Abstract
Objectives
We reviewed PET/CT findings of pneumoconiosis and determined the ability of PET/CT to differentiate lung cancer from progressive massive fibrosis (PMF), and metastatic lymph nodes (LNs) from underlying reactive LN hyperplasia.
Methods
This was a retrospective study of patients with pneumoconiosis and suspected lung cancer. Maximum standardized uptake value (SUVmax), long- and short-axis diameters (DL and DS), ratio of DL to DS (DL/S), and Hounsfield unit (HU) from the lung mass and mediastinal LNs were measured. The cutoff values of each parameter were obtained by ROC analysis, and we evaluated the diagnostic sensitivity.
Results
Forty-nine pneumoconiosis patients were included. Eighty-three lung masses were detected, of which 42 were confirmed as lung cancer (23 squamous cell carcinomas, 12 adenocarcinomas, and 7 small cell carcinomas) and 41 were PMF. There were significant differences between lung cancer and PMF in terms of SUVmax, DS, DL/S, and HU (all p < 0.05). The sensitivity, specificity, and accuracy for diagnosis of lung cancer were 81.0%, 73.2%, and 77.1%, respectively, with an SUVmax cutoff value of 7.4; and 92.8%, 87.8%, and 90.4%, respectively, with a HU cutoff value of 45.5. Among the 40 LNs with available pathological results, 7 were metastatic. Metastatic LNs showed higher SUVmax, larger DS, and lower HU than benign lesions (all p < 0.05). The sensitivity, specificity, and accuracy for predicting metastatic LNs by PET/CT were 85.7%, 93.9%, and 92.5%, respectively.
Conclusion
By applying PET and CT parameters in combination, the accuracy for differentiating malignant from benign lesions could be increased. PET/CT can play a central role in the discrimination of lung cancer and PMF.
Key Points
• Lung cancer showed significantly higher SUVmax than PMF.
• Lung cancer showed similar D L but longer D S , resulting in a smaller D L/S than PMF.
• SUVmax demonstrated additive value in differentiating lung cancer from PMF, compared with HU alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The prevalence of pneumoconiosis in a given country varies according to socioeconomic factors related to its coal-mining industry. In most developed countries, the incidence rates of coal work–related and occupational respiratory diseases are no longer increasing and have leveled off because of a decrease in the number of active workers commensurate with the decline of the mining industry [1]. However, patients with a history of working in mining areas are still being diagnosed with pneumoconiosis, because it takes more than 20 years to develop pneumoconiosis after exposure to coal or mineral dust [2].
Pneumoconiosis could lead to several thoracic complications, among which progressive massive fibrosis (PMF) and lung malignancy are the most serious [3, 4]. Although differentiation between PMF and lung malignancy is clinically essential, it is usually difficult to determine malignancy with non-invasive imaging modalities in pneumoconiosis patients. On chest computed tomography (CT), PMF is characterized by large symmetrical opacities in the bilateral lungs, which can contain air bronchograms and calcifications [5, 6]. The CT findings of occupational and environmental lung cancers can appear similar to those of PMF, which presents as unilateral or bilateral opacities ranging from nodules of a few millimeters to large masses [4]. These are well-known limitations inherent to radiological imaging studies, which reduce their diagnostic accuracy in assessing pulmonary nodules or masses in pneumoconiosis patients. In addition, it is difficult to determine whether metastatic involvement is present in the mediastinal lymph nodes (LNs) using only chest CT in pneumoconiosis patients with lung cancer.
