrative soft tissue encasement and fat stranding around the SMA (arrow). Most of the stranding is centered around the vessel, rather than the pancreatic parenchyma. b There is obliteration of the portal confluence, splenic vein, and SMV, resulting in cavernous transformation of the main portal vein (arrow) and peri-gastric collaterals (arrowhead). These findings were reported by the radiologist but the CT was misinterpreted as pancreatitis, despite the patient presenting with a normal lipase and symptoms suspicious for malignancy (RADPEER 3). The imaging diagnosis of PDAC was made on MRI 1 month later (not shown), which was requested due to “elevated CA 19-9 and CT findings of pancreatitis without supporting biochemical evidence” as noted on the requisition. The patient died 6 weeks thereafter
There were 22/107 (21%) potential cases where the radiological impression was incongruent with the clinical presentation of the patient. For example, the clinical information provided was suspicious for malignancy, such as new-onset diabetes or weight loss, but only benign entities such as uncomplicated acute pancreatitis were reported (Fig. 6).
Discussion
In this study, we retrospectively assessed 107 imaging examinations with missed or misinterpreted imaging findings of PDAC to identify potential factors and lessons for radiologists. The discussion below is organized as follows: (1) intrinsic tumor features; (2) secondary signs; (3) concurrent pathology; (4) technique; and (5) cognitive biases.
Intrinsic tumor features
Tumors that are small (< 2 cm), isoattenuating, or non-contour deforming can confound detection. Detection of PDAC when small is beneficial to patient outcomes because small tumors are slowly growing and less frequently metastatic than larger tumors [16]. The proportion of isoattenuating tumors in our study (44%) is higher than previously reported (11% in ref. [11]), likely because our study only assessed missed and misinterpreted cases of PDAC. Interestingly, the prevalence of isoattenuating pancreatic cancer has been shown to be higher in small and well-differentiated tumors and has been associated with better patient survival after curative intent surgery [22, 17]. The more favorable survival of isoattenuating and small PDAC reinforces the importance of detecting these subtle tumors via primary and secondary imaging signs [16, 17].
Uncinate process tumors are also challenging to detect and carry a significantly higher incidence of superior mesenteric artery encasement and peri-neural invasion compared with pancreatic head tumors [18]. Due to their anatomic location away from the pancreatic duct, uncinate tumors less commonly cause duct dilation and parenchymal atrophy [19]. Findings that may assist detection include loss of the normal feathery pancreatic contour and focal loss of fatty atrophy (Fig. 2). Any change in the normal biconcave margin of the uncinate process should be viewed with suspicion [20].
The use of different window widths and levels is crucial to detect subtle pancreatic tumors: particularly small, isoattenuating or non-contour deforming tumors or in cases of contrast media (CM) underdosing. Shown in Fig. 3 is a small tumor which is near inconspicuous on routine soft tissue windows, but more conspicuous on narrow window settings [21].
Secondary signs
In our study, most cases demonstrated secondary signs of PDAC. This is in agreement with the literature; one study found secondary signs in 88% of tumors 2 cm or smaller, and 100% of tumors measuring 2.1–3 cm [22]. Secondary signs are therefore highly useful for tumor detection [22]. Because PDAC arises from ductal epithelium, pancreatic and common bile duct obstruction is more commonly seen than with other pancreatic tumors [23, 24].
Pancreatic duct abnormalities were the most common secondary signs, which also agrees with results from previous studies [9, 11, 12, 22, 25]. One study found that 20/35 (57%) of PDAC tumors demonstrated pancreatic duct dilation prior to the primary mass being evident on CT [26]. Other studies have found that pancreatic duct dilation may be evident over 18 months before the diagnosis is made [9, 12].
Another important secondary finding is vascular invasion, which was the most commonly missed secondary finding in our study (Fig. 1). Although vascular narrowing, thrombosis, and pseudoaneurysms can develop from pancreatitis, vascular invasion, where infiltrative soft tissue encases the vessel, should be considered highly suspicious for malignancy. Our results and the literature indicate that secondary findings, and in particular abnormalities of the pancreatic duct and vasculature, are critical to detecting early and subtle PDAC tumors (Fig. 3). Assessing patency of the peripancreatic vasculature can not only help detect small but locally invasive tumors, but also is important for local staging.
Concurrent pancreatic pathology
The majority of misinterpreted examinations in our study were reported as uncomplicated pancreatitis (Fig. 6). Approximately 2.6 to 13.8% of patients with PDAC present with acute pancreatitis [27]. Pancreatitis presents a challenge with respect to the imaging diagnosis and staging of PDAC for two reasons: first, PDAC can be misinterpreted as acute pancreatitis, and pancreatitis, particularly mass-forming pancreatitis, can be mistaken for malignancy. Second, inflammatory changes can mimic locally invasive disease, limiting assessment of resectability [1].
