Abstract
Objectives
The clinical utility of electronically derived ASPECTS (e-ASPECTS) to quantify signs of acute ischemic infarction could be demonstrated in multiple studies. Here, we aim to clinically validate the impact of CT slice thickness (ST) on the performance of e-ASPECTS software.
Methods
A consecutive series of n = 258 patients (06/2016 and 01/2019) with middle cerebral artery occlusion and subsequent treatment with mechanical thrombectomy was analyzed. The e-ASPECTS score and acute infarct volumes were calculated from baseline non-contrast CT with a software using 1-mm slice thickness (ST) (defined as ground truth) and axial reconstructions with 2–10-mm ST and correlated with baseline stroke severity (NIHSS) as well as clinical outcome (mRS) using logistic regressions.
Results
In comparison with the ground truth, significant differences were seen in e-ASPECTS scores with ST > 6 mm (p ≤ 0.031) and infarct volumes with ST > 4 mm (p ≤ 0.001). There was a significant correlation of lower e-ASPECTS and higher acute infarct volumes with increasing baseline NIHSS values for all ST (p ≤ 0.001, respectively), with values derived from 1 mm yielding the highest correlation for both parameters (rho, − 0.38 and 0.31, respectively). Similarly, lower e-ASPECTS and higher acute infarct volumes from all ST were significantly associated with poor outcome after 90 days (p ≤ 0.05, respectively) with values derived from 1-mm ST yielding the highest effects for both parameters (OR, 0.69 [95% CI 0.50–0.88] and 1.27 [95% CI 1.10–1.50], respectively).
Conclusions
The e-ASPECTS software generates robust values for e-ASPECTS and acute infarct volumes when using ST ≤ 4 mm with ST = 1 mm yielding the best performance for predicting baseline stroke severity and clinical outcome after 90 days.
Key Points
• Clinical utility of automatically derived ASPECTS from computed tomography scans was shown in patients with acute ischemic stroke and treatment with mechanical thrombectomy.
• Thin slices (= 1 mm) had the highest clinical utility in comparison with thicker slices (2–10 mm) by having the strongest correlation with baseline stroke severity and independent effects on clinical outcome after 90 days.
• Automatically calculated acute infarct volumes possess clinical utility beyond ASPECTS and should be considered in future studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The imaging modality of choice for triage of patients with suspected acute ischemic stroke (AIS) is non-contrast-enhanced computerized tomography (NCCT), which enables to identify several signs for early ischemia. The Alberta Stroke Program Early CT Score (ASPECTS) was established to standardize the evaluation of infarct extent and assist in identifying patients eligible for reperfusion therapies by subdividing the territory of the middle cerebral artery into 10 different regions [1].
Software solutions aim to assist in the clinical decision-making in patients with AIS to evaluate infarct extent. The e-ASPECTS software from Brainomix (electronic Alberta Stroke Program Early CT Score = e-ASPECTS, www.brainomix.com) allows rapid and standardized automated analysis of NCCT slices and was shown to be non-inferior in the detection of parenchymal hypoattenuation in comparison with experienced neuroradiologists [2]. Furthermore, it can predict clinical outcome of AIS patients who are treated with mechanical thrombectomy (MT) [3]. The general clinical utility of e-ASPECTS in AIS patients has been validated in large real-world populations [3, 4], but the robustness of e-ASPECTS in regard to different ST of NCCT has not been investigated in detail yet. In its latest version, e-ASPECTS also quantifies the early ischemic changes by generating absolute volumes, but the clinical impact of this feature is not sufficiently known yet.
Here, we aim to clinically validate the impact of different ST of NCCT on the e-ASPECTS software’s performance and the differences in the clinical utility of the derived e-ASPECTS and infarct volumes.
Materials and methods
We selected consecutive patients with AIS due to large vessel occlusion of the middle cerebral artery, who underwent NCCT with ≤ 1-mm ST at a 64-multislice CT scanner (Somatom Definition AS, Siemens Healthineers GmbH) on admission and subsequent treatment with MT between June 2016 and January 2019 from a prospectively compiled database of our institution. Nine additional axial multiplanar reconstructions (MPR) between 2- and 10-mm ST (increment of 1 mm) were generated for each patient with Syngo.via (Siemens Healthineers GmbH) derived from 1-mm MPR.
Patients, whose scans could not be processed by the software due to technical reasons, were excluded. From all remaining patients, NCCT scans and their reconstructions were processed with e-ASPECTS (version 7.1). After resampling and standardizing the input including three-dimensional registration, e-ASPECTS uses machine learning classifiers to identify early ischemic changes in each voxel and segment those areas to compute electronic ASPECTS values as well as acute and non-acute ischemic changes by indicating those volumes in milliliters (mL). Parameters used in our analysis were e-ASPECTS (0–10) and acute infarct volume (indicated in mL, representing only acute ischemic changes).