As a functional imaging modality, positron emission tomography (PET) with 18F-fluorodeoxyglucose (FDG) can visualize tumor metabolism and allow semi-quantitative measurement of this activity. It has also been reported to have high sensitivity for differentiation between lung cancer and benign pulmonary nodules or mass lesions [7]. Moreover, the combination of PET and CT (PET/CT) has been shown to provide better morphological details of the lesions and overcome the limitations related to attenuation in PET [8, 9]. FDG PET/CT has proven helpful for differentiation between lung cancer and benign pulmonary nodules or mass lesions [10]. However, in cases with non-malignant conditions (like infection, sarcoidosis, tuberculosis, and PMF), inflammation related to the disease may cause false-positive findings, which is a limitation of PET/CT. Radiotracers other than FDG including 3′-deoxy-3′-18F-fluorothymidine (FLT) as a biomarker of tumor proliferation, 18F-fluoromisonidazole (FMISO) as a biomarker of tumor hypoxia, and L-[3-18F]-α-methyl tyrosine (18F-FMT) as a biomarker of amino-acid metabolism have also shown promise [11,12,13]. There have been few reports of the use of PET/CT to assess lung masses in case series of pneumoconiosis patients [14, 15]. To our knowledge, few data are available on the diagnostic value of FDG PET/CT for distinguishing lung cancer from PMF. One report did not recommend PET/CT in the staging of mediastinal LNs in lung cancer patients with pneumoconiosis because of the low specificity for the diagnosis of metastatic lymphadenopathy [16]. However, in non-pneumoconiosis patients, a sensitivity of 88.3% and specificity of 82.6% were observed for FDG PET/CT in mediastinal LN staging by using both SUVmax and Hounsfield unit (HU) information [17]. Therefore, we hypothesized that FDG PET/CT could be helpful in mediastinal LN staging in patients with underlying pneumoconiosis. The present study was performed to investigate the diagnostic value of PET/CT with respect to differentiating PMF from lung cancer, and for assessing mediastinal LN in lung cancer patients with pneumoconiosis.
Materials and methods
Patient population
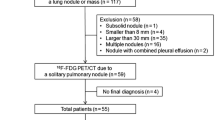
This retrospective study was approved by our Institutional Review Board. The requirement for informed consent was waived because of the retrospective design of the study. A total of 74 pneumoconiosis patients with suspected lung cancer on previous chest radiography or chest CT and who underwent PET/CT between July 2009 and April 2016 were retrospectively screened. We excluded patients with a previous history of comorbid malignancy (n = 5) and lack of sufficient clinical data (n = 20). Forty-nine pneumoconiosis patients were finally enrolled (Fig. 1) (48 men and one woman; mean age, 72.6 years; range 54–87 years). In total, 48 patients had an occupational history associated with pneumoconiosis (41 coal workers, 7 stonemasons), and occupational history was unknown for one patient. Mean occupational duration of the 48 patients was 21.7 ± 7.9 years.
FDG PET/CT protocol
All patients fasted for at least 6 h before the PET/CT scan. A dose of 3.7–5.5 MBq/kg [18F]FDG was injected intravenously, and scanning began 60 min later. None of the patients had a blood glucose level > 150 mg/dL before injection. No intravenous contrast agent was administered. Images were acquired using a combined PET/CT in-line system (Biograph Duo or Biograph TruePoint; Siemens Medical Solutions). The acquisition time was 2–3 min per bed position. Six or seven beds were acquired according to patient’s height. All patients were in the supine position without breath-holding during the PET/CT scan. CT began at the orbitomeatal line and progressed to the proximal thigh using a standard protocol: 130 kVp, 80 mAs, 5-mm slice thickness (Biograph Duo); and 120 kVp, 50 mAs, 5-mm slice thickness (Biograph TruePoint). Average CT dose index (CTDIvol) was 4.96 mGy. CT data was used for attenuation correction, and CT images were reconstructed with body 30 kernel, back projection algorithm, and a 512 × 512 voxel matrix. PET scans of the same body region were performed immediately afterwards, and images were reconstructed using a standard ordered-subset expectation maximization algorithm with 4 iterations and 8 subsets.
