Abstract
Objectives
To evaluate mutidetector computed tomography (MDCT) for the prediction of perforation site according to each gastrointestinal (GI) tract site and elapsed time.
Methods
One hundred and sixty-eight patients who underwent MDCT before laparotomy for GI tract perforation were enrolled and allocated to an early or late lapse group based on an elapsed time of 7 h. Two reviewers independently evaluated the perforation site and assessed the following CT findings: free air location, mottled extraluminal air bubbles, focal bowel wall discontinuity, segmental bowel wall thickening, perivisceral fat stranding and localised fluid collection.
Results
The overall diagnostic accuracy was 91.07 % and 91.67 % for reviewers 1 and 2, respectively, with excellent agreement (kappa 0.86). Accuracies (98.97 % and 97.94 %) and agreements (kappa 0.894) for stomach and duodenum perforation were higher than for other perforation sites. Strong predictors of perforation at each site were: focal bowel wall discontinuity for stomach, duodenal bulb and left colon, mottled extraluminal air bubbles for retroperitoneal duodenum and right colon, and segmental bowel wall thickening for small bowel. The diagnostic accuracy was not different between the early- and late-lapse groups.
Conclusions
MDCT can accurately predict upper GI tract perforation with high reliability. Elapsed time did not affect the accuracy of perforation site prediction.
Key Points
• Perforation of the stomach and duodenum can be accurately predicted with MDCT.
• Knowledge of CT findings predicting perforation site can improve diagnostic accuracy.
• Elapsed time does not significantly affect accuracy in predicting perforation sites.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastrointestinal (GI) tract perforation is an emergent condition with a variety of aetiologies, including ulcer disease, inflammation, neoplasms, trauma and iatrogenic factors [1, 2]. Patients with GI tract perforation usually require timely surgical treatment. Laparoscopic surgery is currently performed as a less invasive alternative to open surgery for GI tract perforation [3, 4]. Consequently, establishing the perforation site may be beneficial for the surgeon.
Multidetector computed tomography (MDCT) is now widely available and is well accepted as a useful modality for identifying the presence, site and cause of GI tract perforation [5–9]. Multiplanar reformations of MDCT are also helpful for identifying perforation site by direct visualisation of a bowel wall discontinuity [10]. However, all GI tract perforation on CT cannot be recognised as bowel wall discontinuity and, in some cases, the CT findings predicting the perforation site may be subtle or only indirectly related to the perforation site. Because the GI tract is long and has various relationships with surrounding supporting structures depending on location within the GI tract, CT findings predicting GI tract perforation may be different depending on the GI tract site involved [7].
Although several researchers have addressed the accuracy of MDCT in predicting the site of GI tract perforation and suggestive CT findings according to perforation site [5–9], to the best of our knowledge, no study has been performed on the accuracy and interobserver agreement in predicting perforation site by MDCT according to each GI tract site. In addition, the CT findings that are most predictive of each GI tract perforation site have not been studied. If MDCT confidently offers an accurate detection rate for perforation according to the each GI tract site, it may be helpful for surgeons in determining therapeutic options.
We also hypothesised that the time elapsed between bowel perforation and CT may affect the accuracy of perforation site prediction, because intra-abdominal reactions after bowel perforation may actively change over time. Although a few studies have discussed CT findings in relation to the elapsed time since bowel perforation [11–13], there have not been any reports on the accuracy of predicting the site of bowel perforation according to elapsed time.
We undertook this study to evaluate the accuracy and interobserver agreement of MDCT in predicting perforation site according to the each GI tract site. We also examined the most predictive CT findings and the effects of the time elapsed since clinical suspicion of perforation.
