Abstract
Objective
To assess diagnostic performance of dual-input CT perfusion for distinguishing malignant from benign solitary pulmonary nodules (SPNs).
Methods
Fifty-six consecutive subjects with SPNs underwent contrast-enhanced 320-row multidetector dynamic volume CT. The dual-input maximum slope CT perfusion analysis was employed to calculate the pulmonary flow (PF), bronchial flow (BF), and perfusion index \( \left( {\mathrm{PI},={{\mathrm{PF}} \left/ {{\left( {\mathrm{PF} + \mathrm{BF}} \right)}} \right.}} \right) \). Differences in perfusion parameters between malignant and benign tumours were assessed with histopathological diagnosis as the gold standard. Diagnostic value of the perfusion parameters was calculated using the receiver-operating characteristic (ROC) curve analysis.
Results
Amongst 56 SPNs, statistically significant differences in all three perfusion parameters were revealed between malignant and benign tumours. The PI demonstrated the biggest difference between malignancy and benignancy: 0.30 ± 0.07 vs. 0.51 ± 0.13 , P < 0.001. The area under the PI ROC curve was 0.92, the largest of the three perfusion parameters, producing a sensitivity of 0.95, specificity of 0.83, positive likelihood ratio (+LR) of 5.59, and negative likelihood ratio (−LR) of 0.06 in identifying malignancy.
Conclusions
The PI derived from the dual-input maximum slope CT perfusion analysis is a valuable biomarker for identifying malignancy in SPNs. PI may be potentially useful for lung cancer treatment planning and forecasting the therapeutic effect of radiotherapy treatment.
Key Points
• Modern CT equipment offers assessment of vascular parameters of solitary pulmonary nodules (SPNs)
• Dual vascular supply was investigated to differentiate malignant from benign SPNs.
• Different dual vascular supply patterns were found in malignant and benign SPNs.
• The perfusion index is a useful biomarker for differentiate malignancy from benignancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the early 1970s it was discovered through post-mortem microarteriography study that lung tumours have a dual vascular supply, i.e. the pulmonary circulation and the systemic circulation [1]. In vivo quantification of the dual blood supply in lung cancer by CT perfusion is now possible owing to the greater coverage along the z axis provided by the 320-row CT system [2]. Before this, perfusion or blood flow could only be measured within a coverage range limited by the detector width. Thus, the pulmonary artery usually could not be included in the perfusion imaging territory, and in most cases the aorta was selected as the input artery. The single-input maximum slope perfusion model was used to assess the lung tumour haemodynamics. The recent dynamic volume CT mode utilising the 320-row system (with 16-cm coverage in the z axis) makes it possible to include the pulmonary artery, the aorta, and the tumour studied in one gantry rotation without table movement. Then contrast-enhanced dynamic-volume acquisitions will simultaneously capture the pulmonary and systemic circulation input functions as well as the tumour’s first-pass response function. It is then possible to assess the dual blood supply in lung tumours with the dual-input maximum slope analysis model.
Good management of the pulmonary nodules was supposed to reduce lung cancer mortality [3]. Differentiating malignant from benign SPNs when only conventional CT data are available is always a challenge for the radiologist because of the huge overlap in morphological findings between malignancy and benignity. With the development of multi-detector CT systems and the CT perfusion technique, tumour haemodynamics derived from perfusion measurements were used to help identify lung cancer [4, 5]. The single-input maximum slope analysis model was used for this purpose and proved helpful in the differential diagnosis between malignant and benign [6, 7]. Theoretically DI-CTP is more suitable for analysing lung tumour perfusion as it can estimate the pulmonary circulation and the bronchial or systemic circulation as separate perfusion parameters. To our knowledge, the pulmonary and the bronchial circulation (systemic circulation) has never been measured for discrimination between malignant and benign lung tumours. We hypothesise that quantification of the two circulations in SPNs might help to identify lung cancer. This prospective study was designed to determine the diagnostic value of DI-CTP in solitary pulmonary nodules for identifying lung cancer.