Image analysis
PET/CT images were assessed using software (XD3; Mirada Medical), which produced multiplanar reformatted images and displayed attenuation-corrected PET images, CT images, and PET/CT fusion images. Image analysis was performed by two experienced nuclear medicine physicians (with 9 and 10 years of experience, respectively). In case of reader disagreement, we reached consensus with another nuclear medicine physician (22 years of experience). For semi-quantitative analysis, the maximum standardized uptake value (SUVmax) was measured from PET images by placing a spherical region of interest (ROI) at the site of suspected primary lung cancer or PMF. Long- and short-axis diameters (DL and DS), ratio of long- to short-axis diameter (DL/S), and Hounsfield unit (HU) were measured on the CT portion of PET/CT.
In addition to quantitative analysis, two nuclear medicine physicians independently conducted visual analysis for lung masses. For discordant lesions, final decision was made by a third nuclear medicine physician. For the PET portion, when the masses showed intense FDG uptake and globular shape, they were considered lung cancer. Masses with elongated shape regardless of FDG uptake were considered PMF. For the CT portion, when the masses showed globular shape and lower attenuation compared with blood vessels or muscle density on non-contrast CT, they were considered lung cancer. On the other hand, masses with elongated shape, high density above blood vessels or muscle, and/or calcification were considered PMF. For PET/CT, when the masses showed intense FDG uptake, globular shape, and lower attenuation compared with blood vessels or muscle density on non-contrast CT portion, they were considered lung cancer. On the other hand, masses with elongated shape, high density above blood vessels or muscle, and/or calcification were considered PMF. For intrareader reliability analysis, one reader reviewed the images 14 weeks after the first image review.
SUVmax, DS, and HU from the mediastinal LNs, which were confirmed reactive or metastatic LN by endobronchial ultrasound–guided transbronchial needle aspiration (EBUS-TBNA) or operation, were measured. DS and HU were measured on the CT portion of PET/CT. The mediastinal LN locations were described according to the International Association for the Study of Lung cancer (IASLC) LN map [18]. Metastatic LNs on PET images were defined as those showing FDG uptake higher than mediastinal blood pool activity (aortic arch level) with an asymmetric distribution. Asymmetric distribution means that enlarged LNs with increased FDG uptake were made prominent on one side (right or left). Metastatic LNs on CT images were defined as LN enlargement with DS ≥ 1 cm and attenuation < 70 HU. For PET/CT criteria, the LN showed a higher uptake than the mediastinal blood pool, with an asymmetric distribution and attenuation < 70 HU [19].
To evaluate the diagnostic value of N staging using PET/CT, we compared overall N staging using both PET/CT criteria and CT (only) criteria.
Reference of diagnosis
All suspected lung cancer masses on PET/CT were pathologically confirmed by CT-guided biopsy or operation. Among the pneumoconiotic nodules, lesions > 1 cm in diameter were considered PMF. For suspected PMF masses, the final diagnosis was made by one of two methods. Histopathological confirmation was performed in patients with available findings from CT-guided biopsy or operation. In patients for whom histopathological confirmation was unavailable, the final diagnosis was made by imaging and clinical follow-up. Lesions that were not pathologically confirmed but remained unchanged or showed an indolent clinical course for at least 2 years of follow-up (mean 33.2 months) were considered PMF.
Statistical analysis
Statistical analyses were carried out using SPSS software (ver. 24.0; SPSS). All values are presented as means ± standard deviation (range). After a normality test (the Kolmogorov–Smirnov test), either Student’s t test or the Mann–Whitney U test was performed to compare the mean values of SUVmax, DL, DS, DL/S, and HU from lung cancer and PMF, and the mean values of SUVmax, DS, and HU from metastatic LNs and reactive LNs. The sensitivity, specificity, and accuracy of PET/CT and CT for diagnosis of metastatic mediastinal LN were compared by McNemar’s test. Receiver operating characteristic (ROC) analysis was used to determine the optimal cutoff value to differentiate lung cancer from PMF and to differentiate metastatic LN from reactive LN. Inter-reader agreement was expressed as kappa value. For intrareader reliability, we used intraclass correlation coefficient (ICC) by a two-way random effects model. In all analyses, p < 0.05 was taken to indicate statistical significance.
