Abstract
Objective
To assess and compare the value of whole-body MRI with FDG-PET for detecting bone marrow involvement in lymphoma.
Methods
A total of 116 patients with newly diagnosed lymphoma prospectively underwent whole-body MRI and blind bone marrow biopsy (BMB) of the posterior iliac crest. Of 116 patients, 80 also underwent FDG-PET. Patient-based sensitivities of whole-body MRI for detecting bone marrow involvement were calculated using BMB as reference standard and compared with FDG-PET in aggressive and indolent lymphomas separately.
Results
Sensitivity of whole-body MRI in all lymphomas was 45.5 % [95 % confidence interval (CI): 29.8–62.0 %]. Sensitivity of whole-body MRI in aggressive lymphoma [88.9 % (95 % CI: 54.3–100 %)] was significantly higher (P = 0.0029) than that in indolent lymphoma [23.5 % (95 % CI: 9.1–47.8 %)]. Sensitivity of FDG-PET in aggressive lymphoma [83.3 % (95 % CI: 41.8–98.9 %)] was also significantly higher (P = 0.026) than that in indolent lymphoma [12.5 % (95 % CI: 0–49.2 %)]. There were no significant differences in sensitivity between whole-body MRI and FDG-PET (P = 1.00)
Conclusion
Sensitivity of whole-body MRI for detecting lymphomatous bone marrow involvement is too low to (partially) replace BMB. Sensitivity of whole-body MRI is significantly higher in aggressive lymphoma than in indolent lymphoma and is equal to FDG-PET in both entities.
Key Points
• Bone marrow involvement in lymphoma has prognostic and therapeutic implications.
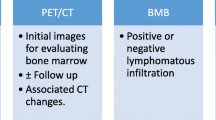
• Blind bone marrow biopsy (BMB) is standard for bone marrow assessment.
• Neither whole-body MRI nor FDG-PET can yet replace BMB.
• Both techniques have higher sensitivity in aggressive than in indolent lymphoma.
• Both imaging techniques are complementary to BMB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lymphomas comprise approximately 5 % of all malignancies and are the sixth most frequently occurring type of cancer in the Western world [1]. Diagnosis of bone marrow involvement is of great importance in lymphoma, because its presence indicates the highest Ann Arbor stage (stage IV), and this may have prognostic and therapeutic implications [2–5]. Blind bone marrow biopsy (BMB) of the iliac crest is the standard method for assessing the bone marrow in lymphoma. However, BMB is invasive and has a small but non-negligible risk of complications [6]. In addition, this method may suffer from sampling errors (i.e. risk of false negatives) as BMB only assesses a very small and random portion of the bone marrow [7–10]. Identification of patients who are unlikely to have bone marrow involvement would be advantageous to spare patients from invasive and diagnostically limited BMB [11].
Magnetic resonance imaging (MRI) provides a non-invasive means of visualising the bone marrow at high spatial resolution [12, 13]. Moreover, MRI can be used as a whole-body technique (whole-body MRI) to visualise bone marrow throughout the entire body, thereby avoiding sampling errors. If whole-body MRI is sufficiently sensitive (and has a high negative predictive value), it can be used to exclude lymphomatous bone marrow involvement and prevent unnecessary BMBs. So far, only a limited number of studies with small sample sizes have evaluated the value of whole-body MRI in this setting [14–16]. 18F-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) is another whole-body investigation that is often used for the evaluation of lymphoma [17], and, depending on the lymphoma subtype (particularly the degree of aggressiveness), may be useful for detecting bone marrow involvement [18, 19]. So far, only one small study has compared whole-body MRI with FDG-PET for the detection of lymphomatous bone marrow involvement [15]. Finally, it is still unknown whether the diagnostic performance of whole-body MRI is affected by the type of lymphoma (i.e. aggressive vs. indolent) under evaluation.
The purpose of this prospective study in 116 patients was therefore to assess the value of whole-body MRI for the detection of bone marrow involvement in lymphoma (using BMB as the standard of reference) and to compare it with FDG-PET in aggressive and indolent lymphomas separately.
