Abstract
Objectives
To evaluate the influence of scan duration on pharmacokinetic parameters and their performance in differentiating benign from malignant breast lesions.
Methods
Dynamic breast imaging was performed on a 3.0-T MR system using a prototype CAIPIRINHA-Dixon-TWISTVIBE (CDT-VIBE) sequence with a temporal resolution of 11.9 s. Enrolled in the study were 53 women with 55 lesions (26 benign and 29 malignant). Pharmacokinetic parameters (Ktrans, ve , kep and iAUC) were calculated for various scan durations from 1 to 7 min after injection of contrast medium using the Tofts model.
Results
Ktrans, kep and ve calculated from the 1-min dataset were significantly different from those calculated from the other datasets. In benign lesions, Ktrans, kep and ve were significantly different only between 1 min and 2 min (corrected P > 0.05), but in malignant lesions there were significant differences for any of the comparisons up to 6 min vs. 7 min (corrected P > 0.05). There were no significant differences in AUCs for any of the parameters (P > 0.05).
Conclusions
In breast dynamic contrast-enhanced MRI the scan duration has a significant impact on pharmacokinetic parameters, but the diagnostic ability may not be significantly affected. A scan duration of 5 min after injection of contrast medium may be sufficient for calculation of Tofts model pharmacokinetic parameters.
Key Points
• Scan duration of DCE-MRI breast imaging has a significant impact on pharmacokinetic parameters
• A scan duration of less than 2 min results in spurious parameter estimates
• The initial 2 min are important for both benign and malignant lesions
• In malignant lesions the impact extends to 4 – 6 min
• The differentiation ability of parameters may not be affected by scan duration
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The hypervascularity and increased permeability of malignant breast lesions are believed to contribute to a fast wash-in and delayed wash-out pattern in dynamic contrast-enhanced studies, while benign lesions usually show a slow/medium wash-in and persistent enhancement in the delayed phase [1, 2]. The underlying information in the signal intensity changes can be explored by dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) and used for the differentiation between benign and malignant breast lesions.
Typically, there are three methods available for the analysis of signal intensity changes: qualitative, semiquantitative and quantitative methods. Compared with the first two methods, quantitative analysis is more objective and accurate because it provides pharmacokinetic parameters that directly reflect the physiological properties of tissue, including vessel permeability, perfusion and the volume of the extravascular/extracellular space (EES). It has been shown that quantitative analysis can potentially improve the accuracy of breast lesion diagnosis [3–6] and is valuable in monitoring responses to neoadjuvant chemotherapy [7–9]. However, the quantitative method has not been adopted as part of routine breast MRI because of several limitations, a major one being the difficulty in obtaining high temporal and spatial resolution using conventional sequences.
Recently, the CAIPIRINHA-Dixon-TWIST volume-interpolated breath-hold examination (CDT-VIBE) technique with a high spatial and temporal resolution has been evaluated with promising results in liver imaging [10], and this technique might be able to improve the temporal resolution of breast DCE-MRI with preserved spatial resolution. In this study, according to the recommendations of the American College of Radiology practice guidelines for the performance of breast DCE-MRI [11] regarding spatial resolution, CDT-VIBE was configured with a temporal resolution of 11.9 s and an isotropic spatial resolution of 1 mm.
With such a temporal resolution, whether the scan duration can be reduced to further reduce motion artefacts and to improve patient comfort is still unclear. In this study, a CDT-VIBE DCE-MRI was performed in patients with pathologically confirmed benign and malignant breast lesions. The aim was to determine a feasible scan duration by evaluating the influence of scan time on pharmacokinetic parameters and performance in diagnosing breast lesions.
