Abstract
Purpose
Pneumodissection is described as a simple method for preventing skin injury during cryoablation of superficial musculoskeletal tumours.
Methods
Superficial tumour cryoablations performed from 2009 to 2015 were retrospectively reviewed. Pneumodissection was performed in 13 patients when the shortest tumour-skin distance was less than 25 mm. Indications were pain palliation (n = 9) and local tumour control (n = 4). Patients, target tumours, technical characteristics and complications up to 60 days post ablation were reviewed. The ice ball-skin distances with and without pneumodissection were compared by a paired t-test and further assessed for association with covariates using ANCOVA.
Results
Technical success for ablation was 12 of 13. The mean shortest tumour-skin distance was 15.0 mm (3.2–24.5 mm). The mean thickness of pneumodissection was 9.6 mm (5.2–16.6 mm) resulting in mean elevation of skin of 3.4 mm (1.2–5.3 mm). Mean shortest ice ball-skin distance after pneumodissection was 10.5 mm (4.2–19.7 mm). No infection or systemic air embolism was noted. No intraprocedural frostbite was observed.
Conclusion
Pneumodissection is feasible, effective and safe in protecting the skin during image-guided cryoablation of superficial tumours.
Key Points
• Frostbite during image-guided cryoablation of superficial tumours is commonly under-reported.
• Frostbites are painful and may introduce infection into the superficial ablation zone.
• Warm compress, saline and CO 2 have shortcomings in protecting the skin.
• Pneumodissection is free, readily available, easy to use and safe and effective.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cryoablation is a well-established technique for treatment of bone tumours [1–6]. This technique relies on image-guided percutaneous placement of applicators into the tumour, and the Joule-Thompson principle of argon and helium gas to rapidly cool or thaw the tissue immediately around the applicator. A sudden drop of temperature exceeding -150 °C or rise in temperature up to +33 °C can be achieved. Cytotoxic effects occur secondary to intracellular and interstitial crystal formation in a combination of freeze and thaw cycles [7].
Different from the various other ablation techniques such as radiofrequency ablation or microwave ablation, cryoablation creates an “ice ball” that offers the advantage of easy visibility on ultrasound (US), computed tomography (CT) and magnetic resonance imaging (MRI) [8]. This allows for close monitoring of the ablation zone, and helps prevent damage to the healthy perilesional structures [9, 10]. However, even with visualization, protective measures are needed to prevent the ice ball from extending into the skin as a critical non-target structure (Fig. 1). Skin ulcers created during ablation increase morbidity by being painful and may provide a route for direct extension of infection into the underlying necrotic tissues of the superficial ablation zone.
a A 69-year-old male with painful lytic metastasis from basal cell carcinoma of skin to the posterior left 12th rib (arrows) despite radiation treatment. b Palliative cryoablation with two Endocare Perc-24 applicators (only one is shown). Extension of ice ball to overlying skin is visible (arrows). This is despite utilization of topical warm compress (arrowheads). Freezing of skin was evident intraprocedurally and a non-blanching bruise developed at the conclusion of cryoablation. A 2-cm skin ulcer developed at this site later and resolved with wound care and conservative management. This patient is not among the study group
Local warm compress applied by physically placing a warm heat source on the skin commonly becomes less effective by the presence of interventional devices in the field and by non-horizontal anatomic angles that work against gravity (Figs. 2 and 3). Although CO2 is used in pneumodissection in the peritoneal cavity to protect other organs, it has not been fully studied as a buffer to protect skin. Its handling is cumbersome, and its rapid absorption requires repeated injections and makes formation of a cushion of gas in subcutaneous tissues unlikely (Fig. 3). Saline has a higher thermal conductivity than gas, which can result in the ablation zone extending to the skin (http://www.engineeringtoolbox.com/thermal-conductivity-d_429.html). It obscures tumour margins on CT imaging, which may negatively affect technical outcomes of ablation. In many instances where protection of skin is deemed inadequate with local warm compress alone and intraprocedural imaging mandates immediate action to avoid frostbite, pneumodissection may be considered the fastest remedy, as it literally needs no additional equipment or time to apply.