Some clinical and imaging features may help distinguish between pancreatitis and PDAC. Several studies have shown an association between new-onset diabetes (defined as within 2 years of PDAC diagnosis) in patients with PDAC [28, 29] when compared with controls without PDAC [30]. According to the American College of Gastroenterology guidelines, patients over 40 with idiopathic pancreatitis should undergo contrast-enhanced CT or MRI to assess for a pancreatic neoplasm, especially if the patient’s course is prolonged or recurrent [31].
On imaging, findings that favor malignancy include the double duct sign, loss of normal fatty atrophy, and changes to the peripancreatic vessels, including stricturing with caliber change, and lumen deformity [32, 33]. Circumferential soft tissue cuff or stranding around a vessel, with loss of the perivascular fat plane, is indicative of vascular invasion [34]. Although perivascular stranding can represent inflammatory changes from pancreatitis [35], a location centered around the vasculature, rather than the pancreatic parenchyma, favors vascular or perineural tumoral invasion [34] (Fig. 6).
Imaging technique
The most important technical issues identified in our study were (1) examinations that were not dedicated to imaging the pancreas, (2) suboptimal slice thickness, (3) lack of DWI, (4) intravenous contrast dosing, and (5) image artifacts. One of the problems with the diagnosis of PDAC is that patients often present with non-specific signs and symptoms [5]; as such, they may be imaged with different modalities and protocols. With respect to slice thickness, guidelines are set forth by the National Comprehensive Cancer Network, which recommends slice thickness of less than 3 mm for CT, and less than 2–3 mm for MRI pre and dynamic post IV contrast administration sequence [15]. This is crucial not only for the diagnosis of PDAC, but also for local staging. A minority of MRIs did not include DWI; however, DWI provides valuable sensitivity for identifying tumors and can be helpful in differentiating benign from malignant processes [32, 36].
In our experience, sufficient intravenous CM dosing is critical for detection and staging of PDAC on CT and MRI. Ideally, dosing should be according to a patient’s weight, which is the main physiologic parameter affecting parenchymal enhancement [37]. As PDAC is typically hypoenhancing to the background pancreas, soft tissue contrast between tumor and normal pancreas is maximized by administering a liberal dose of CM. For CT, experts recommend a dose of 400–600 mg of iodine per kilogram of body weight to achieve optimal enhancement of the liver and pancreas [37,38,39].
Other methods to improve the CT technique include ingestion of neutral oral contrast (water), which enhances assessment of periampullary and pancreatic head lesions by distending the stomach and duodenum (Fig. 4). One of the artifacts identified in our study included streak artifact from the use of positive oral contrast. This is not recommended in pancreatic imaging as beam hardening artifact from pooled contrast in the stomach or duodenum can obscure pancreatic or periampullary pathology [38, 40].
Cognitive biases
Cognitive biases influence radiologic decision-making and can result in medical errors or adverse patient outcomes [41]. The most common potential cognitive error was inattentional blindness, also known as tunnel vision or scrolling error, which represents a finding missed because of its location, or a missed unexpected finding [41] (Fig. 5). A systematic approach to reviewing examinations, perhaps with use of a structured report, can help ensure that no area is missed. Since the completion of our study, we have modified out reporting of the pancreas on ultrasound, adding comment on visualization of the pancreas and diagnostic certainty to the reports.
Not considering the clinical context is a cognitive error related to anchoring bias. In this pitfall, radiologists remain fixed to an initial diagnostic impression without considering additional information, such as the clinical context of the patient [41]. Examples included a history of new-onset diabetes or weight loss, but only benign pathology such as acute pancreatitis was reported. Patient symptoms, duration of symptoms, relevant bloodwork, and potential causes should be sought when considering a diagnosis of pancreatitis (Fig. 6).
Limitations
Our study had limitations, including its retrospective nature and evaluation of a defined population within a single healthcare system, which may limit generalizability. We identified potential imaging factors and cognitive biases; however, these were inferred based on our review of the imaging examinations and radiology reports. It is important to note that one cannot know what was (or were) the causative factor(s) that ultimately led to a tumor being missed or misinterpreted, nor is the interplay between factors known, that is, the relative strength of each factor. We found that a large proportion of CTs in our study were not optimized for detection of pancreatic abnormalities with a dedicated protocol—itself a major pitfall in PDAC detection—which may have confounded assessment for specific imaging features. However, our study reflects the historical practice across multiple centers, and demonstrates how dedicated pancreatic imaging is often not performed in patients ultimately diagnosed with PDAC.