Materials and methods
Patients
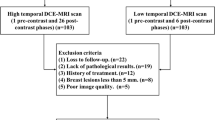
This study was approved by our institutional review board and all patients gave written consent to the examination. From 19 August 2013 to 20 December 2013, 61 consecutive patients were referred for breast MRI because of suspicious findings on ultrasonography or mammography (36 patients), for presurgery evaluation (18 patients) and for short-interval (3–6 months) follow-up (7 patients). Of these 61 patients, 8 were excluded because of small lesion size (maximum diameter <1 cm) that might compromise the accuracy of quantitative analysis (5 patients), no positive findings (2 patients) and poor patient cooperation (1 patient). Thus 53 patients (median age 44 years, range 25 – 83 years; all women) with 55 lesions were included.
Magnetic resonance imaging
All examinations were performed on a 3.0-T MR system (MAGNETOM Skyra; Siemens Healthcare, Erlangen, Germany) with a four-channel phased-array breast coil. Patients were examined in the prone position. Breast compression was not applied.
Dynamic imaging was performed with a prototype CDT-VIBE sequence. The protocol consisted of 1 min 9 s for T1 mapping and 8 min 20 s for DCE imaging (40 phases in total). A method involving two flip angles (2° and 14°) was used for T1 mapping. The same field of view (320 × 320 × 154 mm) and spatial resolution (1 × 1 × 1 mm) were used for the transverse T1 mapping and DCE imaging protocol.
The basic principle of CAIPIRINHA has been described in detail previously [2, 3]. In this study, a CAIPIRINHA 2 × 2 – 1 sampling strategy was applied with 50 % slice oversampling. The values of the TWIST view-sharing parameters A and B were both selected as 20 % with forward sharing strategy, resulting in a time resolution of 11.9 s for each phase except the first TWIST frame (35 s, full k-space sampling). A and B represent the central region and the peripheral portion of the k-space, respectively. These values were selected based on the findings of a kidney MR angiography study that showed less than 5 % errors in a TWIST DCE-MRI signal intensity time-course with both A and B set at 20 %, compared to an acquisition with full k-space sampling [12]. The values selected were higher than in other studies of TWIST-based breast imaging [13–15].
For the Dixon-based water–fat separation, echo times were chosen for in-phase and opposite-phase conditions (2.46 ms and 3.69 ms). Although fat saturation is not mandatory for breast DCE-MRI, it is difficult for the patient to remain motionless for the imaging time of 5 – 10 min, and any motion leads directly to a failure of subtraction. Therefore, the Dixon method was used in this study, although it requires a longer TR for the generation of in-phase and opposite-phase echoes. A gadodiamide contrast medium (Omniscan; GE Healthcare) was power-injected (Spectris Solaris EP; Medrad, Pittsburgh, PA) with the beginning of the fourth phase of CDT-VIBE sequences at a dose of 0.1 mmol/kg and a rate of 3 mL/s. A total volume of 20 mL saline was subsequently injected to flush in all contrast medium.
Data processing
The dataset that began to show contrast medium filling in the heart and its arteries was marked as the first postcontrast phase. All precontrast CDT-VIBE phases were combined with different postcontrast phases (1 – 5, 1 – 10, 1 – 15, 1 – 20, 1 – 25, 1 – 30 and 1 – 35) to form seven dynamic series sets. The corresponding postcontrast scan durations ranged from 1 to 7 min. The whole processing flow is presented in Fig. 1.
Flow chart of CDT-VIBE dynamic data processing. The image set that showed contrast medium filling the heart and its arteries was marked as the first post-contrast phase. All precontrast sequences and different phases of postcontrast sequences (1 – 5, 1 – 10, 1 – 15, 1 – 20, 1 – 25, 1 – 30 and 1 – 35) were used to form seven sets of dynamic series with postcontrast imaging duration ranging from 1 min to 7 min
The T1 maps and dynamic series with different scan durations were uploaded to a workstation and analysed using dedicated software for pharmacokinetic analysis (Tissue 4D; Siemens Healthcare). Initially, motion correction was performed automatically with the first dynamic image set as reference. The motion-corrected dynamic phases were then registered to T1 maps. The fifth postcontrast dynamic dataset (acquired at 1 min after contrast medium injection) was used to set up regions of interest (ROIs). ROIs were manually drawn over the most enhancing component of the lesion. Time–intensity curves were calculated for all ROIs. Pharmacokinetic evaluation was based on the two-compartment Tofts model and a population average arterial input function (intermediate type) provided by Tissue 4D.