Materials and methods
Study population
The prospective study was approved by the institution’s ethics committee. Written informed consent was obtained from all patients, and complete explanation of the study, which included information about radiation exposure during the CT examinations, was given to all patients. Exclusion criteria were respiratory dysfunction and previous reactions to iodinated contrast media. Fifty-six consecutive patients (31 men and 25 women; mean age, 51 years; range, 37–66 years) all with solitary pulmonary nodules were enrolled prospectively in the study. Pathological diagnoses were acquired by CT-guided puncture biopsy or surgical resection or bronchofibroscopic biopsy within 2 weeks before or after the CT perfusion was performed (32 malignant: 11 squamous cell carcinoma, 6 adeno-squamous carcinoma, 11 adeno carcinoma, and 4 small cell lung carcinoma; 24 benign: 7 inflammatory pseudotumour, 8 tuberculoma, 4 hamartoma, 4 global atelectasis, 1 sclerosing angioma). Mean tumour size was 10.7 cm3, ranging from 2.4 cm3 to 44.1 cm3.
The radiation dose of the dynamic CT was calculated from the dose–length product (DLP) listed in the exposure summary sheet generated by the CT equipment and multiplied by a k-factor of 0.014 [8].
CT perfusion imaging technique
Before the examination, all patients underwent breath exercise training to ensure that they could hold their breath for the duration of the entire perfusion procedure (approximately 30 s). Shallow abdominal breathing was permitted at the end stage of acquisition in cases where the patients were unable to hold their breath for the entire period of CT data acquisition. Two 20-gauge intravenous catheters were placed, one in each antecubital vein.
Before perfusion CT, unenhanced helical CT of the entire thorax was performed to determine the location of the SPN. The dynamic volume CT perfusion was performed using 320-row multidetector CT (Aquilion ONE, Toshiba Medical Systems, Otawara, Japan) with z-axis coverage of 16 cm. With a dual-head power injector, 60 ml of non-ionic contrast medium with an iodine concentration of 370 mg I/ml (Iopromide, Bayer Schering, Berlin, Germany) was injected at a flow rate of 8 ml/s (4 ml/s on each side). Two seconds after the start of the bolus injection, 15 intermittent low-dose volume acquisitions were made with 2-s intervals with no table movement.
The dynamic volume CT protocol was performed with the following parameters: 80-kV tube voltage, 80-mA tube current, 0.5-s gantry rotation speed, and 0.5-mm slice thickness. The 16-cm coverage included both the lung hilum and the SPN. The first two volumes were acquired before the contrast medium arrived in the heart and served as a baseline. The duration of the breath hold was approximately 30 s. The data were processed with adaptive iterative dose reduction (AIDR 3D) and automatically reconstructed with 0.5-mm slice thickness and 0.5-mm spacing, resulting in 320 images per volume and a total of 4,800 images for the entire perfusion data set.
Data post-processing and analysis
Post-processing was performed using perfusion software available on the CT equipment (Body Perfusion, dual-input maximum slope analysis, Toshiba Medical Systems, Otawara, Japan). The first step is volume registration. The registration is performed to correct for motion between the dynamic volumes and creates a registered volume series. The registered volumes were then loaded into the body perfusion analysis software.
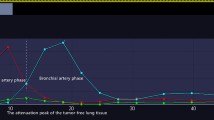
Rectangular ROIs (mean area 1.0 cm2) were manually placed in the pulmonary artery trunk and the aorta at the level of the hilum to generate the TDCs representing the PA input function and the BA input function respectively. An elliptical ROI was placed in the left atrium, and the peak time of the left atrium TDC was used to differentiate pulmonary circulation (before the peak time point) and bronchial circulation (after the peak time point) [2]. A freehand ROI was drawn to encompass the lesion to generate the TDC of the contrast medium’s first-pass attenuation in the SPN. The perfusion analysis range was set from 0 HU to 150 HU to restrict the perfusion analysis to soft tissue regions only and to ignore lung parenchyma and bone. Finally, 512 × 512 matrix colour-coded maps of the PF, BF and PI \( \left( {\mathrm{PI},={{\mathrm{PF}} \left/ {{\left( {\mathrm{PF} + \mathrm{BF}} \right)}} \right.}} \right) \) were generated automatically. For each lesion, measurements were repeated on all relevant 5.0-mm axial slices and then averaged to calculate the final value. Tumour volume (size) was measured on commercial software (organ selection, Vitrea version 6.0, Vital Images, Minnetonka, MN, USA).