Results
Of 83 lung masses detected in 49 patients, 42 were lung cancer and 41 were PMF. The median value and average of number of lung masses per patient were 1 and 1.7, respectively (range 1~4). Among the 42 lung cancers, squamous cell carcinoma was the most common type (n = 23), followed by adenocarcinoma (n = 12) and small cell carcinoma (n = 7). The treatment methods of 42 lung cancer patients were as follows: operation (n = 8), systemic chemotherapy with/or without radiation therapy (n = 19), radiation therapy (n = 6), or conservative care (n = 9).
Lung cancer versus PMF
Forty-two lung cancers were confirmed by biopsy or surgical pathology. Forty-one PMF lesions were confirmed by CT-guided biopsy (n = 1) or imaging and clinical follow-up (n = 40). SUVmax of lung cancer was significantly higher than that of PMF (12.3 ± 5.7 vs. 6.3 ± 2.8, respectively; p < 0.001) (Fig. 2). There was no difference in DL between lung cancer and PMF (4.0 ± 1.6 vs. 4.7 ± 2.1; p = 0.082), but lung cancer showed longer DS (2.8 ± 1.2 cm vs. 2.3 ± 1.0 cm, respectively; p = 0.020) and smaller DL/S (1.4 ± 0.3 vs. 2.2 ± 0.6, respectively; p < 0.001) compared with PMF. HU of lung cancer was significantly lower than that of PMF (36.6 ± 9.3 vs. 61.3 ± 19.6, respectively; p < 0.001) (Table 1 and Fig. 3).
A 77-year-old man with a growing mass in the left upper lobe (LUL). a Maximum intensity projection image, (b) axial PET image, and (c) axial CT image showing a lobulated mass with intense focal uptake in the LUL (arrowhead, SUVmax 23.3, DL 3.2 cm, DS 2.3 cm, DL/S 1.4, and HU 39.6) and irregular coalescent nodule with moderate FDG uptake in the right upper lobe (RUL) (arrow, SUVmax 7.0, DL 4.1 cm, DS 1.7 cm, DL/S 2.4, and HU 60.4). Squamous cell carcinoma was confirmed by LUL lobectomy. The RUL mass showed no growth for 2 years, suggestive of PMF. Mediastinal LNs showed symmetrically increased FDG uptake with higher density. For the right lower paratracheal and subcarinal LNs, reactive LNs were confirmed by pathology
A subgroup analysis was performed according to PET/CT scanner (scanners 1 and 2) considering the dependence of HU value on the kilovoltage peak in CT protocol. In the subgroup analysis of PET/CT scanner 1, HU of lung cancer was significantly lower than that of PMF (37.5 ± 8.2 vs. 59.7 ± 13.8, respectively; p = 0.001). Likewise, in the subgroup analysis of PET/CT scanner 2, HU of lung cancer was significantly lower than that of PMF (36.2 ± 9.7 vs. 62.2 ± 22.4, respectively; p < 0.001).
In ROC analysis, FDG PET/CT had a sensitivity of 81.0%, specificity of 73.2%, and accuracy of 77.1%, with SUVmax 7.4 as the cutoff value (AUC 0.848, p < 0.001). The sensitivity, specificity, and accuracy were 92.8%, 87.8%, and 90.4%, respectively, for a cutoff HU value of 45.5 (AUC 0.910, p < 0.001). Using a cutoff value of 1.7 for DL/S, the sensitivity, specificity, and accuracy were 85.7%, 80.5%, and 83.1%, respectively (AUC 0.874, p < 0.001). The sensitivity, specificity, and accuracy were 57.1%, 66.7%, and 61.9%, respectively, for DS cutoff value of 2.45 cm (AUC 0.648, p = 0.02) (Fig. 4). When we combined the cutoff value of SUVmax (> 7.4) and HU (< 45.5), the sensitivity, specificity, and accuracy were 73.8%, 97.6%, and 85.5%, respectively. The specificity was higher than that using SUVmax or HU alone.