After obtaining voxel-wise pharmacokinetic maps, the drawn ROIs were copied to the same spatial position. The median of four parameters within the drawn ROIs, including Ktrans (volume transfer constant between plasma and EES), ve (EES volume), kep (constant flux rate between EES and plasma) and iAUC (area under the curve for the initial 60 s), were recorded. Finally, seven sets of quantitative parameters from different scan durations were generated. Data processing was performed by one radiologist with more than 5 years experience in breast MR imaging under the supervision of a senior radiologist with more than 10 years experience in breast MR imaging. They were both blinded to the patients’ clinical history and other examination results. Figure 2 shows voxel-wise parametric maps for malignant (invasive ductal carcinoma, Fig. 2a) and benign (fibroadenoma, Fig. 2b) breast lesions.
Statistical analysis
A single-sample K-S test was used to test whether Ktrans, kep, ve and iAUC were normally distributed. If these parameters were normally distributed, a paired t-test with Bonferroni correction was used to identify significant differences in the seven sets of pharmacokinetic parameters for benign and malignant breast lesions, respectively. Otherwise, a nonparametric test would be used. Statistical analysis was performed using SPSS 21. Receiver operating characteristic curve (ROC) analysis and pair-wise comparison of areas under the curve (AUC) with Bonferroni correction were used to assess the diagnostic efficiency of the parameters. ROC analysis was performed using Medcalc (12.5.7). P values <0.05 were considered to indicate statistical significance.
Results
Pathological diagnosis
Among 53 patients included in this study, 17 received core needle biopsy under ultrasound guidance, 29 received lumpectomy after wire localization and 7 received mastectomy. Pathological assessment was performed on 55 lesions in 53 patients and revealed 29 malignant lesions (18 invasive ductal carcinomas and 5 ductal carcinoma in situ) and 26 benign lesions (11 fibrocystic changes, 6 fibroadenomas and 3 papillomas). The 55 lesions ranged in size from 7 mm to 78 mm with a mean of 35 mm.
Changes in pharmacokinetic parameters with different scan durations
Figure 3 shows the values of the pharmacokinetic parameters in relation to scan duration for all benign and malignant lesions. The paired t-test results for the value of the parameters with different scan durations in benign and malignant lesions are summarized in Table 1.
Scatter plots of pharmacokinetic parameter values in relation to scan duration for all benign lesions (purple) and malignant lesions (yellow). The black solid and dashed lines represent mean values for the malignant and benign lesions respectively, and the corresponding values are shown in the table below
The 1-min mean Ktrans values (0.149 min−1 and 0.383 min−1 for benign and malignant lesions, respectively) were higher than the 2-min Ktrans values (0.126 min−1 and 0.276 min−1, respectively), and the 7-min Ktrans values showed slight increases (0.147 min−1 and 0.313 min−1, respectively). The percentage changes in the 1-min to 6-min Ktrans values in relation to the mean 7-min value, i.e. (Ktrans[x] − Ktrans[7 min])/Ktrans[7 min], were 2 %, −14 %, −12 %, −6 %, −3 % and −2 % in benign lesions and 23 %, −12 %, −13 %, −8 %, −3 % and −3 % in malignant lesions, respectively. The differences in Ktrans in benign lesions between 1 min and 2 min and between 1 min and 3 min were significant (corrected P < 0.001 and corrected P = 0.02, respectively). In malignant lesions, there were significant differences in all paired Ktrans values (corrected P < 0.05), except between 2 min and 3 min, between 2 min and 4 min and for all pairs among 5 min, 6 min and 7 min (corrected P > 0.05).