Clinical presentation and outcome were measured by collecting the National Institutes of Health Stroke Scale (NIHSS) score on admission and discharge, as well as modified Rankin scale (mRS) at discharge and 90 days after onset by a neurologist. A NIHSS score of 42 was assigned to patients who deceased during their initial hospitalization. Occurrences of intracranial hemorrhage (ICH) were evaluated on follow-up NCCT 18 to 36 h after reperfusion therapy and categorized according to the Heidelberg Bleeding Classification [5].
Ethical considerations
The stroke database was approved by the local ethics committee. As this was a retrospective analysis, additional written informed consent was waived.
Statistical analysis
The e-ASPECTS and acute infarct volumes derived from the different MPR reconstructions (2–10 mm in 1-mm increments) were compared against those of the respective 1-mm dataset (which was defined as ground truth since Brainomix generally recommends using 1-mm ST to generate e-ASPECTS) using the Wilcoxon rank-sum test. Correlations of e-ASPECTS and acute infarct volumes derived from 2- to 10-mm ST were compared with the correlations of those parameters derived from 1-mm ST by calculating Spearman’s correlation coefficient. Associations of e-ASPECTS and acute infarct volumes with clinical outcome after 90 days and hemorrhagic events in follow-up NCCT were analyzed for all ST using multivariate generalized logistic regressions adjusted for baseline and periprocedural variables. The absolute agreement between all reconstructions and the ground truth was determined. All statistical analyses were performed using R version 3.4.1 (Foundation for Statistical Computing).
Results
Patients and clinical outcome
Of a total of 1242 patients, 258 patients (51.2% female, 75 ± 11.8 years) with AIS due to occlusion of the middle cerebral artery were included in the analysis (see Fig. 1 for a flowchart of patient selection). These patients presented with a median NIHSS of 15 (interquartile range [IQR], 10–20) on admission. The median onset-to-groin-puncture time was 222 min (IQR, 140–410 min). Successful reperfusion could be achieved in 219 patients (84.9%, defined as modified thrombolysis in cerebral infarction (mTICI) ≥ 2b), while unsuccessful recanalization was noted in 13 patients (5.8%, defined as mTICI ≤ 1). Overall, 134 patients (51.9%) were concomitantly treated with bridging intravenous thrombolysis. After reperfusion therapy, any ICH was detected in 50 (19.4%) patients, while 11 patients (4.3%) developed symptomatic ICH on follow-up NCCT. Median e-ASPECTS on initial imaging (calculated from 1-mm ST) was 9 (IQR, 8–10) and the median infarct volume was 29.58 mL (IQR, 16.29–46.35 mL). The median outcome of patients after 90 days measured by mRS was 2 (IQR, 0–5) with 53.1% having a moderate outcome (mRS after 90 days of 0–2) and a mortality rate of 18.9%. Clinical attributes of all patients, as well as baseline and imaging characteristics, are shown in Table 1.
Univariate evaluation of e-ASPECTS and infarct volumes
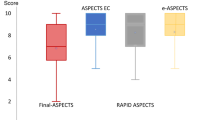
No significant difference of e-ASPECTS scores was derived in univariate tests between 1-mm ST and those from MPR with 2–6 mm. However, there was a difference in e-ASPECTS derived from MPR with ST > 6 mm (p ≤ 0.031, respectively). For the calculated acute infarct volumes, there were significant differences between values derived from the ground truth and those derived from MPR with ST > 4 mm (p < 0.001, respectively), while acute infarct volumes derived from MPR with 2–4-mm ST did not differ significantly (p > 0.101, respectively). Summary statistics and the univariate differences of e-ASPECTS scores and acute infarct volumes derived from the 1-mm ground truth with those of the different MPR are summarized in Table 2. Results on the absolute agreement of e-ASPECTS scores and acute infarct volumes derived from 1-mm ground truth with those of the different MPR are depicted in Figs. 2 and 3, respectively. Figure 4 illustrates the differences between ST of 1 mm, 5 mm, and 10 mm and their respective e-ASPECTS analyses on NCCT images of an exemplary patient.