a A 66-year-old male with painful lytic metastasis from renal cell carcinoma to the left scapular blade (arrows). This lesion is painful despite radiation treatment. b Two Endocare Perc-24 applicators are in place (only one is shown). c Pneumodissection is done while the probes are on “stick” mode. Arrows show resultant subcutaneous emphysema. Topical warm compress is also in place (arrowhead). Note the inadequate contact of warm compress with skin due to presence of applicator and the non horizontal angle of skin. d Full-size ice ball toward the end of the second freeze cycle (arrows) could have extended to the overlying skin in the absence of pneumodissection. Originally injected pneumodissection has not changed significantly in the approximately 1 hour duration of this ablation intervention. There was no need to repeat pneumodissection throughout this intervention. Low quality of procedural images is due to utilization of low mA to reduce radiation dose to the patient
Therapeutic cryoablation in a 71-year-old patient with history of adenocarcinoma of lung and two prior biopsy-proven bone metastases treated with percutaneous ablation. a PET/CT study shows a small sclerotic FDG avid (PET image not shown) lesion in the left eighth rib (arrow) thought to represent a metastasis. b Intraprocedural CT image with the patient in supine position immediately prior to initiation of cryoablation. A single Endocare Perc-17 cryo applicator is in position. Since gas dissection with CO2 was planned to push the stomach and the splenic flexure of colon away from the target tumour, the same mechanism was chosen to protect skin. A 5 French Yueh Centesis Catheter (Cook Medical, Bloomington, Indiana, USA) is in place (arrow) for peritoneal CO2 gas dissection. A 25-gauge needle was used for subcutaneous CO2 pneumodissection. About 0.5 L CO2 was used for peritoneal dissection and about 50 mL CO2 was used for subcutaneous dissection (asterisks). Subcutaneous CO2 pneumodissection elevated the skin 2.5 mm; however, no contiguous gas pads were discernible. Peritoneal pneumodissection was repeated one more time with the same volume and subcutaneous pneumodissection was repeated two more times during the intervention. c CT image immediately after removal of cryo applicator and Yueh catheter at the conclusion of cryoablation about 60 minutes later. Tract of cryo applicator in residual ice ball is visible (solid arrow). Peritoneal dissection has significantly absorbed (asterisk) and subcutaneous dissection is no longer discernible. Local warm compress is in place (dotted arrow)
The aim of this article is to describe pneumodissection technique as a simple method for preventing skin injury during cryoablation of superficial tumours.
Methods
An institutional review board waiver of consent was obtained for this retrospective study. All image-guided cryoablations of soft tissue and bone tumours performed during a 75-month period spanning January 2009 through March 2015 were reviewed to identify lesions close to the skin for which pneumodissection was utilized. Images taken during the procedure were evaluated for the following parameters: utilization of pneumodissection, target lesion size and location, shortest distance between target lesion and skin before pneumodissection, maximum ice ball size, elevation of skin over the tumour by pneumodissection, thickness of pneumodissection air cushion in the overlying subcutaneous tissues, shortest distance between ice ball and skin after pneumodissection, as well as technical details of each ablation (Fig. 4). All cryoablations were performed with general anaesthesia under computed tomography (CT), positron emission tomography (PET)/CT or magnetic resonance imaging (MRI) guidance using Endocare (Endocare, Inc., Austin Texas, USA) or Galil Medical (Galil Medical Inc., Arden Hills, Minnesota, USA) systems. Ten cases were performed under CT guidance (Figs. 2 and 4), two under MR guidance (Fig. 5) and one under PET/CT guidance. Per institutional standard practice, all patients were given one dose of prophylactic IV antibiotics (cefazolin, or ciprofloxacin if allergic to cefazolin) to cover skin flora. No additional antibiotics were given. As a standard practice, local warm compress (Instant Hot Pack, Cardinal Health, McGaw Park, Illinois, USA) in a sterile shower cap was utilized for all patients.