The mean 1-min kep values (0.769 min−1 and 1.255 min−1 for benign and malignant lesions, respectively) were higher than the 2-min values (0.399 min−1 and 0.699 min−1, respectively). The 3-min values were also lower but the decreases were more moderate (0.328 min−1 and 0.644 min−1, respectively). From 3 min to 7 min, there were slight increases in both benign and malignant lesions (0.363 min−1 and 0.747 min−1, respectively, at 7 min). The percentage changes in the 1-min to 6-min kep values in relation to the mean 7-min value were 112 %, 10 %, −10 %, −8 %, −6 %, and −2 % in benign lesions and 68 %, −6 %, −14 %, −12 %, −6 % and −3 % in malignant lesions, respectively. In benign lesions, the differences in kep between 1 min and all other scan durations (corrected P < 0.001) and the difference between the 2-min and 3-min values (corrected P = 0.03) were significant. In malignant lesions, there were significant differences in all paired kep values (corrected P < 0.05) except between 2 min and 4 – 7 min, between 3 min and 4 min and between 6 min and 7 min (corrected P > 0.05).
The changes in mean ve values were in contrast to the changes in Ktrans and kep. From 1 min to 4 min, ve in benign lesions increased from 0.226 to 0.466 and in malignant lesions from 0.352 to 0.480. With longer scan durations, ve in benign and malignant lesions gradually decreased and reached 0.459 and 0.445, respectively, by 7 min. The percentage changes in the 1-min to 6-min ve values in relation to the mean 7-min value were −51 %, −17 %, −5 %, 2 %, 0.5 % and −1 % in benign lesions and −21 %, 0.3 %, 7 %, 8 %, 5 % and 1 % in malignant lesions, respectively. The differences in ve between benign and malignant lesions diminished with increasing scan duration. In benign lesions, there were significant differences between the 1-min value and the values for all other scan durations, and between the 2-min values and 4-min, 5-min and 7-min values (corrected P < 0.05). In malignant lesions, there were significant differences between the 1-min value and the values for all other scan durations, between the 2-min values and the 3-min and 4-min values, between the 4-min values and the 6-min and 7-min values and between the 5-min values and the 6-min and 7-min values (corrected P < 0.001).
Mean iAUCs in benign and malignant lesions showed good consistency with the various scan durations. The percentage changes in the 1-min to 6-min iAUC in relation to the 7-min value were −7 %, −3 %, −5 %, −1 %, −3 % and −2 % in benign lesions and 2 %, 3 %, 2 %, 2 %, 0.3 % and 0.2 % in malignant lesions. There were no significant differences among any of the iAUC values (P > 0.05).
ROC analysis
For Ktrans the highest AUC value of 0.932 was for the 1-min scan duration. With increased imaging time, the AUC values decreased and reached 0.885 at 7 min. The AUCs for kep showed a consistent increase from 0.824 at 1 min to 0.913 at 5 min, but decreased to 0.893 at 6 min and 0.888 at 7 min. The highest AUC of 0.703 for ve was also seen at 1 min, but the AUC values dropped dramatically to below 0.6 from 2 min. The AUCs for iAUC showed good consistency with the various scan durations. There was no significant difference among AUC pairs for the seven sets of Ktrans, kep, ve and iAUC (P > 0.05). The AUCs for the different scan durations are shown in Table 2.
Discussion
The aim of this study in a cohort of 53 patients who underwent high temporal and spatial resolution dynamic CDT-VIBE imaging to 7 min after injection of contrast medium was to determine a feasible dynamic scan duration by investigating its influence on parameter estimates and diagnostic performance.
In previous studies with temporal resolutions of 2 – 6 s, computer simulation approaches were used to investigate the influence of scan time on parameter estimates [16, 17]. Changes in preset parameters with various simulated scan durations were recorded. The calculated values of Ktrans and ve with scan durations less than 2 min were significantly different from preset values and the deviations became worse with shorter scan durations. In this study, the imprecise estimation of Ktrans and ve with imaging times less than 2 min was in agreement with the findings of previous experimental studies.