Violin plots of absolute differences of e-ASPECTS between the ground truth (1-mm ST) and multiplanar reconstructions with ST from 2 to 10 mm. Asterisks depict the respective mean of each ST and the dashed line represents the baseline of 0. With increasing ST, a trend to overestimate e-ASPECTS in comparison to the ground truth can be noted
Box plots of absolute differences in acute infarct volumes (mL) between the ground truth (1-mm ST) and multiplanar reconstructions with ST from 2 to 10 mm. Asterisks depict the respective mean of each ST and the dashed line represents the baseline of 0. With increasing ST, there is a trend to underestimate the acute infarct volume in comparison to the ground truth with increasing ST
Exemplary illustration of a CT scan with occlusion of the right middle cerebral artery (a) and the respective analyses of e-ASPECTS with overlay of 1-mm ST (b), 5-mm ST (c), and 10-mm ST. The subregions which are defined to grade the ASPECTS are outlined in yellow color. Regions which show signs of early ischemia are framed with red color. More intense red color reflects more distinct features of ischemia. The yellow dotted line represents the cerebral midline. While the signs of early ischemia in the anterior middle cerebral artery cortex, corresponding to the frontal operculum, are analyzed by e-ASPECTS on b to be distinct enough to interpret it as affected on 1-mm ST by e-ASPECTS, it is not considered as such on c and d. Furthermore, the putamen is interpreted as affected by signs of early ischemia on b and c, but not on d. On all analyses, signs of early ischemia of the insular cortex are considered to be affected. This results in differences of the global evaluation of e-ASPECTS, which might change the clinical approach in a corresponding setting (e-ASPECTS for b = 7, e-ASPECTS for c = 8, e-ASPECTS for d = 9)
Correlation of e-ASPECTS and infarct volumes with baseline stroke severity
There was a significant correlation between e-ASPECTS as well as calculated acute infarct volumes and baseline stroke severity measured by NIHSS for all evaluated ST (p ≤ 0.001). However, a progressive increase in correlation coefficients was noted for lower ST with the highest correlation coefficients yielded when using the 1-mm ground truth (rho of − 0.38 for e-ASPECTS and 0.31 for acute infarct volume) (Fig. 5).
Regression analysis to predict clinical outcome
In multivariate generalized logistic regressions adjusted for baseline and periprocedural variables (see legend of Table 3 for details), e-ASPECTS scores from all ST were significantly associated with the clinical outcome after 90 days (p ≤ 0.05, respectively). Specifically, the e-ASPECTS scores that were derived from 1-mm ST yielded the highest effects with odds ratios (OR) of 0.69 (95% CI, 0.50–0.88, p = 0.003) for poor clinical outcome (mRS 3–6 on 90 days after onset). Similarly, acute infarct volumes from all ST were significantly associated with the clinical outcome after 90 days (p ≤ 0.03, respectively). Again, the acute infarct volumes that were derived from 1-mm ST yielded the highest effects with odds ratios of 1.27 (95% CI, 1.10–1.50, p = 0.002). Furthermore, acute infarct volumes were independently associated with mortality after 90 days (mRS 6 on 90 days after onset) with 1-mm ST yielding the highest effects (OR of 1.26, 95% CI 1.07–1.50, p = 0.006), while e-ASPECTS did not show independently significant effects on mortality after 90 days. No significant and independent effects of e-ASPECTS or acute infarct volumes on the occurrence of any or symptomatic ICH in the follow-up CT could be found. Results of multivariate generalized logistic regressions for poor outcome and mortality after 90 days as well as occurrence of symptomatic ICH for the predictors of e-ASPECTS and acute infarct volume are summarized in Table 3.
Discussion
The implementation of electronically derived ASPECTS by automated software solutions has been shown to be a clinically useful tool [2, 4]. Our results confirm that the e-ASPECTS software produces robust scores generated from NCCT up to 6-mm ST and acute infarct volumes derived from NCCT up to 4-mm ST. However, e-ASPECTS and infarct volumes derived from 1-mm ST had the best clinical utility, as they showed the highest correlation with the baseline stroke severity and had the strongest independent effects on the clinical outcome after 90 days. While e-ASPECTS had stronger correlations with baseline stroke severity, prediction of mortality after 90 days could not be determined with e-ASPECTS scores, but only with acute infarct volumes. No independent association between e-ASPECTS or infarct volumes and occurrences of any or symptomatic ICH after reperfusion therapy could be found.