Statistical analysis
Statistical analysis was performed using commercially available software (SPSS, V13.0). Student’s t test and the 95 % confidence interval were used to compare perfusion parameters between malignant and benign. ROC analysis was used to calculate and compare the diagnostic values of the three perfusion parameters in identifying lung cancer. A P value lower than 0.05 was considered to indicate a significant difference.
Results
Eleven patients adopted shallow abdominal breathing because of hypoxia at the end stage of the perfusion CT. All patients showed good compliance with the CT perfusion procedure despite the relatively high injection rate of contrast agent and the slightly long breath-hold duration of 30 s. No severe adverse events occurred.
Perfusion parameters were visualised by colour maps and fused onto the original axial CT images. Representative perfusion colour maps are shown in Figs. 1 and 2. Perfusion results of the 56 SPNs derived from DI-CTP are listed in Table 1 and shown in Fig. 3. Of the 56 SPNs, significant differences in all three perfusion parameters were revealed between malignant and benign tumours. The PI demonstrates the greatest difference between malignant and benign: 0.30 ± 0.07 vs. 0.51 ± 0.13 , P < 0.001. The area under the ROC of the PI is 0.92, the largest of the three perfusion parameters, indicating a sensitivity of 0.95, specificity of 0.83, +LR of 5.59, and –LR of 0.06 for identifying lung cancer. The dynamic perfusion protocol was identical for all 56 cases. The CT dose DLP = 324.8 mGy. cm or 4.55 mSv (k = 0.014).
Discussion
In vivo measurement of the two circulations in lung cancer was not technically possible until recently. Bronchial blood flow in lung cancer has been confirmed by many reports from bronchoangiography studies [9]. On the other hand, in vivo evidence of pulmonary circulation in lung cancer was rarely documented, except for a hint from a previous study [10], which reported that some lung cancer tumours enhanced earlier than the enhancement of the aorta, indicating significant blood flow from pulmonary vessels. Theoretically, the single-input maximum slope algorithm calculates blood flow as the ratio of (maximum slope of the tissue TDC)/(maximum HU of the feeding artery). In the case of a double vascular system, such as pulmonary and bronchial circulation in lung tumours, the maximum slope in the tissue’s TDC represents the dominant blood flow; the lower blood flow is thus ignored by single-input analysis. Considering that bronchial or systemic blood flow is relatively higher than the pulmonary blood flow in lung cancer (Figs. 2 and 3), the single-input maximum slope analysis result is just the bronchial flow. Vice versa, the blood flow in benign tumours derived from the single-input maximum slope analysis is the pulmonary blood flow. Insufficient assessment of the lung tumour’s true haemodynamics may be the reason why the diagnostic performance of CT perfusion in lung cancer reported previously [11] is not as good as the figures from this study. In this study, in all cases the blood flow fractions of the two circulations are heterogeneous within the tumour (Fig. 2); regional measurement therefore differs significantly from whole volume assessment. This may be another reason for the difference in the findings between this investigation and previously reported studies, which were performed within one or two transverse CT sections owing to the limited detector width of the device.
In terms of the total blood flow in normal lung tissue, the bronchial blood flow fraction is very low, to the order of 1 % to 2 %. However, the bronchial blood flow is crucial for maintaining airway and lung function [12] and is more transformable under pathological conditions. In lung cancer the BA fraction increases. Findings from this study support a dominant bronchial blood flow with a relatively low fraction of pulmonary blood flow in malignant SPNs (Table 1, Figs. 2 and 3), as demonstrated by the PI = 0.30 ± 0.07 derived from DI-CTP. For benign tumours, nearly balanced perfusion between pulmonary circulation and bronchial circulation was demonstrated with a PI of 0.51 ± 0.13. These findings may not only benefit the differential diagnosis of lung cancer, but also help lung cancer treatment planning: (1) If interventional therapy is a choice for patients with lung cancer, we can make the decision whether transpulmonary artery treatment or transbronchial artery treatment will be performed based on the value of the PI. (2) Because of different oxygen concentrations in pulmonary and systemic blood, the PI does indicate oxygen saturation in the tumour by considering the BA fraction. It has been reported that a high level of oxygenation leads to greater radiosensitivity [13]. The PI is potentially useful for forecasting the therapeutic effect of radiotherapy treatment in lung cancers.