In this study, mean Ktrans and ve for the 1-min scan duration were significantly different from the values for the other scan durations, as was mean kep. This deviation in the estimates was significantly less with a scan duration of 2 min and reached a relatively stable state with a duration of 3 min. In a study by Jena et al., high temporal resolution (4.4 s) T1-weighted images were acquired up to 90 s in 36 lesions (16 benign and 20 malignant) [18]. They measured Ktrans from 30 s to 90 s with an interval of 10 s and found a decrease from 10.809 to 2.194 for malignant lesions and from 4.446 to 0.189 for benign lesions. Despite differences in the technique and analysis methods, the changes in Ktrans with varying scan durations were very similar to the findings in the current study. The consistency in clinical and experimental results indicates that deviations in parameters with a scan duration of 1 min may not be a true reflection of lesion features, but overestimation and underestimation caused by incomplete data acquisition.
Compartment models, such as the Tofts model, used for T1-weighted dynamic contrast-enhanced data assume instantaneous mixing of intravenously injected contrast medium and ignore first-pass effects of bolus injection [19, 20]. The early phase of contrast enhancement (referred to as the first pass in bolus injection studies) involves the contrast medium arriving via the arterial supply and constantly mixing into the blood plasma and the closely coupled compartments [21, 22]. This mixing phase might last up to about 2 min [23], which coincides with the imprecise scan duration of 2 min found in this study. Thus, incomplete contrast medium transfer during the 2 min after injection may be the underlying reason for the spurious parameter estimates. Therefore, a scan time of less than 2 min is not appropriate for compartmental analysis.
Significant changes in individual parameters with varying scan durations were also observed in this study. In benign and malignant lesions, the fast concentration of contrast medium in plasma and EES within the first 2 min after injection produced significant changes in Ktrans, kep and ve between 1 and 2 min and other scan durations. However, dynamic imaging times from 3 to 7 min revealed different responses from benign and malignant lesions. In benign lesions, there were no significant differences in the three Tofts parameters, while in malignant lesions significant differences existed until the last 6-min vs. 7-min comparison. A possible explanation is that the transfer of contrast medium between plasma and EES in benign lesions may be stable during the 3 – 7 min after injection, but in malignant lesions the 3 – 6 min after injection corresponds to the delayed wash-out phase and the variable contrast medium reflux rate between EES and plasma has a significant effect on parameter values. Therefore, prolonging dynamic imaging to collect adequate delayed information is necessary, especially for malignant lesions. Thus, reported pharmacokinetic parameters from some previous studies [24–26] in which a high spatial resolution sequence of 1 – 3 min was inserted between ultrafast dynamic sequences with lower spatial resolution to compensate for missed morphological information might be inaccurate because the inserted sequence generally occurred during the 2 – 6 min after contrast medium injection.
Parameter values were significantly influenced by the scan duration, but discrimination of benign from malignant lesions was not. The best Ktrans AUC produced with the 1-min imaging time might be derived from overestimation of the Ktrans value. Although it did improve the diagnostic performance (but not statistically significantly), it is unknown whether this advantage would persist or introduce extra uncertainty into the parameter estimation. To answer these questions, more clinical application and verification are needed in future studies. The consistent increase in kep AUC with increasing imaging time may be caused by the efflux of contrast medium from the tissue back to the plasma which usually appears after 2 min in breast lesions [1, 23]. Clinically, Ktrans is more widely used for differentiation and monitoring treatment response, while the clinical value of kep and ve is discrepant between studies [4, 18, 24, 25]. However, Ktrans is influenced by any condition correlated with blood perfusion, for example cardiac output and hypertension, while kep is not [27]. Thus kep may be a more accurate indicator of tumour capillary permeability. In this study, kep showed reliable and comparable AUC values. And the best diagnostic performance with kep was achieved with a scan duration of 5 min.