Material and methods
Study population and medical records
The institutional review board of our hospital approved this retrospective study and waived the requirement for informed consent. From January 2007 to October 2012, 241 consecutive adult patients (>18 years) underwent surgery for GI tract perforation other than appendiceal perforation at our hospital. From a total of 241 patients, we excluded 66 patients who underwent CT examination at an outside hospital due to concerns regarding inhomogeneous CT techniques. Thus, a total of 175 patients met this criterion and all of these patients underwent surgery within 12 hours after CT. Among this population, we excluded seven patients who did not have complete medical records, and the remaining 168 patients were enrolled in this study. The mean age of the patients was 56.9 years (range, 19–90 years). There were 119 male and 49 female patients.
Based on medical records, we estimated the time elapsed between CT and abdominal trauma or between CT and the onset of acute non-traumatic severe abdominal pain. The mean elapsed time was 18 h (range, 1–120 h). We divided the patients into an early lapse group (n = 85) and a late lapse group (n = 83) with a cut-off of 7 h, which was set by the cumulative frequency percentage point of 50 %.
Based on the surgery, we categorised the GI tract perforation sites as follows: stomach including the duodenal bulb (n = 91), retroperitoneal duodenum (n = 6), small bowel (n = 39), right colon (n = 9) consisting of the cecum, ascending colon, hepatic flexure and transverse colon, and left colon (n = 23) consisting of the splenic flexure, descending colon, sigmoid colon and rectum. The causes of each GI tract perforation are listed in Table 1.
Imaging techniques
All CT images were obtained using a 16- or 64-slice MDCT scanner (Brilliance 16 and 64; Philips Medical Systems, Cleveland, OH). CT was performed in the craniocaudal direction from the level above the diaphragm to the pubic symphysis. None of the patients received oral contrast. For the 16-slice MDCT, CT parameters were as follows: collimation 1.5 mm, pitch 1.188 and rotation time 0.75 s. For the 64-slice MDCT the parameters were: collimation 0.625 mm, pitch 1.014 and rotation time 0.5 s. Tube voltage was 120 kVp and tube current was 150–300 mA in both scanners. Contrast-enhanced CT of the entire abdomen was performed with a 70 s delay after the injection of 120 ml iomeprol (Iomeron 350; Bracco, Milan, Italy) or iohexol (Iobrix 350; Taejoon Pharmaceutical, Kyungkido, South Korea) at a rate of 4 ml/s through an antecubital vein. The axial section data were reconstructed at a thickness of 5 mm with 5-mm increments and at a thickness of 2 mm with 1-mm increments. The second set of reconstructed axial scans was then reformatted in the coronal plane at a thickness of 3 mm with 3-mm increments.
Image analysis
Two radiologists with 8 (S.W.K., reviewer 1) and 14 years (S.J.P., reviewer 2) of dedicated abdominal imaging experience independently evaluated CT images to detect the site of GI tract perforation. These two reviewers were aware that all CT images involved surgical patients with GI tract perforation, but did not have access to surgical or pathological records. Images were presented to the reviewers in a random sequence using a PACS system (Piview Star; Infinitt Healthcare, Seoul, Korea) in stack mode. The two reviewers evaluated both axial reconstructions and coronally reformatted images and they independently recorded the location of the perforation site along the GI tract as follows: stomach including duodenal bulb, retroperitoneal duodenum, small bowel, right colon and left colon.
In each case, the two reviewers also assessed strong predictors for each perforation site among the following six useful CT findings: free air location, mottled extraluminal air bubbles, focal bowel wall discontinuity, segmental bowel wall thickening, perivisceral fat stranding and localised fluid collection. Free air location can be localised as free air only around the liver and stomach, which may be more suggestive of gastroduodenal perforation, or free air only in the pelvis, which may be more suggestive of colon perforation or, less frequently, of small bowel perforation [9, 11, 14, 15]. Based on these definitions, the reviewers subjectively used the free air location for predicting perforation site. Mottled extraluminal air bubbles were defined as concentrated small air collections in close proximity to the bowel wall. Focal bowel wall discontinuity was defined as interruption of the enhancing bowel wall as depicted by a low-attenuation area, such as fluid, air or faeces. Segmental bowel wall thickening was defined as wall thickness greater than 3 mm. The reviewers subjectively assigned each contribution score of six useful CT findings for predicting the perforation sites (0, no contribution; 1, partial contribution; 2, definite contribution). Reviewers were requested to assign at least one or two definite contribution in each case.