In subjective analysis, reader disagreement was seen in thirteen lung masses for PET, three for CT, and six for PET/CT. The degree of inter-observer agreement expressed as kappa value for PET, CT, and PET/CT was 0.69, 0.86, and 0.93, respectively. The sensitivity, specificity, and accuracy for PET were 88.1%, 90.2%, and 89.2%, respectively. The sensitivity, specificity, and accuracy for CT were 97.6%, 97.6%, and 97.6%, respectively. The sensitivity, specificity, and accuracy for PET/CT were 100%, 97.6%, and 97.6%, respectively.
For intrareader reliability, ICC of PET, CT, and PET/CT was 0.879 (95% confidence interval [CI] 0.813, 0.922; p < 0.001), 0.963 (95% CI 0.942, 0.976; p < 0.001), and 0.940 (95% CI 0.907, 0.961; p < 0.001), respectively.
Mediastinal lymph node staging
A total of 40 LNs from 18 patients had histological results available (20 from EBUS-TBNA and 20 LNs from surgery). Seven LNs were confirmed to be metastatic (details of all 40 LNs are described in supplementary data 1). Metastatic LNs showed significantly higher SUVmax (7.4 ± 2.5 vs. 5.6 ± 1.8, respectively; p = 0.027), larger DS (1.5 ± 0.7 cm vs. 0.9 ± 0.4 cm, respectively; p = 0.008), and lower HU (40.5 ± 7.5 vs. 57.8 ± 14.1, respectively; p = 0.001) than reactive LNs. When applying the diagnostic criteria of PET, the sensitivity, specificity, and accuracy of mediastinal LN staging were 85.7%, 87.9% and 87.5%, respectively. The sensitivity, specificity, and accuracy with CT were 71.4%, 69.7% and 70.0%, respectively. Using PET/CT criteria, the sensitivity, specificity, and accuracy were 85.7%, 93.9%, and 92.5%, respectively. The specificity and accuracy of PET/CT were significantly higher than those of CT alone (p = 0.039 and p = 0.035, respectively). There were no significant differences between PET only and CT only results, or between PET only and PET/CT combined (all p > 0.05, Table 2).
We analyzed overall N staging in 40 lung cancer patients with final diagnosis available, either by pathology or by clinical follow-up. PET/CT accurately predicted N staging in 38 of 40 patients and CT predicted N staging in 33 of 40 patients. For one patient, N stage could not be predicted by PET/CT or CT. There were seven discordant cases between PET/CT and CT. Of the seven discordant cases, PET/CT was wrong in one case and CT was wrong in six cases. One case which was N0 by PET/CT due to symmetric FDG uptake in mediastinal LNs had a subcarinal node with 1.3 cm and 45.2 HU on CT portion. CT N stage was N2. EBUS-TBNA was done and pathology of subcarinal node was metastatic carcinoma. The other six cases were accurately predicted by PET/CT: three cases were upstaged and three cases were downstaged. One of the patients downstaged by PET/CT resulted in change of treatment and could undergo surgical resection.
Discussion
Our study highlights the diagnostic value of PET/CT for differential diagnosis between lung cancer and PMF in pneumoconiosis patients. This study compares the PET/CT findings of PMF and lung cancer based on both PET (SUVmax) and CT parameters (size, shape, and density). Compared with PMF, lung cancer showed a higher SUVmax, longer DS, smaller DL/S, and lower HU. Our study suggests that PET/CT may have a role in the differentiation between lung cancer and PMF in pneumoconiosis patients.