The non-inferiority of e-ASPECTS software in comparison with neuroradiologists was demonstrated by Nagel et al in a cohort of 132 patients with AIS [2]. Herweh et al could also show in 32 AIS patients that e-ASPECTS generated results similar to stroke experts [6]. Recently, Nagel et al applied e-ASPECTS analysis on a large multicenter trial and could reliably predict the clinical outcome of 1480 patients with AIS and treatment with intravenous thrombolysis [4]. In their study, they performed a sensitivity analysis and found that NCCT scans with thin slices (≤ 3 mm) performed even better in predicting clinical outcome than in the general cohort with ST ≤ 6 mm, proposing that an optimal ST of 1 mm would lead to more concise results. Also, Brainomix recommends using thin slice CT images to generate e-ASPECTS, ideally ST of 1 mm. Our results did not show significant differences between the suggested optimal ST of 1 mm and larger ST up to 6 mm for e-ASPECTS and 4 mm for acute infarct volumes. Still, we can support the notion that it is reasonable to use the optimal ST of 1 mm for the computation of e-ASPECTS or infarct volumes, as these had the strongest clinical impact by featuring the highest correlation with baseline stroke severity and highest effects on the clinical outcome after 90 days in this cohort of patients with AIS who were treated with MT. Higher ST tended to overestimate e-ASPECTS and correspondingly underestimate the acute infarct volume in our analysis, which might influence the appropriate triage of patients with AIS. Although it is understood that thicker slices tend to allow better visual identification of ischemic demarcation by the human reader, the algorithm of e-ASPECTS seems to handle thinner slices better, as asserted by Brainomix.
It is worth highlighting that we were not able to independently predict mortality after 90 days with e-ASPECTS, but only with acute infarct volumes, which the e-ASPECTS software quantifies in absolute milliliter units. To the best of our knowledge, infarct volumes generated by e-ASPECTS software were not included in published studies as a predictor for clinical outcome so far. Our findings suggest that this parameter possesses clinical utility on its own and should be further investigated in future studies. Comparing and validating not only e-ASPECTS [7] but also infarct volumes generated with e-ASPECTS software with the (final) infarct core derived from perfusion maps would be of particular interest in this context.
Multivariate regressions adjusted for important clinical and periprocedural parameters did not find significant and independent effects on the occurrence of any or symptomatic ICH after MT. This finding is surprising, as bigger infarct sizes were shown to be associated with a higher risk of any or symptomatic ICH after MT [8], possibly due to more extensive damage to the blood-brain barrier. Our results support the assumption that parameters such as age, onset-to-groin times, and successful reperfusion, which were used for adjustment of the models, are more important predictors than e-ASPECTS alone for the occurrence of ICH in patients with AIS of the middle cerebral artery and treatment with MT. One possible approach to increase the prediction of symptomatic ICH with e-ASPECTS might be to take the intensity of hypoattenuation into account. Currently, the progression of infarct demarcation can only be derived by visual qualitative assessment of the red heat map provided as an overlay by e-ASPECTS.
Certainly, e-ASPECTS represents a valuable tool for triage and outcome prediction, especially for non-experienced radiologists and clinicians. However, some caveats of e-ASPECTS must be taken into consideration. Pre-existing parenchymal changes, like leukoencephalopathy or previous strokes, pose a challenge for e-ASPECTS [9]. Nagel et al had to exclude a small number of scans (3.5%) from their multicenter study because of general technical issues (read errors, segmentation errors) [4]. We encountered similar problems, as we also had to exclude a small number of scans (1.9%) due to technical problems. Also, not all software solutions which provide automatically calculated ASPECTS deliver the same reliability [10].
Some general limitations of our study have to be acknowledged. Although data of stroke patients were registered prospectively, this study was performed retrospectively and data were gathered from a single center. Thus, raw data of CT scans were not available anymore, and MPR were derived from 1-mm images. Possible differences between e-ASPECTS derived from MPR of already reconstructed images and MPR from raw CT data were not taken into account and should be investigated further in prospective studies. As the purpose of this study was to determine the internal robustness of the e-ASPECTS software and as its non-inferiority to neuroradiologists was already shown, the generated e-ASPECTS of this study were not tested against the ASPECTS of human readers. Adverse events between discharge and 90-day follow-up, which might have possibly affected the mRS score, were not gathered and could thus not be included in our analysis.
In conclusion, we could demonstrate that e-ASPECTS scores and acute infarct volumes generated with the e-ASPECTS software had the highest clinical utility derived from NCCT with 1-mm ST by the highest correlation with the baseline stroke severity and having the strongest independent effects on clinical outcome after 90 days. No significant difference of e-ASPECTS scores was derived in univariate tests between 1-mm ST and those from MPR with 2–6 mm, but for e-ASPECTS derived from MPR with ST > 6 mm. Notably, prediction of mortality after 90 days was only possible using acute infarct volumes, but not e-ASPECTS scores.