Palliative cryoablation in a 54-year-old female patient with metastatic breast cancer. a Initial intraprocedural CT imaging with the patient in prone position. The target tumour is a 2.5 cm lytic metastasis in the right posterior iliac bone (white arrow). The solid straight line measures the closest distance between the tumour and the skin (14.7 mm). b Two Endocare Perc-24 applicators are partially seen in this image (white arrows). Local warm compress is in place (dotted arrow). The applicators are intentionally placed at a shallow angle into the tumour to avoid extension of the ice ball into the skin along their shafts. Pneumodissection is in place (asterisks). The solid straight line measures the new closest distance between the tumour and the skin (19.1 mm). Pneumodissection has resulted in 4.6 mm elevation of skin. The average thickness of subcutaneous air cushion measured in at least two points is 8 mm (dotted line showing one point of measurement). No additional air injection was needed throughout this intervention. c Post procedure CT image immediately after removal of applicators approximately one hour after initial pneumodissection. Residual ice ball is visible (white arrows). Pneumodissection is still in place (asterisks). Local warm compress is in place (dotted arrow). This cryoablation was technically successful with no complications and successful clinical outcome
MR-guided cryoablation in a 47-year-old male with a subcentimeter painful right scapular lesion. a axial post-gadolinium fat-saturated T1-weighted image in supine position shows an 8 mm lobulated, well-defined, enhancing, very T2-hyperintense (not shown) mildly expansile lesion in medial border of mid scapular body that has been stable in the past 2 years (arrow). It was thought to possibly represent enchondroma or fibrous dysplasia. Due to its size, location and stability, ablation was planned without biopsy. b The patient is in prone position. An IceSeed Galil cryo applicator (asterisk) is positioned abutting the lateral aspect of the lesion in mid scapular body (arrow). No attempt was made to drill into the bone as the ice ball was expected to grow into the bone and include the lesion. c Pneumodissection in place (asterisks) toward the end the single planned freeze cycle. Local warm compress is in place as our standard practice. Flattening of the surface of ice ball where it contacts air is evident (arrows). This is a visual confirmation of efficient thermal resistance of air
Pneumodissection Technique: Pneumodissection was used when the shortest distance between the target lesion and overlying skin was 25 mm or less and the intended size of the ice ball could potentially reach the skin. Considering uncertainties about the final size of ice ball that could be affected by variables such as applicator size, number, approach and tissue vascularity, an arbitrary 25 mm distance was thought to include most scenarios where an ice ball could potentially reach the skin. Pneumodissection was performed after placing all applicators (on “stick” mode) and obtaining the first set of procedural images. Approximately 10–20 mL room air was gently injected into the subcutaneous tissues under the skin overlying the prospective area of ice ball formation using a syringe and a 25- or 30-gauge needle. Proper depth of injection was visually confirmed by immediate elevation of skin upon injection. The number of punctures was decided at the discretion of the operator, so the skin elevation was visibly covering the area over the ablation zone. Two punctures were enough for most cases. No local anaesthesia was given for pneumodissection. The same syringe and needle used for local anaesthesia for cryoprobe placement was usually used for pneumodissection. The minimum acceptable thickness of injected air within subcutaneous tissues was arbitrarily set to 3 mm. Based on routine intra procedural imaging; additional air was injected to maintain the minimum thickness if needed. No thermocouple was used to monitor the skin temperature, as integrity of the skin could be monitored by intermittent imaging and physical examination intraprocedurally. Intraprocedural frostbite was defined as with the presence of any of the three criteria; 1) extension of ice ball to skin on intraprocedural images; 2) freezing of skin on intraprocedural physical examination where the skin becomes rigid; 3) presence of a non-blanching bruise over the area of the ice ball.
No microparticle filter was used, although our operating rooms are equipped with a ventilation system with five levels of filtration, including two levels of high-efficiency particulate arrestance (HEPA) filters.
Technical success of ablation was defined as the ability to execute the ablation as planned pre-procedurally.
A 5 mm safe minimum distance between ice ball and skin was set arbitrarily based on common recommendation for a 5–10 mm minimum displacement to protect critical organs from collateral damage in thermal ablation interventions.
All ablation patients are seen in Interventional Radiology (IR) clinic 45–60 days post procedure with a contrast-enhanced CT or MRI study. The electronic medical records were reviewed up to 60 days past the date of procedure to assess complications. These included all visits, hospital admissions, notes, phone communications, as well as laboratory and imaging results. Special attention was paid to capture information related to local or systemic infections and skin, neurologic or respiratory issues within this period.