Kakubo et al reported that SUVmax was significantly higher in lung cancer than in pneumoconiotic lesions [20]. This finding is similar to our results, indicating the potential of SUVmax for differentiation between lung cancer and benign lesions in pneumoconiosis patients. However, the previous report showed a lower mean SUVmax in cases of pneumoconiotic lesions than was seen in PMF lesions in the present study (2.85 ± 0.24 vs. 6.3 ± 2.8, respectively). Likewise, SUVmax of lung cancer in the previous study was lower than that in the present study (7.12 ± 2.36 vs. 12.3 ± 5.7). The difference in SUVmax between PMF lesions in our study and pneumoconiotic lesions in the previous study was likely due to differences in the size of the lesions included in the analyses; while the previous study included pneumoconiotic lesions ≤ 3 cm, we included only PMFs > 1 cm in diameter. Thus, the higher SUVmax of PMF in our study may be explained by the larger size of PMF lesions included in the analysis. A wide range of SUVmax values has been reported for PMF in the literature, with a mean value of 6.3 (range 1.9–14.3) [14, 20, 21].
We plotted ROC curves to determine the optimal cutoff values of PET and CT parameters for differential diagnosis between lung cancer and PMF. While the sensitivity of HU (92.9%) was sufficient to detect lung cancer in pneumoconiosis patients, the specificities of HU (73.2%) and even SUVmax (87.8%) were moderate. The inherent limitations of both morphological and functional imaging modalities, with respect to evaluating malignancy, are well known. These modalities may have complementary value, so cutoff values of the two parameters were applied simultaneously, and the specificity for discrimination between lung cancer and PMF was improved (97.6%). The clinical implication of these results is that PET/CT may have a better ability to distinguish between lung cancer and PMF in pneumoconiosis patients than either PET or CT alone.
Morphological features on chest CT may be used to distinguish between lung cancer and benign mass lesions. In particular, PMF appears as an irregular nodule or mass with calcification, commonly occurring in the upper and middle lung zones and in areas surrounding the emphysematous lung tissue [22]. However, in cases in which malignant lung cancer shows similar radiological findings to PMF, it is difficult to distinguish lung cancer from PMF in pneumoconiosis patients. Furthermore, PMF may grow over time, which could raise suspicion of malignancy. There have been few reports on the use of HU from CT to differentiate between lung cancer and PMF, and we assessed PMF using HU on the CT portion of PET/CT in pneumoconiosis patients. In our study, there was a significant difference in HU between lung cancer and PMF (36.6 ± 9.3 vs. 61.3 ± 19.6, respectively). The high attenuation in PMF is likely due to the coexistence of granulomatous inflammation and calcification [6]. In this study, while 61% (25/41) of PMF had calcification, only 21.4% (9/42) of lung cancer had calcification. The calcification pattern in lung cancer was one or two tiny calcifications located in the peripheral portion of the lung mass. On the other hand, the pattern of calcification in PMF was relatively large, multifocal calcifications with random distribution.
Microscopically, PMF is composed of coal dust, collagen, and elastic fibers, with numerous pigment-laden macrophages and fibroblasts, with or without central necrosis [23]. It has been suggested that increased FDG uptake in PMF is related to active inflammation with fibrosis and may cause false-positive lung cancer results in pneumoconiosis patients [24, 25]. In this study, lung cancer tended to show higher SUVmax than PMF in pneumoconiosis patients. However, there was a partial overlap in the degree of FDG uptake between lung cancer and PMF in this study, and 11 false-positive cases were found when only SUVmax was considered (Fig. 5). Previous studies have reported a relatively low specificity and high rate of false-positive PET diagnoses of lung cancer in patients with underlying pneumoconiosis [14, 21]. To overcome this limitation, we performed additional CT analysis with HU to improve the specificity of differentiation between lung cancer and PMF. When SUVmax and HU were used in combination to distinguish lung cancer from PMF, the number of false positives was reduced from 11 to 1 (Table 3). One factor leading to this discrepancy may be that the previous studies were based only on PET findings of PMF and not on PET/CT findings.