Receiver-operating characteristic curve analysis is used to assess the diagnostic performance of a certain index for a certain disease state, the area under the curve indicating its diagnostic efficiency: the larger the area, the better the diagnostic performance [14]. Among the ROC curves of the three perfusion parameters, the PI has the largest area under its curve, indicating the PI as the best among the three for discriminating between malignant and benign (Fig. 4). To further determine its sensitivity and specificity, a cutoff value point in the curve was determined. Usually this point is defined as having the shortest distance to the left upper corner of the ROC coordinate system. In this study the cutoff value of PI is 0.42, generating sensitivity of 0.95, specificity of 0.83, +LR of 5.59, and –LR of 0.06. The positive and negative predictive values (PPVs and NPVs) of a test in confirming and excluding a diagnosis of cancer in a group of patients depend on the prevalence of cancer in that group. In contrast, the –LR and +LR were regarded as being more stable than PPVs and NPVs in delineating diagnostic efficiency and therefore were chosen in this study [15, 16]. When the +LR has a value >10 and –LR < 0.1, we have great confidence in confirming or ruling out a certain disease. Accordingly, if a case of SPN has a PI value higher than 0.42 the cancer diagnosis can be ruled out with great confidence. However if the PI value is lower than 0.42, the lung cancer diagnosis can be suggested, but without too much confidence owing to a relatively low +LR. Further tests, such as biopsy, should be adopted to confirm the diagnosis.
Receiver-operating characteristic (ROC) curves of the three perfusion parameters for identifying lung cancer. The cutoff value of the perfusion index (PI) is defined as the point with the shortest distance to the left upper corner of the ROC coordinate system (toroid). \(-\mathrm{LR} = {{{\left( {1-\mathrm{sensitivity}} \right)}} \left/ {\mathrm{specificity}} \right.} \) and \( +\mathrm{LR}={{\mathrm{sensitivity}} \left/ {{\left( {1-\mathrm{specificity}} \right)}} \right.} \)
There are limitations to this study. The overlap of the two circulations may undermine the validity of the perfusion measurements. A high injection rate and therefore short injection duration was achieved to reduce such overlap by bolus injection of CM through the left and right antecubital veins (Fig. 5) [2]. The integration of the diagnostic information from CT morphology and perfusion was proposed to be more helpful in the differential diagnosis than using perfusion measurements alone [17]. Thus, the usefulness of the integration of CT morphology and DI-CTP needs to be assessed further. Considering the diversity of the pathological types of lung tumours and differences in haemodynamics in various pathological conditions, the relatively small sample size of this investigation will unavoidably lead to selection bias and therefore biased results to some extent. Therefore, population-based investigation is warranted to further determine the clinical utility of these findings. The radiation exposure is an inherent limitation of perfusion CT, which increases with tube voltage, tube current, and the number of CT volume exposures. In order to keep the overall radiation dose within the range of clinical utility, we reduced the kV and mA in CT perfusion so that the dose was comparable with a triphasic abdominal imaging procedure [18, 19].
In conclusion, the PI derived from dual-input maximum slope CT perfusion, which represents the fraction of pulmonary circulation and systemic circulation in SPNs, is a useful biomarker for identifying malignancy vs. benignity in solitary pulmonary nodules. The perfusion index may be potentially useful for lung cancer treatment planning and forecasting the therapeutic effect of radiotherapy treatment.