Considering the fact that ve had minor diagnostic value and iAUC was not an effective variable in the current circumstances, the determination of the optimized imaging time was based on Ktrans and kep. For Ktrans and in benign lesions kep, the dynamic data collected during the 6-min and 7-min scans did not show significant changes in the parameter estimates. Although there was a significant difference in kep in malignant lesions between 5 min and 6 and 7 min, kep produced the best AUC with the 5-min scan duration. Moreover, scan durations above 5 min did not improve the diagnostic performance of any of the parameters. Therefore, a scan duration of 5 min for adequate wash-in and wash-out information may be a conservative but reasonable choice. It should be noted that the best Ktrans AUC with 1 min was not taken into consideration. The more prominent overestimation of Ktrans in malignant lesions with a scan duration of 1 min enhanced its differentiation performance, but before solid evidence can verify the effectiveness of this overestimation, a cautious attitude should still be adopted. But the potential to improve the diagnostic value of Ktrans with shorter scan durations, such as 2 min, was raised for further discussion and confirmation.
There were two major technical limitations in this study. First, although the TWIST technique has been used for ultrafast DCE-MRI of the breast in many studies with some interesting findings [13–15, 28, 29], the potential influence of the TWIST method on the pharmacokinetic parameters is unclear. It is known that sharing k-space data from different time points of dynamic contrast enhancement will affect the measured signal intensity [30, 31]. A simulation study performed by Le Y et al. showed that in tumours larger than 5 mm in diameter, with A = 20 %, the same A value as used in the current study, the underestimation of signal enhancement due to TWIST k-space data sharing is 7.56 % or less [28]. Such an error is unlikely to cause an error in the enhancement curve classification. However, further study is needed to confirm whether this conclusion is also applicable to the pharmacokinetic model. Second, the four-channel coil used in this study limited the effectiveness of the CAIPIRINHA technique, since the performance of a parallel acquisition method is highly related to the number of coil channels [32].
There were also several methodological limitations. First, the sample size (55 lesions) may not have been enough to reveal differences that exist among the parameters or AUCs with varying imaging durations. Moreover, the selected imaging duration needs to be extended to more patients to test its efficiency. These two points will be explored in future research. Considering the purpose of this study, it is important to avoid any calculation inaccuracy caused by measuring procedures. When a lesion is smaller than 1 cm, the ROI position is highly variable and a fluctuating time–signal curve is frequently observed. The cut-off in lesion size of 1 cm may have helped exclude this inaccuracy although it risked introducing some bias into this study. On the other hand, the diagnostic accuracy of pharmacokinetic parameters for lesions smaller than 1 cm is still controversial [18, 33]. But these previous studies were performed using conventional techniques. The coarse spatial resolution and the partial volume effect might be the reasons for the disagreements. With its improved spatial resolution, the CDT-VIBE technique could be a promising solution to this issue.
The quantitative parameters are influenced by multiple factors, and this clinical study can only provide a guide for protocol setup for quantitative DCE-MRI of the breast under the current conditions, including the two-compartment Tofts model, high temporal resolution acquisition, a population average arterial input function and small-sized contrast agent. The results of this study may not be consistent in a different scenario. Despite all these limitations, CDT-VIBE provides a novel tool to achieve real high temporal and spatial resolution imaging for DCE-MRI of the breast. Nevertheless, in the current study, dynamic data could be consecutively and frequently collected with high spatial resolution, enabling the determination of the influence of imaging duration on parameter estimation and diagnostic performance. These preliminary findings provide a solid base for further exploration and clinical application.
In conclusion, the scan duration of breast DCE-MRI has a significant impact on pharmacokinetic parameter estimation. The impact on benign lesions is prominent within the first 2 min after contrast medium injection, but in malignant lesions the impact extends to 4 – 6 min because of the delayed wash-out of contrast medium. However, the discrimination ability of parameters may not be significantly influenced by the scan duration. Since imaging beyond 5 min does not add any improvement, an imaging time of 5 min may be sufficient for calculation of pharmacokinetic parameters of the Tofts model, but the potential to improve the diagnostic value of Ktrans with a shorter scan duration needs further discussion and confirmation.