It is known that there is difference in the measured HU for a variety of different CT scanners as well as for different kilovoltage peak settings [26]. In our study, PET/CT scans were acquired using two different scanners of Siemens (Biograph Duo and Biograph TruePoint). When we divided masses into subgroups according to PET/CT scanner, the results were similar regardless of the PET/CT scanner type.
We evaluated only 40 pathologically verified mediastinal LNs, because invasive mediastinal nodal sampling (i.e., via surgery, endobronchial ultrasound, or mediastinoscopy) was not possible in pneumoconiosis patients with poor pulmonary function. In our study, metastatic LNs tended to have more intense FDG uptake, with an asymmetrical pattern, larger size, and lower attenuation than reactive LNs in the mediastinum of pneumoconiosis patients. Although the number of mediastinal LNs included in the analysis was small, our study demonstrated that PET/CT may be useful as a non-invasive method to help discriminate between malignant and reactive nodes in pneumoconiosis patients. Further validation studies with larger number of patients are required.
A limitation of this study was that pathologic confirmation was not available for all pulmonary lesions and mediastinal LNs. We could not assess the clinical impact of mediastinal LN staging with PET/CT, because lung cancer patients with underlying pneumoconiosis generally have poor pulmonary function, precluding them from surgery. In addition, the retrospective nature of the study design and the relatively small number of patients enrolled must be taken into account. Finally, selection bias may have been introduced by the inclusion of only patients with suspected lung malignancy on previous chest CT, with or without contrast enhancement. We plan to perform a further prospective study including data from larger numbers of patients, with a higher rate of pathological confirmation, and analysis of overall survival to assess prognostic value.
In conclusion, PET/CT is useful for the detection of pulmonary malignancy and mediastinal LN staging in patients with underlying pneumoconiosis. SUVmax, DS, DL/S, and HU were useful parameters for differentiating lung cancer from PMF in these patients. When combining PET and CT parameters, a diagnostic advantage may be obtained, with respect to specificity, for distinguishing lung cancer from PMF and for mediastinal LN staging.
Abbreviations
- CT:
-
Computed tomography
- D L :
-
Long-axis diameter
- D L/S :
-
Ratio of long- to short-axis diameter
- D S :
-
Short-axis diameter
- FDG:
-
Fluorodeoxyglucose
- HU:
-
Hounsfield unit
- LN:
-
Lymph node
- NPV:
-
Negative predictive value
- PET:
-
Positron emission tomography
- PMF:
-
Progressive massive fibrosis
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- SUVmax:
-
Maximum standardized uptake value
References
Choi BS, Park SY, Lee JO (2010) Current status of pneumoconiosis patients in Korea. J Korean Med Sci 25:S13–S19
Choi BS (1996) Development of coalworkers’ pneumoconiosis in Korea: risk factors and incidence density. Korean J Occup Environ Med 8:137–152
Jun JS, Jung JI, Kim HR et al (2013) Complications of pneumoconiosis: radiologic overview. Eur J Radiol 82:1819–1830
Garg K, Lynch DA (2002) Imaging of thoracic occupational and environmental malignancies. J Thorac Imaging 17:198–210
Leung CC, Yu IT, Chen W (2012) Silicosis. Lancet 379:2008–2018
Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS (2006) Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics 26:59–77
Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK (2001) Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. JAMA 285:914–924