Statistical analyses
The diagnostic accuracy of the MDCT in the prediction of perforation site for both reviewers was evaluated by comparing the MDCT results to the surgical results. Agreement between the two reviewers in predicting the perforation site regardless of accuracy was determined using the kappa statistic. We also calculated the diagnostic accuracy and interobserver agreement for predicting the perforation sites according to the each GI tract site. A kappa value of 0.0–0.19 indicated poor agreement; 0.2–0.39, fair agreement; 0.4–0.59, moderate agreement; 0.6–0.79, good agreement; 0.8–1.0, excellent agreement. For the accurately predicted cases, we calculated the mean contribution scores (range, 0–2) of each CT finding for predicting the perforation site in each part of the GI tract. We subjectively defined a mean contribution score more than 1 as a useful finding for predicting the perforation site.
We divided the study population into the upper GI tract perforation group (n = 97), including the stomach and duodenum, and a lower GI tract perforation group (n = 71), including the small bowel and colon [6, 14]. The diagnostic accuracy and interobserver agreement for the MDCT between the early lapse group and late lapse group and between the upper and lower GI tract groups were also evaluated by comparing the MDCT results to the surgical results.
Statistical significance was accepted for P values of <0.05. Statistical analysis was performed using MedCalc version 12.3.0 (MedCalc Software, Mariakerke, Belgium).
Results
Accuracy and agreement for the prediction of perforation at each GI tract site
The accuracy for predicting the GI tract perforation site was 91.07 % (153 of 168) for reviewer 1 (8 years of abdominal imaging experience) and 91.67 % (154 of 168) for reviewer 2 (14 years of abdominal imaging experience). There was no significant difference in accuracy between the reviewers. The overall agreement between reviewers in predicting the site of perforation was excellent (kappa value = 0.861). Accuracy and agreement for both reviewers according to each GI tract site are listed in Table 2. Stomach perforation, including the duodenal bulb, was nearly perfectly predicted by both reviewers. The agreement for this perforation site was good (kappa value = 0.797). Perforations of the retroperitoneal duodenum were perfectly predicted by both reviewers. However, the accuracy for predicting small bowel and colon perforation was less than 90 %. In addition, the agreement for prediction of these perforation sites was poor and fair for the small bowel and colon, respectively. Reviewer 1 and 2 incorrectly predicted the perforation site in 15 patients and 14 patients for each site, respectively. Cases of incorrect site prediction by each reviewer according to GI tract site are listed in Table 3.
MDCT findings for predicting perforation site according to each GI tract site
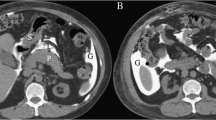
The mean contribution score of each CT finding for predicting perforation site according to each site along the GI tract is summarised for both reviewers in Table 4. In stomach including duodenal bulb perforation, focal bowel wall discontinuity (Fig. 1) was a useful CT predictor for both reviewers. Segmental bowel wall thickening was also regarded as a useful predictor for reviewer 1. Mottled extraluminal air bubbles (Fig. 2), focal bowel wall discontinuity and localised fluid collections were useful predictors for retroperitoneal duodenal perforation for both reviewers. In small bowel perforation, segmental bowel wall thickening (Fig. 3) was a useful predictor for both reviewers, and perivisceral fat stranding (Fig. 4) was useful for reviewer 1. In right colon perforation, mottled extraluminal air bubbles, segmental bowel wall thickening and perivisceral fat stranding were useful predictors for reviewer 1 and mottled extraluminal air bubbles were useful for reviewer 2. Focal bowel wall discontinuity was a useful predictor of left colon perforation for both reviewers (Fig. 5) and perivisceral fat stranding was useful for reviewer 1.