Statistical analysis
Patient demographics, tumour characteristics and ablation parameters were recorded for each case. Means and medians were estimated for tumours’ greatest dimension, minimum distance from skin before pneumodissection, elevation of skin with pneumodissection, as well as the maximum diameter of ice ball and minimum distance of ice ball from the skin after pneumodissection. The presumed distance without pneumodissection was calculated by subtracting the thickness of pneumodissection from the minimum distance between ice ball and skin with pneumodissection in place. An exact Wilcoxon signed rank test was used to evaluate whether the median ice ball–skin distances with and without pneumodissection were significantly different; this is equivalent to testing whether the median thickness of pneumodissection was significantly different from zero. We also graphically examined the association of these distance measures with tumour distance from skin, tumour size and tumour location using scatter plots and box plots. We evaluated the association of median thickness of pneumodissection with these tumour characteristics using an exact Kruskal Wallis test. For analysis purposes, tumour size and tumour distance from skin were dichotomized at the median. Analyses were based on all 13 patients, and included a single technical failure in which pneumodissection was used but the cryoablation could not be completed as planned for an intent-to-treat analysis. p < 0.05 was considered statistically significant. All analyses were performed using SAS version 9.4 (Cary, NC).
Results
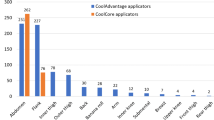
Patient demographics and technical characteristics of the study group are listed in Table 1. Thirteen patients (male n = 9, female n = 4) with the mean age of 59 years (3–79 years, median 64 years) were included in this study. The majority of lesions were metastases (n = 11) with one recurrent sarcoma and one benign bone lesion (enchondroma or fibrous dysplasia). The indications were palliation of pain (n = 9) or local control (n = 4). The tumours had a mean diameter of 37.2 mm (10.0–71.1 mm, median 33.73 mm). The mean shortest distance between the lesion and the skin was 15.0 mm (3.2 to 24.5 mm; median 15.7 mm). The mean elevation of skin by pneumodissection was 3.4 mm (1.2–5.3 mm, median 3.3 mm). The mean thickness of pneumodissection air cushion in the overlying subcutaneous tissues was 9.6 mm (4.9–16.6 mm, median 9.5 mm). The elevation of skin was not equal to the thickness of the pneumodissection layer. This is probably due to the less dense air replacing denser soft tissues. The mean maximum diameter of the ice ball was 60.1 mm (35.2–149.1 mm; median 53.6 mm). The mean shortest distance between ice ball edge and skin after pneumodissection was 10.5 mm (4.2–19.2 mm; median 9.2 mm). When comparing ice ball and skin distance with and without pneumodissection in place, the difference was significant, or equivalently, the thickness of pneumodissection was significantly different from zero (p < 0.001), suggesting that the minimum acceptable air pocket thickness was successfully maintained during cryoablation. In all but one patient, the presumed distance without pneumodissection was less than 5 mm. This 5 mm distance may represent a ‘safe’ minimum distance between ice ball and skin, as no patients experienced intraprocedural frostbite in this case series. Without pneumodissection, the predicted ice ball to skin distance would be less than 5 mm in 12 of 13 cases (Fig. 6). Tumour distance from skin, tumour size, and anatomic location were not significantly associated with median thickness of pneumodissection.
Dot plot of minimum ice ball-skin distance with and without pneumodissection with means and standard deviations. The ice ball to skin distance without pneumodissection was calculated by subtracting the thickness of the pneumodissection layer from the ice ball to skin distance with pneumodissection. The dotted line depicts a potential “safe” minimum 5 mm distance between ice ball and skin. In the absence of pneumodissection, all but one ice ball breach the safe distance toward the skin and five ice balls grow through the skin (0 mm point)
Technical details of ablation interventions, including the number of applicators, the systems used, number of freeze-thaw cycles and the duration of cycles, are outlined in Table 1.
In cases where the applicators provided temperature readings (Endocare), cytotoxic temperatures were achieved within a range of -120 °C to -159 °C. In cases where the applicators did not provide temperature reading (Galil), a thermocouple was not used and adequacy of ablation was assessed by imaging confirmation of progression of ice ball to include the target tumour and intended margin.
Pneumodissection was required only once at the start of the intervention for 11 patients. Additional pneumodissection (10–20 mL) to maintain the minimum 3 mm thickness of subcutaneous air was needed during cryoablation in two patients with prolonged intervention times of more than 120 minutes (patients 4 and 5, Table 1).
No infection or systemic air embolism was noted in any patients (0/13). No intraprocedural frostbite was noted in any of the study patients (0/13).