References
Moon M, Cornfeld D, Weinreb J (2009) Dynamic contrast-enhanced breast MR imaging. Magn Reson Imaging Clin N Am 17:351–362
Barrett T, Brechbiel M, Bernardo M, Choyke PL (2007) MRI of tumor angiogenesis. J Magn Reson Imaging 26:235–249
Huang W, Tudorica LA, Li X et al (2011) Discrimination of benign and malignant breast lesions by using shutter-speed dynamic contrast-enhanced MR imaging. Radiology 261:394–403
Schabel MC, Morrell GR, Oh KY, Walczak CA, Barlow RB, Neumayer LA (2010) Pharmacokinetic mapping for lesion classification in dynamic breast MRI. J Magn Reson Imaging 31:1371–1378
Eyal E, Badikhi D, Furman-Haran E, Kelcz F, Kirshenbaum KJ, Degani H (2009) Principal component analysis of breast DCE-MRI adjusted with a model-based method. J Magn Reson Imaging 30:989–998
Vincensini D, Dedieu V, Eliat PA et al (2007) Magnetic resonance imaging measurements of vascular permeability and extracellular volume fraction of breast tumors by dynamic Gd-DTPA-enhanced relaxometry. Magn Reson Imaging 25:293–302
Ah-See MW, Makris A, Taylor NJ et al (2008) Early changes in functional dynamic magnetic resonance imaging predict for pathologic response to neoadjuvant chemotherapy in primary breast cancer. Clin Cancer Res 14:6580–6589
Yankeelov TE, Lepage M, Chakravarthy A et al (2007) Integration of quantitative DCE-MRI and ADC mapping to monitor treatment response in human breast cancer: initial results. Magn Reson Imaging 25:1–13
Yu Y, Jiang Q, Miao Y et al (2010) Quantitative analysis of clinical dynamic contrast-enhanced MR imaging for evaluating treatment response in human breast cancer. Radiology 257:47–55
Michaely HJ, Morelli JN, Budjan J et al (2013) CAIPIRINHA-Dixon-TWIST (CDT)-volume-interpolated breath-hold examination (VIBE): a new technique for fast time-resolved dynamic 3-dimensional imaging of the abdomen with high spatial resolution. Invest Radiol 48:590–597
American College of Radiology (2014) ACR practice parameter for the performance of contrast-enhanced magnetic resonance imaging (MRI) of the breast. American College of Radiology, Reston, VA. Available via http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/MRI_Breast.pdf. Accessed 25 Sep 2014
Song T, Laine AF, Chen Q et al (2009) Optimal k-space sampling for dynamic contrast-enhanced MRI with an application to MR renography. Magn Reson Med 61:1242–1248
Mann RM, Mus RD, van Zelst J, Geppert C, Karssemeijer N, Platel B (2014) A novel approach to contrast-enhanced breast magnetic resonance imaging for screening: high-resolution ultrafast dynamic imaging. Invest Radiol 49:579–585
Tudorica LA, Oh KY, Roy N et al (2012) A feasible high spatiotemporal resolution breast DCE-MRI protocol for clinical settings. Magn Reson Imaging 30:1257–1267
Herrmann KH, Baltzer PA, Dietzel M et al (2011) Resolving arterial phase and temporal enhancement characteristics in DCE MRM at high spatial resolution with TWIST acquisition. J Magn Reson Imaging 34:973–982
Aerts HJ, Jaspers K, Backes WH (2011) The precision of pharmacokinetic parameters in dynamic contrast-enhanced magnetic resonance imaging: the effect of sampling frequency and duration. Phys Med Biol 56:5665–5678
Jaspers K, Aerts HJ, Leiner T et al (2009) Reliability of pharmacokinetic parameters: small vs. medium-sized contrast agents. Magn Reson Med 62:779–787
Jena A, Mehta SB, Taneja S (2013) Optimizing MRI scan time in the computation of pharmacokinetic parameters (K(trans) ) in breast cancer diagnosis. J Magn Reson Imaging 38:573–579
Ellinger R, Kremser C, Schocke MF et al (2000) The impact of peak saturation of the arterial input function on quantitative evaluation of dynamic susceptibility contrast-enhanced MR studies. J Comput Assist Tomogr 24:942–948