Coronal contrast-enhanced reformatted CT image of a 53-year-old man with abdominal pain for 4 h shows a focal discontinuity (arrow) at the thickened wall of duodenal bulb. Note the free air entrapped in the intrahepatic fissure. The patient underwent laparoscopic surgery, which confirmed duodenal bulb perforation
Axial contrast-enhanced CT image of a 64-year-old man who had obtained a CT 27 h after blunt abdominal trauma shows mottled extraluminal air bubbles (arrows) in close proximity to the retroperitoneal duodenum (open arrows). Note the fluid collection in right retroperitoneum. The patient underwent operation, which confirmed perforation of the third portion of duodenum
Axial contrast-enhanced CT image of a 32-year-old man who had obtained a CT 36 h after blunt abdominal trauma shows a thick, enhancing wall (arrows) of a jejunal loop and adjacent extraluminal air (open arrows). Note the large amount of free air. The patient underwent operation, which confirmed perforation of the jejunum
Axial contrast-enhanced CT images of a 56-year-old man who had been experiencing abdominal pain for 15 h show (a) perienteric fat stranding (arrows) with mottled air bubbles (open arrows) in the right mesentery and greater omentum, and (b) a focal wall defect with air trapping (arrowhead) in the fluid filling structure suggesting Meckel’s diverticulum (m). This patient underwent operation, which confirmed perforation of a Meckel’s diverticulum in the ileum
Accuracy and agreement for the prediction of perforation site between the upper and lower GI tract and according to elapsed time
The diagnostic accuracy and interobserver agreement for predicting perforation site between the upper and lower GI tract and according to elapsed time are summarised in Table 5. The accuracy of upper GI tract perforation prediction for both reviewers (98.97 % and 97.94 % for reviewer 1 and 2, respectively) was significantly higher than that for lower GI tract perforation (80.28 % and 83.10 % for reviewer 1 and 2, respectively) (P < 0.01). There was no significant difference in diagnostic accuracy between the early and late lapse groups according to perforation site (P = 0.622 and 0.745 for reviewer 1 and 2, respectively). The accuracy of upper GI tract perforation in the early lapse group was significantly higher than that of lower GI tract perforation for both reviewers (P < 0.01), whereas accuracy in the late lapse group was not significantly different between the upper and lower GI tract for either reviewer.
Inter-reviewer agreement was significantly higher in upper GI tract perforation (kappa value = 0.894) than in lower GI tract perforation (kappa value = 0.595) (P < 0.001). In terms of elapsed time, agreement was significantly higher in the late lapse group (kappa value = 0.925) than in the early lapse group (kappa value = 0.779) (P < 0.001). Inter-reviewer agreement was significantly higher in the early lapse group than in the late lapse group in upper GI tract perforation, whereas it was significantly higher in the late lapse group than in the early lapse group in cases of lower GI tract perforation. In the late lapse group, agreement in upper GI tract perforation was not significantly different from lower GI tract perforation.
Discussion
Our results show that both reviewers successfully predicted GI tract perforation site by viewing MDCT images for more than 90 % of the patients in this study. This result was similar to previous reports [5, 8]. Among the perforation sites, both reviewers more accurately predicted perforation of the upper GI tract, consisting of the stomach and duodenum, than perforation of the lower GI tract. Thus, we suggest that preoperative MDCT can be interpreted confidently in cases of upper GI tract perforation. Furthermore, MDCT may affect the selection of treatment options, such as laparoscopic approach. The laparoscopic repair of a perforated peptic ulcer has been regarded as a safe and reliable procedure [3, 16, 17]. The laparoscopic approach is also gradually gaining acceptance in the treatment of colon and small bowel perforation [4, 18]. In our study, small bowel perforation was accurately predicted in more than 87 % of cases, which may enable surgeons to initially try a laparoscopic approach in patients with an MDCT suggesting small bowel perforation. Less than 75 % of cases of colon perforation were accurately predicted by MDCT, suggesting that surgeons may want to hesitate before accepting a laparoscopic approach in these patients. Instead, the surgeon may wish to consider conventional laparotomy in patients with colon perforation when CT findings indicating the colon perforation are not definitely detected.