In one patient with technically unsuccessful palliative cryoablation of a left posterior lateral rib metastasis (patient 4, Table 1), despite lack of intraprocedural frostbite , a 2-cm non-blanching bruise was noted on the skin the next day. This turned into a shallow ulcer on follow-up visit 9 days after ablation. The ablation could not be executed as planned, due to irresolvable adhesion of tumour to the splenic flexure of colon requiring several time-consuming manoeuvres. We hypothesized that the residual ice ball at the conclusion of ablation damaged the overlying skin during the recovery period when the patient was lying on this site. The patient’s comorbidities such as diabetes, coronary artery disease, cachectic body habitus and chemotherapy-induced mucusitis may have contributed to formation of a skin ulcer. The ulcer was healed with conservative management (SIR complication class minor B).
A patient with prostate cancer and cryoablation of a painful left 6sixh rib metastasis developed moderate left pleural effusion requiring thoracentesis 6 days after ablation. (SIR complication class minor B).
Discussion
Percutaneous ablative techniques have evolved into a useful modality for treatment or palliation of tumours of the musculoskeletal system [11]. These techniques include chemical ablation (ethanol or acetic acid), laser ablation, radiofrequency ablation, microwave ablation, cryoablation, high intensity focused ultrasound and irreversible electroporation. In the application of these techniques, it is imperative to take measures to protect the critical non-target structures in the vicinity of the target lesion.
Common non-target critical structures in body IR domain include skin, bowel and nerves. A variety of protective measures are available, including gas dissection, hydrodissection and warming/cooling compressions for skin protection. Protection may also be achieved by continuous temperature monitoring in the area using thermocouples, and by monitoring of nerve at risk using neurodiagnostic EEG, EMG and evoked potential electrodes with accessories [12]. Some protective measures are planned in advance and some are required on an urgent basis during an ablation intervention. The various protective techniques carry unique advantages and disadvantages, and defining their specific applicability in the different clinical settings is important [13].
Skin ulcers created during ablation are painful and may provide a route for direct extension of infection into the necrotic tissues of the superficial ablation zone. It is likely that the prevalence of intraprocedural frostbite is under-reported, as the integrity of skin is shadowed by the primary objective of a cryoablation intervention [14]. Currently, the common practice for protecting the overlying skin during cryoablation is to use hydrodissection with saline or lidocaine, gas dissection with CO2 and local warm compress [1–3, 6, 14].
Local warm compression is the easiest and least expensive method. However, due to the presence of physical obstacles in the ablation region, including cryoablation applicators, and asymmetric shapes of the heat containers (i.e. gloves), and the anatomic challenges of keeping the source of heat on the skin in non-horizontal angles, warm compress alone cannot protect the skin (Figs. 1 and 2). Saline is easy to apply. It may need to be warmed before use, which adds another step to its utilization. The limitations of using saline are that it may freeze and extend the ice ball to the skin [1, 14]. Additionally, it obscures tumour margins on CT imaging, which may negatively affect technical outcomes of ablation [14]. Addition of diluted water-soluble contrast material to saline may be needed to overcome this problem.
Gas buffers such as CO2 and air work by two mechanisms; 1) displacing the skin away from the ice ball, and 2) decreasing the subcutaneous tissue’s thermal conductivity (cushion of gas replacing water-containing soft tissues).
Both CO2 and air are easily visible on CT and MRI and are excellent insulators, each having a much lower thermal conductivity than water (saline). The thermal conductivity of CO2, air and water are 0.014–0.016 W/m.K, 0.024–0.025 W/m.K and 0.56–0.59 W/m.K, respectively (http://www.engineeringtoolbox.com/thermal-conductivity-d_429.html).
Compared to air, CO2 is relatively expensive, cumbersome to use and requires repeated injections due to its rapid absorption rate. Air is readily available, free of charge and does not require special handling or equipment for delivery.
Hypothetical arguments against the use of pneumodissection have included: 1) CO2 being a better insulator than air (0.014–0.016 W/m.K for CO2 vs. 0.024–0.025 W/m.K for room air), and 2) the potential risk of infection and air embolism associated with air. Given that the difference in thermal conductivity between CO2 and air is small but both are much lower than water (20-40 times), we expect no major difference in the effectiveness of either material in protecting the skin from freezing. Rapid solubility of CO2 probably makes it unlikely to form a cushion of gas in the subcutaneous tissues, and requires repeated injections during an ablation intervention (Fig. 3). This is unlikely with air. Hypercarbia along with other complications from utilization of CO2 in laparoscopic surgeries have been reported and can be of concern in select patients with poor respiratory reserve [15]. Awareness of this issue when planning cryoablation in patients with poor respiratory reserve is important.