Conclusion
Radiologists play an integral role in the diagnosis of PDAC and early, accurate diagnosis is crucial for improving survival of this highly fatal disease. In this study, we retrospectively reviewed 107 examinations of missed or misinterpreted PDAC on US, CT, and MRI to identify key tumoral, imaging, and cognitive factors which may confound radiologist detection or interpretation of PDAC. Recognizing imaging pitfalls of PDAC can assist radiologists in diagnosing PDAC, which in turn can improve patient survival.
Abbreviations
- CM:
-
Contrast media
- IPMN:
-
Intraductal papillary mucinous neoplasm
- PDAC:
-
Pancreatic ductal adenocarcinoma
References
Zins M, Matos C, Cassinotto C (2018) Pancreatic adenocarcinoma staging in the era of preoperative chemotherapy and radiation therapy. Radiology 287:374–390
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74:2913–2921
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
National Cancer Institute (2019) SEER Cancer Stat Facts: Pancreatic Cancer. https://seer.cancer.gov/statfacts/html/pancreas.html. Accessed 18 Feb 2020
Swords DS, Mone MC, Zhang C, Presson AP, Mulvihill SJ, Scaife CL (2015) Initial misdiagnosis of proximal pancreatic adenocarcinoma is associated with delay in diagnosis and advanced stage at presentation. J Gastrointest Surg 19:1813–1821
Gobbi PG, Bergonzi M, Comelli M et al (2013) The prognostic role of time to diagnosis and presenting symptoms in patients with pancreatic cancer. Cancer Epidemiol 37:186–190
Egawa S, Takeda K, Fukuyama S, Motoi F, Sunamura M, Matsuno S (2004) Clinicopathological aspects of small pancreatic cancer. Pancreas 28:235–240
Takeshita K, Kutomi K, Haruyama T et al (2010) Imaging of early pancreatic cancer on multidetector row helical computed tomography. Br J Radiol 83:823–830
Gangi S, Fletcher JG, Nathan MA et al (2004) Time interval between abnormalities seen on CT and the clinical diagnosis of pancreatic cancer: retrospective review of CT scans obtained before diagnosis. AJR Am J Roentgenol 182:897–903
Higashi M, Tanabe M, Onoda H et al (2019) Incidentally detected pancreatic adenocarcinomas on computed tomography obtained during the follow-up for other diseases. Abdom Radiol (NY). https://doi.org/10.1007/s00261-019-02365-w
Ahn SS, Kim MJ, Choi JY, Hong HS, Chung YE, Lim JS (2009) Indicative findings of pancreatic cancer in prediagnostic CT. Eur Radiol 19:2448–2455
Tanaka S, Nakaizumi A, Ioka T et al (2002) Main pancreatic duct dilatation: a sign of high risk for pancreatic cancer. Jpn J Clin Oncol 32:407–411
Kang JD, Clarke SE, Abdolell M, Ramjeesignh R, Payne JI, Costa AF (2020) The implications of missed or misinterpreted cases of pancreatic ductal adenocarcinoma on imaging: a multi-centered population-based study. Eur Radiol. https://doi.org/10.1007/s00330-020-07120-0
Goldberg-Stein S, Frigini LA, Long S et al (2017) ACR RADPEER Committee White Paper with 2016 updates: revised scoring system, new classifications, self-review, and subspecialized reports. J Am Coll Radiol 14:1080–1086
Tempero MA, Malafa MP, Al-Hawary M et al (2017) Pancreatic Adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 15:1028-1061
Ahn SJ, Choi SJ, Kim HS (2017) Time to progression of pancreatic cancer: evaluation with multi-detector computed tomography. J Gastrointest Cancer 48:164–169
Kim JH, Park SH, Yu ES et al (2010) Visually isoattenuating pancreatic adenocarcinoma at dynamic-enhanced CT: frequency, clinical and pathologic characteristics, and diagnosis at imaging examinations. Radiology 257:87–96
Padilla-Thornton AE, Willmann JK, Jeffrey RB (2012) Adenocarcinoma of the uncinate process of the pancreas: MDCT patterns of local invasion and clinical features at presentation. Eur Radiol 22:1067–1074
Tamada T, Ito K, Kanomata N et al (2016) Pancreatic adenocarcinomas without secondary signs on multiphasic multidetector CT: association with clinical and histopathologic features. Eur Radiol 26:646–655
Smith SL, Rajan PS (2004) Imaging of pancreatic adenocarcinoma with emphasis on multidetector CT. Clin Radiol 59:26–38