Pedevilla M, Stollberger R, Wach P, Ebner F (1998) Influence of capillary blood flow and first pass effects on determination of tissue permeability. Proceedings of the Sixth Scientific Meeting and Exhibition of the International Society of Magnetic Resonance in Medicine, Sydney. p 1651
Parker GJ, Buckley DL (2005) Tracer kinetic modeling for T1-weighted DCE-MRI. In: Jackson A, Buckley DL, Parker GJ (eds) Dynamic contrast-enhanced magnetic resonance imaging in oncology. Springer, Berlin, pp 81–92
Tofts PS (1997) Modeling tracer kinetics in dynamic Gd-DTPA MR imaging. J Magn Reson Imaging 7:91–101
Kuhl CK, Mielcareck P, Klaschik S et al (1999) Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology 211:101–110
Veltman J, Stoutjesdijk M, Mann R et al (2008) Contrast-enhanced magnetic resonance imaging of the breast: the value of pharmacokinetic parameters derived from fast dynamic imaging during initial enhancement in classifying lesions. Eur Radiol 18:1123–1133
El Khouli RH, Macura KJ, Kamel IR, Jacobs MA, Bluemke DA (2011) 3-T dynamic contrast-enhanced MRI of the breast: pharmacokinetic parameters versus conventional kinetic curve analysis. AJR Am J Roentgenol 197:1498–1505
Stoutjesdijk MJ, Zijp M, Boetes C, Karssemeijer N, Barentsz JO, Huisman H (2012) Computer aided analysis of breast MRI enhancement kinetics using mean shift clustering and multifeature iterative region of interest selection. J Magn Reson Imaging 36:1104–1112
Garcia EM, Storm ES, Atkinson L, Kenny E, Mitchell LS (2013) Current breast imaging modalities, advances, and impact on breast care. Obstet Gynecol Clin N Am 40:429–457
Le Y, Kipfer H, Majidi S et al (2013) Application of time-resolved angiography with stochastic trajectories (TWIST)-Dixon in dynamic contrast-enhanced (DCE) breast MRI. Magn Reson Imaging 38:1033–1042
Le Y, Kroeker R, Kipfer HD, Lin C (2012) Development and evaluation of TWIST Dixon for dynamic contrast-enhanced (DCE) MRI with improved acquisition efficiency and fat suppression. Magn Reson Imaging 36:483–491
Krishnan S, Chenevert TL (2004) Spatio-temporal bandwidth-based acquisition for dynamic contrast-enhanced magnetic resonance imaging. J Magn Reson Imaging 20:129–137
Oesterle C, Strohschein R, Kohler M, Schnell M, Hennig J (2000) Benefits and pitfalls of keyhole imaging, especially in first-pass perfusion studies. J Magn Reson Imaging 11:312–323
Deshmane A, Gulani V, Griswold MA, Seiberlich N (2012) Parallel MR imaging. J Magn Reson Imaging 36:55–72
Gibbs P, Liney GP, Lowry M, Kneeshaw PJ, Turnbull LW (2004) Differentiation of benign and malignant sub-1 cm breast lesions using dynamic contrast enhanced MRI. Breast 13:115–121
Acknowledgements
The scientific guarantor of this study is Guangbin Wang. The authors declare relationships with Siemens Healthcare. Hui Liu is a collaboration scientist with Siemens Healthcare and is responsible for sequence optimization.This study received funding from the National Natural Science Foundation of China (81371525). No complex statistical methods were necessary for this study. Institutional review board approval was obtained, Written informed consent was obtained from all subjects (patients) in this study.
Methodology: prospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hao, W., Zhao, B., Wang, G. et al. Influence of scan duration on the estimation of pharmacokinetic parameters for breast lesions: a study based on CAIPIRINHA-Dixon-TWIST-VIBE technique. Eur Radiol 25, 1162–1171 (2015). https://doi.org/10.1007/s00330-014-3451-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3451-z