Two of the potential complications of injecting air into the subcutaneous tissue and causing iatrogenic subcutaneous emphysema are air embolization and infection. A review of the literature on iatrogenic subcutaneous emphysema originating from lung procedures shows that air embolism and infection are extremely rare [16–21]. The air, even in large volumes, is expected to reabsorb over time once the underlying problem is resolved.
Approximately 10–40 ml of air was injected in the patients in this case series. Therefore, when compared to reported cases of subcutaneous emphysema, the volume of air used in our case series was significantly smaller. Additionally, the air used for pneumodissection is the operating room air, which has been through several layers of filtration and injected under sterile percussions. Therefore, theoretically, operating room air used for pneumodissection is more purified compared to ordinary air. For the above reasons, systemic air embolism and infection are expected to be extremely unlikely from intraprocedural pneumodissection as described here.
Pneumodissection has been reported as a protective technique in cryoablation of small renal masses [22].
Utilization of air as an ingredient of foam sclerotherapy in different organs such as venous vascular malformations, varicocele and portal vein, among others, is well reported in the literature [23–26]. Utilization of air in subcutaneous tissues for pneumodissection should not carry higher risk for complications compared to its accepted use in foam sclerotherapy in other organs. In this case series, none of the patients developed infection or air embolization.
One patient in this series developed frostbite during the recovery period while lying supine on the residual ice ball. Comorbidities such as cachectic body habitus , mucusitis and irresolvable adhesions probably facilitated this outcome. Based on this case and another patient with the same outcome (not in this series), we changed our standard practice such that all patients who undergo superficial cryoablation will receive local warm compress throughout the recovery period. Also, organ displacement will be performed first before initiation of cryoablation to avoid complications from irresolvable adhesions.
This study has several limitations, including its retrospective design, lack of a control group and the small patient population.
Pneumodissection technique is readily available and easy to use when protection of skin is urgently needed, particularly when rapid, unexpected growth of ice ball is detected on intra procedural images.
In conclusion, pneumodissection can be added to the armamentarium of interventional radiologists as an easy and readily available method for skin protection during image-guided percutaneous cryoablation of superficial musculoskeletal tumours. Based on this small case series, pneumodissection is recommended when the lesion is 2.5 cm from the skin surface. Additionally, pneumodissection of 10 mm that results in average of 3.4 mm of skin elevation can effectively prevent skin injury during image-guided cryoablation of superficial bone and soft tissue tumours.
References
Buy X, Tok CH, Szwarc D, Bierry G, Gangi A (2009) Thermal protection during percutaneous thermal ablation procedures: interest of carbon dioxide dissection and temperature monitoring. Cardiovasc Intervent Radiol 32:529–534
Filippiadis DK, Tutton S, Maxioti A, Kelekis A (2014) Percutaneous image-guided ablation of bone and soft tissue tumors: a review of available techniques and protective measures. Insights Imaging 5:339–346
Filippiadis DK, Maxioti A, Velonakis G et al (2013) Percutaneous image guided ablation of bone and soft tissue tumors: how to avoid complications. Scientific Exhibit ESSR. doi:10.1594/esst2013/P-0127
Kurup AN, Callstrom MR (2010) Image-guided percutaneous ablation of bone and soft tissue tumors. Semin Interv Radiol 27:276–284
Rosenthal D, Callstrom MR (2012) Critical review and state of the art in interventional oncology: benign and metastatic disease involving bone. Radiology 262:765–780
Callstrom MR, Dupuy DE, Solomon SB et al (2013) Percutaneous image- guided cryoablation of painful metastases involving bone: multicenter trial. Cancer 119:1033–1041
Erinjeri JP, Clark TWJ (2010) Cryoablation: mechanism of action and devices. J Vasc Interv Radiol 21:S187–S191