In this study, overall agreement between the reviewers for predicting the site of perforation was excellent (kappa value = 0.861). Although this agreement is slightly lower than that of a previous study (kappa value = 0.937) [5], our study may be more reliable because of our larger study population of 168 patients compared to only 49 patients in the previous study. In addition, we evaluated interobserver agreement at each perforation site along the GI tract. Similar to the results for diagnostic accuracy, interobserver agreement was much higher for the prediction of upper GI tract perforation than for lower GI tract perforation. This might be because the upper GI tract is shorter and relatively fixed compared with the lower GI tract, which may make it easier to predict the perforation site, once the CT findings indicating the bowel perforation were identified. In addition, the lower GI tract is more coiled and movable than the upper GI tract, which can make perforation site prediction by CT more difficult. Although the agreement may not correspond exactly to diagnostic accuracy, we believe it is meaningful that reader agreement is reliable in predicting perforation site.
In this study, although there was a difference of 6 years of experience between the two reviewers, there was no significant difference in the accuracy of detection of the site of GI tract perforation between them. The retrospective nature of this study and the use of coronal reformatted images may have affected the performance of the less experienced reviewer in comparison to the more experienced reviewer. Ghekiere et al. [10] reported that adding reformatted images can increase the diagnostic accuracy of a junior reviewer and also increase the agreement between reviewers in the identification of possible perforation sites.
The CT findings in cases of GI tract perforation are well known and can be separated into direct and indirect findings [5–9]. Direct findings are focal bowel wall discontinuity and the presence of extraluminal air [7]. Focal bowel wall discontinuity is undoubtedly the most accurate finding indicating the site of bowel perforation. The use of MDCT with multiplanar reformation images can be helpful for identification of bowel wall discontinuity when the axial CT images are indeterminate. In our study, focal bowel wall discontinuity was a useful predictor of gastro-duodenum and left colon perforation. Similar to our study, Oguro et al. [6] reported that the accuracy of focal bowel wall discontinuity in the detection of upper GI tract perforation is significantly higher than the accuracy in lower GI tract perforation. However, focal bowel wall discontinuity is not helpful for detecting small bowel and right colon perforation.
Mottled extraluminal air bubbles in close proximity to the bowel wall may be helpful in prediction the site of perforation when there are few air bubbles [7, 9]. In our study, mottled extraluminal air bubbles were a useful predictor for identification of retroperitoneal duodenum and right colon perforation. Although we thought that mottled extraluminal air bubbles may be also a useful predictor of stomach including duodenal bulb perforation, it did not appear to be a useful finding for this site because focal bowel wall discontinuity was already a strong predictor. Certain free air locations, such as periportal free air, free air around the falciform ligament and free air trapped in the fissure of the ligamentum teres, have been reported as useful predictors that can help to differentiate upper GI from lower GI tract perforation [14]. Conversely, free air only located in the pelvis may suggest colon perforation [9]. Choi et al. [11] reported that free air locations around the liver was less accurate than other strong predictors in the detection of upper GI tract perforation and should rather be regarded as a complementary predictor. As in our study, free air locations had a less significant role in predicting upper GI tract perforation. However, the mean contribution scores (0.856 and 0.809 for reviewers 1 and 2, respectively) for the predictions of stomach including duodenal bulb perforation were higher than that of other GI tract sites perforations. Thus, certain free air locations can be useful findings in the presence of other strong predictors of GI tract perforation.
When focal bowel wall discontinuity cannot be demonstrated by CT, segmental bowel wall thickening, perivisceral fat stranding and a localised fluid collection on CT can be also facilitate the prediction of the site of perforation [1, 19]. In our study, segmental bowel wall thickening and perivisceral fat stranding were regarded as useful findings for predicting small bowel perforation. Perivisceral fat stranding was also regarded as a useful finding for predicting colon perforation.