Weber WA (2006) Positron emission tomography as an imaging biomarker. J Clin Oncol 24:3282–3292
Hurbánková M, Kaiglová A (1993) The changes of some immunological parameters in subjects exposed to asbestos in dependence on age, duration of exposure, radiological findings and smoking habits. Zentralbl Hyg Umweltmed 195:55–65
Madsen PH, Holdgaard PC, Christensen JB, Hoilund-Carlsen PF (2016) Clinical utility of F-18 FDG PET-CT in the initial evaluation of lung cancer. Eur J Nucl Med Mol Imaging 43:2084–2097
Sachpekidis C, Thieke C, Askoxylakis V et al (2015) Combined use of (18)F-FDG and (18)F-FMISO in unresectable non-small cell lung cancer patients planned for radiotherapy: a dynamic PET/CT study. Am J Nucl Med Mol Imaging 5:127–142
Yamamoto Y, Nishiyama Y, Ishikawa S et al (2007) Correlation of 18F-FLT and 18F-FDG uptake on PET with Ki-67 immunohistochemistry in non-small cell lung cancer. Eur J Nucl Med Mol Imaging 34:1610–1616
Kaira K, Oriuchi N, Shimizu K et al (2009) 18F-FMT uptake seen within primary cancer on PET helps predict outcome of non-small cell lung cancer. J Nucl Med 50:1770–1776
Reichert M, Bensadoun ES (2009) PET imaging in patients with coal workers pneumoconiosis and suspected malignancy. J Thorac Oncol 4:649–651
Yu H, Zhang H, Wang Y, Cui X, Han J (2013) Detection of lung cancer in patients with pneumoconiosis by fluorodeoxyglucose-positron emission tomography/computed tomography: four cases. Clin Imaging 37:769–771
Saydam O, Gokce M, Kilicgun A, Tanriverdi O (2012) Accuracy of positron emission tomography in mediastinal node assessment in coal workers with lung cancer. Med Oncol 29:589–594
Lee JW, Kim EY, Kim DJ et al (2016) The diagnostic ability of (18)F-FDG PET/CT for mediastinal lymph node staging using (18)F-FDG uptake and volumetric CT histogram analysis in non-small cell lung cancer. Eur Radiol 26:4515–4523
Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P (2009) The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 4:568–577
Lee JW, Kim BS, Lee DS et al (2009) 18F-FDG PET/CT in mediastinal lymph node staging of non-small-cell lung cancer in a tuberculosis-endemic country: consideration of lymph node calcification and distribution pattern to improve specificity. Eur J Nucl Med Mol Imaging 36:1794–1802
Kanegae K, Nakano I, Kimura K et al (2007) Comparison of MET-PET and FDG-PET for differentiation between benign lesions and lung cancer in pneumoconiosis. Ann Nucl Med 21:331–337
Chung SY, Lee JH, Kim TH, Kim SJ, Kim HJ, Ryu YH (2010) 18F-FDG PET imaging of progressive massive fibrosis. Ann Nucl Med 24:21–27
Bergin CJ, Müller NL, Vedal S, Chan-Yeung M (1986) CT in silicosis: correlation with plain films and pulmonary function tests. AJR Am J Roentgenol 146:477–483
Lapp NL, Parker JE (1992) Coal workers’ pneumoconiosis. Clin Chest Med 13:243–252
Alavi A, Gupta N, Alberini JL et al (2002) Positron emission tomography imaging in nonmalignant thoracic disorders. Semin Nucl Med 32:293–321
Kavanagh PV, Stevenson AW, Chen MY, Clark PB (2004) Nonneoplastic diseases in the chest showing increased activity on FDG PET. AJR Am J Roentgenol 183:1133–1141
Robertson DD Jr, Huang HK (1986) Quantitative bone measurements using x-ray computed tomography with second-order correction. Med Phys 13:474–479
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ie Ryung Yoo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 28.8 kb)
Rights and permissions
About this article
Cite this article
Choi, E.K., Park, H.L., Yoo, I.R. et al. The clinical value of F-18 FDG PET/CT in differentiating malignant from benign lesions in pneumoconiosis patients. Eur Radiol 30, 442–451 (2020). https://doi.org/10.1007/s00330-019-06342-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06342-1