Maybody M, Solomon SB (2007) Image-guided percutaneous cryoablation of renal tumors. Tech Vasc Interv Radiol 10:140–148
Friedman MV, Hillen TJ, Wessell DE, Hildebolt CF, Jennings JW (2014) Hip chondrolysis and femoral head osteonecrosis: a complication of periacetabular cryoablation. J Vasc Interv Radiol 25:1580–1588
Prologo JD, Patel I, Buethe J, Bohnert N (2014) Ablation zones and weight-bearing bones: points of caution for the palliative interventionalist. J Vasc Interv Radiol 25:769–775
McMenomy BP, Kurup AN, Johnson GB et al (2013) Percutaneous cryoablation of musculoskeletal oligometastatic diseasefor complete remission. J Vasc Interv Radiol 24:207–213
Marshall RH, Avila EK, Solomon SB, Erinjeri JP, Maybody M (2016) Feasibility of intraoperative nerve monitoring in preventing thermal damage to the ”nerve at risk” during image guided ablation of tumors. Cardiovasc Intervent Radiol 39(6):875–884
Tsoumakidou G, Buy X, Garnon J, Enescu J, Gangi A (2011) Percutaneous thermal ablation: how to protect the surrounding organs. Tech Vasc Interv Radiol 14:170–176
Griauzde J, Gemmete JJ, Farley F (2015) Successful treatment of a musculoskeletal tumor society grade 3 aneurysmal bone cyst with N-butyl cyanoacrylate embolization and percutaneous cryoablation. J Vasc Interv Radiol 26:905–909
Worrell JB, Cleary DT (2002) Massive subcutaneous emphysema and hypercarbia: complications of carbon dioxide absorption during extraperitoneal and intraperitoneal laparoscopic surgery - case studies. AANA J 70:456–461
Jones PM, Hewer RD, Wolfenden HD, Thomas PS (2001) Subcutaneous emphysema associated with chest tube drainage. Respirology 6:87–89
Lostoridis E, Tourountzi P, Pouggouras K, Koutsouki S, Lampiri K, Nagy EO (2015) Pneumoscrotum after tracheal intubation. Acta Anaesthesiol Taiwanica 53:44–46
Cefolio RJ, Bryant AS, Maniscalco LM (2008) Management of subcutaneous emphysema after pulmonary resection. Ann Thorac Surg 85:1759–1763, discussion 1764-5
Ovári A, Just T, Dommerich S et al (2014) Conservative management of post-intubation tracheal tears-report of three cases. J Thorac Dis 6:E85–E91
Martí de Gracia M, Gutiérrez FG, Martínez M, Dueñas VP (2009) Subcutaneous emphysema: diagnostic clue in the emergency room. Emerg Radiol 16:343–348
Schneider T, Storz K, Dienemann H, Hoffmann H (2007) Management of iatrogenic tracheobronchial injuries: a retrospective analysis of 29 cases. Ann Thorac Surg 83:1960–1964
Maurice MJ, Haaga JR, Nakamoto DA, Ponsky LE (2013) Pneumodissection: an alternative protective technique for the percutaneous cryoablation of small renal masses. Urol Int 90:381–383
Gandini R, Konda D, Reale CA et al (2008) Male varicocele: transcatheter foam sclerotherapy with sodium tetradecyl sulfate—outcome in 244 patients. Radiology 246:612–618
Fischman AM, Ward TJ, Horn JC et al (2014) Portal vein embolization before right hepatectomy or extended right hepatectomy using sodium tetradecyl sulfate foam: technique and initial results. J Vasc Interv Radiol 25:1045–1053
Gandini R, Chiocchi M, Konda D, Pampana E, Fabiano S, Simonetti G (2008) Transcatheter foam sclerotherapy of symptomatic female varicocele with sodium-tetradecyl-sulfate foam. Cardiovasc Intervent Radiol 31:778–784
McCafferty I (2015) Management of low-flow vascular malformations: clinical presentation, classification, patient selection, imaging and treatment. Cardiovasc Intervent Radiol 38:1082–1104
Acknowledgments
The scientific guarantor of this publication is Majid Maybody, MD. The authors of this manuscript declare relationships with the following companies: None. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
This study has received funding by a Cancer Center Support Grant from the National Cancer Institute (P30 CA008748). Chaya Moskowitz and Meier Hsu kindly provided statistical advice for this manuscript. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. No study subjects or cohorts have been previously reported. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maybody, M., Tang, P.Q., Moskowitz, C.S. et al. Pneumodissection for skin protection in image-guided cryoablation of superficial musculoskeletal tumours. Eur Radiol 27, 1202–1210 (2017). https://doi.org/10.1007/s00330-016-4456-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4456-6