Previous studies reported that with an increase in the elapsed time, there was an increase in the amount of extraluminal air [11–13]. We presumed that intra-abdominal changes after bowel perforation might develop rapidly over time. Thus, we questioned whether the time from bowel perforation to CT might affect the prediction of perforation site. In our study, the elapsed time did not significantly affect accuracy in predicting perforation site. This might be due to the relatively short cut-off point of 7 h. Elapsed time might also only influence the amount and movement of extraluminal air, which may be less of a strong predictor of perforation site than focal bowel wall discontinuity. However, interobserver agreement was significantly higher in the late lapse group than in the early lapse group, especially in lower GI tract perforation. This might be because, as elapsed time increases, some CT findings (e.g. mottled extraluminal air bubbles, segmental bowel wall thickening, or perivisceral fat stranding) predicting perforation site may be more clearly identified in cases of lower GI tract perforation.
In this study, we did not administer oral or rectal contrast material for CT imaging. Several articles have recommended oral or rectal contrast material administration before CT because extraluminal leakage of contrast material can be a specific CT sign for GI tract perforation [19–21]. However, the reported sensitivity of extraluminal leakage of contrast material varies from 19–42 % [22]. Oral contrast material administration may delay CT examination by the slow progression of material in patients suffering from paralytic ileus [7]. In addition, it is often difficult to obtain oral or rectal opacification in a patient with acute abdominal pain. Thus, our institution performs CT without oral or rectal contrast material due to the typically emergent nature of cases with suspected GI tract perforation.
Some limitations of our study require consideration. First of all, the study was inherently limited by its retrospective design. Our cohort consisted of patients who were already confirmed to have GI tract perforation by surgery. The retrospective nature of the study may have increased accuracy in the prediction of perforation site compared with common practical situations. Second, the number of patients with stomach including duodenal bulb perforation was much more than that of the patients with retroperitoneal duodenum and right colon perforation, which may have influenced the assessment of the diagnostic accuracy according to the each GI tract site. However, in previous studies, the study populations for stomach and duodenal perforation were larger than for other perforation sites [6, 8, 9, 11, 14]. Third, we subjectively defined elapsed time as the time from the onset of acute severe abdominal pain in non-traumatic patients to the time of CT. Although patients with perforation typically complain of severe abdominal pain [23], it was difficult to predict the exact perforation time by clinical symptoms alone.
In summary, upper GI tract perforation can be predicted with high accuracy and reliability through MDCT evaluation. Although interobserver agreement for predicting the perforation site increased with increasing elapsed time, elapsed time did not influence diagnostic accuracy. Familiarity with CT findings predictive of the site of GI tract perforation could provide improved accuracy in perforation site determination.
Abbreviations
- GI:
-
Gastrointestinal
References
Maniatis V, Chryssikopoulos H, Roussakis A et al (2000) Perforation of the alimentary tract: evaluation with computed tomography. Abdom Imaging 25:373–379
Singh JP, Steward MJ, Booth TC, Mukhtar H, Murray D (2010) Evolution of imaging for abdominal perforation. Ann R Coll Surg Engl 92:182–188
Bertleff MJ, Halm JA, Bemelman WA et al (2009) Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg 33:1368–1373
Hansen AJ, Tessier DJ, Anderson ML, Schlinkert RT (2007) Laparoscopic repair of colonoscopic perforations: indications and guidelines. J Gastrointest Surg 11:655–659