Abbreviations
- DI-CTP:
-
Dual-input maximum slope CT perfusion
- SPN:
-
Solitary pulmonary nodule
- PA:
-
Pulmonary artery
- BA:
-
Bronchial artery
- TDCs:
-
Time density curves
- PF:
-
Pulmonary flow
- BF:
-
Bronchial flow
- \( \left( {\mathrm{PI},={{\mathrm{PF}} \left/ {{\left( {\mathrm{PF} + \mathrm{BF}} \right)}} \right.}} \right) \) :
-
Perfusion index
- ROI:
-
Region of interest
- ROC curve:
-
Receiver-operating characteristic curve
- +LR:
-
Positive likelihood ratio
- −LR:
-
Negative likelihood ratio
References
Milne EN (1967) Circulation of primary and metastatic pulmonary neoplasms: a postmortem microarteriographic study. Am J Roentgenol Radium Ther Nucl Med 100:603–619
Yuan X, Zhang J, Ao G et al (2012) Lung cancer perfusion: can we measure pulmonary and bronchial circulation simultaneously? Eur Radiol 22:1665–1671
Nair A, Hansell DM (2011) European and North American lung cancer screening experience and implications for pulmonary nodule management. Eur Radiol 21:2445–2454
Sitartchouk I, Roberts HC, Pereira AM et al (2008) Computed tomography perfusion using first pass methods for lung nodule characterization. Invest Radiol 43:349–358
Li Y, Yang ZG, Chen TW et al (2010) First-pass perfusion imaging of solitary pulmonary nodules with 64-detector row CT: comparison of perfusion parameters of malignant and benign lesions. Br J Radiol 83:785–790
Zhang M, Kono M (1997) Solitary pulmonary nodules: evaluation of blood flow patterns with dynamic CT. Radiology 205:471–478
Lee YH, Kwon W, Kim MS et al (2010) Lung perfusion CT: the differentiation of cavitary mass. Eur J Radiol 73:59–65
Valentin J (2007) Managing patient dose in multi-detector computed tomography (MDCT). Ann ICRP 37:1–79
Luo L, Wang H, Ma H et al (2010) Analysis of 41 cases of primary hypervascular non-small cell lung cancer treated with embolization of emulsion of chemotherapeutics and iodized oil. Zhongguo Fei Ai Za Zhi 13:540–543
Kiessling F, Boese J, Corvinus C (2004) Perfusion CT in patients with advanced bronchial carcinomas: a novel chance for characterization and treatment monitoring? Eur Radiol 14:1226–1233
Ohno Y, Koyama H, Matsumoto K et al (2011) Differentiation of malignant and benign pulmonary nodules with quantitative first-pass 320-detector row perfusion CT versus FDG PET/CT. Radiology 258:599–609
McCullagh A, Rosenthal M, Wanner A et al (2010) The bronchial circulation–worth a closer look: a review of the relationship between the bronchial vasculature and airway inflammation. Pediatr Pulmonol 45:1–13
Wang J, Ning W, Cham MD et al (2009) Tumor response in patients with advanced non–small cell lung cancer: perfusion CT evaluation of chemotherapy and radiation therapy. AJR Am J Roentgenol 193:1090–1096
He H, Lyness JM, McDermott MP (2009) Direct estimation of the area under the receiver operating characteristic curve in the presence of verification bias. Stat Med 28:361–376
Goehring C, Perrier A, Morabia A (2004) Spectrum bias: a quantitative and graphical analysis of the variability of medical diagnostic test performance. Stat Med 23:125–135
Bhandari M, Guyatt GH (2005) How to appraise a diagnostic test. World J Surg 29:561–566
Marten K, Grabbe E (2003) The challenge of the solitary pulmonary nodule: diagnostic assessment with multislice spiral CT. Clin Imaging 27:156–161
Tsai HY, Tung CJ, Yu CC, Tyan YS (2007) Survey of computed tomography scanners in Taiwan: dose descriptors, dose guidance levels, and effective doses. Med Phys 34:1234–1243
Galanski M, Nagel HD, Stamm G (2007) Results of a federation inquiry 2005/2006: pediatric CT X-ray practice in Germany. Rofo 179:1110–1111
Acknowledgements
The authors thank Dr. Kolo of Toshiba Medical Systems for outstanding technical assistance in this study.
Xiadong Yuan and Jing Zhang contributed equally to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuan, X., Zhang, J., Quan, C. et al. Differentiation of malignant and benign pulmonary nodules with first-pass dual-input perfusion CT. Eur Radiol 23, 2469–2474 (2013). https://doi.org/10.1007/s00330-013-2842-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2842-x