Abbreviations
- AIS:
-
Acute ischemic stroke
- ASPECTS:
-
Alberta Stroke Program Early CT Score
- CI:
-
Confidence interval
- e-ASPECTS:
-
Electronically derived Alberta Stroke Program Early CT Scores
- ICH:
-
Intracranial hemorrhage
- IQR:
-
Interquartile range
- MPR:
-
Multiplanar reconstructions
- mRS:
-
Modified Rankin scale
- MT:
-
Mechanical thrombectomy
- mTICI:
-
Modified thrombolysis in cerebral infarction
- NCCT:
-
Non-contrast-enhanced computerized tomography
- NIHSS:
-
National Institutes of Health Stroke Scale
- OR:
-
Odds ratio
- ST:
-
Slice thickness
References
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Lancet 355:1670–1674. https://doi.org/10.1016/S0140-6736(00)02237-6
Nagel S, Sinha D, Day D et al (2017) e-ASPECTS software is non-inferior to neuroradiologists in applying the ASPECT score to computed tomography scans of acute ischemic stroke patients. Int J Stroke 12:615–622. https://doi.org/10.1177/1747493016681020
Pfaff J, Herweh C, Schieber S et al (2017) e-ASPECTS correlates with and is predictive of outcome after mechanical thrombectomy. AJNR Am J Neuroradiol 38:1594–1599. https://doi.org/10.3174/ajnr.A5236
Nagel S, Wang X, Carcel C et al (2018) Clinical utility of electronic Alberta stroke program early computed tomography score software in the ENCHANTED trial database. Stroke 49:1407–1411. https://doi.org/10.1161/STROKEAHA.117.019863
Neuberger U, Möhlenbruch MA, Herweh C, Ulfert C, Bendszus M, Pfaff J (2017) Classification of bleeding events: comparison of ECASS III (European Cooperative Acute Stroke Study) and the New Heidelberg Bleeding Classification. Stroke 48. https://doi.org/10.1161/STROKEAHA.117.016735
Herweh C, Ringleb PA, Rauch G et al (2016) Performance of e-ASPECTS software in comparison to that of stroke physicians on assessing CT scans of acute ischemic stroke patients. Int J Stroke 11:438–445. https://doi.org/10.1177/1747493016632244
Olive-Gadea M, Martins N, Boned S et al (2019) Baseline ASPECTS and e-ASPECTS correlation with infarct volume and functional outcome in patients undergoing mechanical thrombectomy. J Neuroimaging 29:198–202. https://doi.org/10.1111/jon.12564
Neuberger U, Kickingereder P, Schönenberger S et al (2019) Risk factors of intracranial hemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. Neuroradiology 61:461–469. https://doi.org/10.1007/s00234-019-02180-6
Guberina N, Dietrich U, Radbruch A et al (2018) Detection of early infarction signs with machine learning-based diagnosis by means of the Alberta Stroke Program Early CT score (ASPECTS) in the clinical routine. Neuroradiology 60:889–901. https://doi.org/10.1007/s00234-018-2066-5
Goebel J, Stenzel E, Guberina N et al (2018) Automated ASPECT rating: comparison between the Frontier ASPECT Score software and the Brainomix software. Neuroradiology 60:1267–1272. https://doi.org/10.1007/s00234-018-2098-x
Funding
Dr. Kickingereder, MBA, was supported by the Else Kröner-Fresenius Foundation (Else Kröner Memorial Scholarship).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantors of this publication are Dr. Philipp Kickingereder, MBA and Dr. Ulf Neuberger.
Conflict of interest
Dr. Nagel received grants, personal fees, and other from Brainomix; personal fees and other from Bayer, personal fees and other from Bohringer Ingelheim; personal fees and other from Medtronic; and personal fees from Pfizer outside of submitted work. Dr. Pfaff has received payment for lectures from the University of Hamburg-Eppendorf and Asklepios Arzteakademie; travel and meeting expenses from Stryker and MicroVention Deutschland. Dr. Bendszus has received grants and personal fees from Novartis, Guerbet, and Codman; personal fees from Vascular Dynamics, Roche, Teva, Springer, and Bayer Vital; grants from Siemens and Hopp Foundation. DFG. Dr. Mohlenbruch has received personal fees from Codman, MicroVention, Phenox, and Stryker. Dr. Herweh received personal fees form Brainomix.
The other authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained at the local ethics committee of the medical faculty of the University of Heidelberg.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neuberger, U., Nagel, S., Pfaff, J. et al. Impact of slice thickness on clinical utility of automated Alberta Stroke Program Early Computed Tomography Scores. Eur Radiol 30, 3137–3145 (2020). https://doi.org/10.1007/s00330-019-06616-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06616-8