Siewert B, Sosna J, McNamara A, Raptopoulos V, Kruskal JB (2008) Missed lesions at abdominal oncologic CT: lessons learned from quality assurance. Radiographics 28:623–638
Yoon SH, Lee JM, Cho JY et al (2011) Small (</= 20 mm) pancreatic adenocarcinomas: analysis of enhancement patterns and secondary signs with multiphasic multidetector CT. Radiology 259:442–452
Ren S, Chen X, Wang Z et al (2019) Differentiation of hypovascular pancreatic neuroendocrine tumors from pancreatic ductal adenocarcinoma using contrast-enhanced computed tomography. PLoS One 14:e0211566
Boninsegna E, Zamboni GA, Facchinelli D et al (2018) CT imaging of primary pancreatic lymphoma: experience from three referral centres for pancreatic diseases. Insights Imaging 9:17–24
Kanno A, Masamune A, Hanada K et al (2018) Multicenter study of early pancreatic cancer in Japan. Pancreatology 18:61–67
Ishikawa O, Ohigashi H, Imaoka S et al (1999) Minute carcinoma of the pancreas measuring 1 cm or less in diameter--collective review of Japanese case reports. Hepatogastroenterology 46:8–15
Tummala P, Tariq SH, Chibnall JT, Agarwal B (2013) Clinical predictors of pancreatic carcinoma causing acute pancreatitis. Pancreas 42:108–113
Pannala R, Leirness JB, Bamlet WR, Basu A, Petersen GM, Chari ST (2008) Prevalence and clinical profile of pancreatic cancer-associated diabetes mellitus. Gastroenterology 134:981–987
Lee JH, Kim SA, Park HY et al (2012) New-onset diabetes patients need pancreatic cancer screening? J Clin Gastroenterol 46:e58–e61
Gullo L, Pezzilli R, Morselli-Labate AM (1994) Diabetes and the risk of pancreatic cancer. N Engl J Med 331:81–84
Tenner S, Baillie J, DeWitt J, Vege SS (2013) American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 108:1400-15; 1416
Wolske KM, Ponnatapura J, Kolokythas O, Burke LMB, Tappouni R, Lalwani N (2019) Chronic pancreatitis or pancreatic tumor? A problem-solving approach. Radiographics 39:1965–1982
Kim SS, Choi GC, Jou SS (2018) Pancreas ductal adenocarcinoma and its mimics: review of cross-sectional imaging findings for differential diagnosis. J Belg Soc Radiol 102:71
Low G, Panu A, Millo N, Leen E (2011) Multimodality imaging of neoplastic and nonneoplastic solid lesions of the pancreas. Radiographics 31:993–1015
Deshmukh SD, Willmann JK, Jeffrey RB (2010) Pathways of extrapancreatic perineural invasion by pancreatic adenocarcinoma: evaluation with 3D volume-rendered MDCT imaging. AJR Am J Roentgenol 194:668–674
Toft J, Hadden WJ, Laurence JM et al (2017) Imaging modalities in the diagnosis of pancreatic adenocarcinoma: a systematic review and meta-analysis of sensitivity, specificity and diagnostic accuracy. Eur J Radiol 92:17–23
Fleischmann D, Kamaya A (2009) Optimal vascular and parenchymal contrast enhancement: the current state of the art. Radiol Clin North Am 47:13–26
Bashir MR, Gupta RT (2012) MDCT evaluation of the pancreas: nuts and bolts. Radiol Clin North Am 50:365–377
Almeida RR, Lo GC, Patino M, Bizzo B, Canellas R, Sahani DV (2018) Advances in pancreatic CT imaging. AJR Am J Roentgenol 211:52–66
Raman SP, Fishman EK (2014) Abnormalities of the distal common bile duct and ampulla: diagnostic approach and differential diagnosis using multiplanar reformations and 3D imaging. AJR Am J Roentgenol 203:17–28
Busby LP, Courtier JL, Glastonbury CM (2018) Bias in radiology: the how and why of misses and misinterpretations. Radiographics 38:236–247
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Andreu Costa.
Conflict of interest
Jessie Kang, Sharon Clarke, and Andreu Costa declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Statistical analysis was performed by the authors Jessie Kang and Andreu Costa.
Informed consent
The need for informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational
• Multi-institutional
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, J.D., Clarke, S.E. & Costa, A.F. Factors associated with missed and misinterpreted cases of pancreatic ductal adenocarcinoma. Eur Radiol 31, 2422–2432 (2021). https://doi.org/10.1007/s00330-020-07307-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07307-5