Kim JW, Shin SS, Heo SH, Jeong YY, Kang HK (2011) The accuracy of 64-slice MDCT for determining the perforation site of the gastrointestinal tract: ROC analysis. Abdom Imaging 36:503–508
Oguro S, Funabiki T, Hosoda K et al (2010) 64-slice multidetector computed tomography evaluation of gastrointestinal tract perforation site: detectability of direct findings in upper and lower GI tract. Eur Radiol 20:1396–1403
Kim SH, Shin SS, Jeong YY, Heo SH, Kim JW, Kang HK (2009) Gastrointestinal tract perforation: MDCT findings according to the perforation sites. Korean J Radiol 10:63–70
Imuta M, Awai K, Nakayama Y et al (2007) Multidetector CT findings suggesting a perforation site in the gastrointestinal tract: analysis in surgically confirmed 155 patients. Radiat Med 25:113–118
Hainaux B, Agneessens E, Bertinotti R et al (2006) Accuracy of MDCT in predicting site of gastrointestinal tract perforation. AJR Am J Roentgenol 187:1179–1183
Ghekiere O, Lesnik A, Millet I, Hoa D, Guillon F, Taourel P (2007) Direct visualization of perforation sites in patients with a non-traumatic free pneumoperitoneum: added diagnostic value of thin transverse slices and coronal and sagittal reformations for multi-detector CT. Eur Radiol 17:2302–2309
Choi AL, Jang KM, Kim MJ et al (2011) What determines the periportal free air, and ligamentum teres and falciform ligament signs on CT: can these specific air distributions be valuable predictors of gastroduodenal perforation? Eur J Radiol 77:319–324
Kim HC, Shin HC, Park SJ et al (2004) Traumatic bowel perforation: analysis of CT findings according to the perforation site and the elapsed time since accident. Clin Imaging 28:334–339
Saku M, Yoshimitsu K, Murakami J et al (2006) Small bowel perforation resulting from blunt abdominal trauma: interval change of radiological characteristics. Radiat Med 24:358–364
Cho HS, Yoon SE, Park SH, Kim H, Lee YH, Yoon KH (2009) Distinction between upper and lower gastrointestinal perforation: usefulness of the periportal free air sign on computed tomography. Eur J Radiol 69:108–113
Stoker J, van Randen A, Laméris W, Boermeester MA (2009) Imaging patients with acute abdominal pain. Radiology 253:31–46
Siu WT, Leong HT, Law BK et al (2002) Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg 235:313–319
Druart ML, Van Hee R, Etienne J et al (1997) Laparoscopic repair of perforated duodenal ulcer. A prospective multicenter clinical trial. Surg Endosc 11:1017–1020
Addeo P, Calabrese DP (2011) Diagnostic and therapeutic value of laparoscopy for small bowel blunt injuries: a case report. Int J Surg Case Rep 2:316–318
Furukawa A, Sakoda M, Yamasaki M et al (2005) Gastrointestinal tract perforation: CT diagnosis of presence, site, and cause. Abdom Imaging 30:524–534
Zissin R, Osadchy A, Gayer G (2009) Abdominal CT findings in small bowel perforation. Br J Radiol 82:162–171
Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Scalea TM (2001) Triple-contrast helical CT in penetrating torso trauma: a prospective study to determine peritoneal violation and the need for laparotomy. AJR Am J Roentgenol 177:1247–1256
Becker CD, Mentha G, Schmidlin F, Terrier F (1998) Blunt abdominal trauma in adults: role of CT in the diagnosis and management of visceral injuries. Part 2: gastrointestinal tract and retroperitoneal organs. Eur Radiol 8:772–780
Mahvi DM, Krantz SB (2012) Stomach. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL (eds) Sabiston textbook of surgery: the biological basis of modern surgical practice, 19th edn. Saunders Elsevier, Philadelphia, pp 1182–1226
Acknowledgements
The scientific guarantor of this publication is Wook Jin, M.D. PhD at the Kyung Hee University Hospital at Gangdong. This work was supported by a grant from the Kyung Hee University in 2012 (KHU-20120759). Institutional Review Board approval was obtained and written informed consent was waived. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H.C., Yang, D.M., Kim, S.W. et al. Gastrointestinal tract perforation: evaluation of MDCT according to perforation site and elapsed time. Eur Radiol 24, 1386–1393 (2014). https://doi.org/10.1007/s00330-014-3115-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3115-z