Materials and methods
Patients
This prospective multicentre study was institutional review board approved and all patients provided written informed consent. The parent(s) or guardian(s) of all patients under 18 years of age also provided written informed consent. Inclusion criteria were: patients aged 8 years or older with newly diagnosed (histologically proven) Hodgkin or non-Hodgkin lymphoma, written informed consent before the start of the study, blind BMB had to have been performed before the start of treatment, and there must have been sufficient time to perform whole-body MRI before the start of treatment. Exclusion criteria were: patients with a general contraindication for MRI (including cardiovascular pacemakers, claustrophobia), patients physically or psychologically unable to undergo a whole-body MRI examination, patients with a previous malignancy, patients who were pregnant or nursing, and patients in whom therapy had already started. All patients also underwent blind BMB of the posterior iliac crest as part of standard clinical care before the start of treatment. Pretreatment FDG-PET was also performed as part of standard clinical care in some patients, at the request of the treating haematologists (pretreatment FDG-PET was performed in all patients in two of three participating centres, and only in Hodgkin lymphoma in the other participating centre); this decision was not influenced by whole-body MRI or BMB findings.
A total of 135 patients were potentially eligible for inclusion. However, 14 patients had to be excluded because no BMB was performed, 3 patients were excluded because of a diagnosis other than lymphoma, 1 patient was excluded because treatment had already started, and 1 patient was excluded from repeated inclusion (i.e. she had already been included previously). Thus, 116 patients were finally included in this study, 48 of whom had been included in a previous analysis [16]. Patient characteristics are displayed in Tables 1 and 2. All patients underwent whole-body MRI and BMB. Four patients who could not tolerate the MRI examination for more than 30 min and 1 patient with a spondylodesis only underwent T1W and T2W-STIR whole-body MRI without DWI. In 80 of the 116 patients, FDG-PET was also performed. The mean time interval between whole-body MRI and BMB was 9.1 days [standard deviation (SD): 11.1 days, range: 0–59 days]. In 84 of the 116 patients, whole-body MRI was performed after BMB. The mean time interval between FDG-PET and BMB was 10.8 days (SD: 9.9 days, range: 0–45 days). In 35 out of 80 patients, FDG-PET was performed after BMB.
Whole-body MRI
Whole-body MRI was performed at 1.5 T (Achieva, Philips Healthcare, Best, The Netherlands or Magnetom Avanto, Siemens Healthcare, Erlangen, Germany). First, coronal multishot turbo spin-echo T1-weighted (T1W) [repetition time (TR): 537 ms, echo time (TE): 18 ms, slice thickness/gap: 6/1 mm, field of view (FOV): 500–530 × 265, matrix: 208 × 287] and T2-weighted short inversion time inversion recovery (T2W-STIR) [TR: 2,444 ms, TE: 64 ms inversion time (TI): 165 ms, slice thickness/gap: 6/1 mm, FOV: 500–530 × 265, matrix: 336 × 120] turbo spin-echo whole-body images were acquired using either the built-in body coil (Achieva) or phased-array surface coils (Magnetom Avanto) for signal reception. Second, axial single-shot spin-echo echo-planar imaging diffusion-weighted images [TR: 6,962 or 8,612 ms, TE: 78 ms inversion time (TI): 180 ms, slice thickness/gap: 4/0 mm, FOV: 450 × 360, matrix: 128 × 81, b-values of 0 and 1,000 s/mm2] of the head/neck, chest, abdomen, and pelvis were acquired using phased-array surface coils for signal reception. Total actual MR data acquisition times were 12–15 min for T1W, 12–15 min for T2W-STIR and 20–25 min for diffusion-weighted imaging (DWI), with a total MR examination time of 45–55 min. Seamless coronal whole-body T1W and T2W-STIR images were created by merging separately acquired stations. Axial diffusion-weighted images were first coronally reformatted with a slice thickness/gap of 7/0 mm and then merged to create seamless coronal whole-body diffusion-weighted images. In addition, radial diffusion-weighted maximum intensity projections (36 projections at 5° increments) in the coronal plane were created.
FDG-PET
FDG-PET was performed with four different PET systems (Biograph 40 TruePoint PET-CT, Siemens Healthcare; Biograph mCT, Siemens Healthcare; Philips Gemini TOF PET-CT, Philips Healthcare; or Allegro; Philips Healthcare). Patients fasted for at least 6 h before receiving 2.0–3.7 MBq/kg body weight of FDG intravenously. Before injection of FDG, blood glucose levels were less than 11 mmol/l (i.e. less than 198 mg/dl). Image acquisition was performed 60 min after FDG injection. PET images were acquired with a 3D acquisition, from mid-femur to the base of the skull, in 5–7 bed positions, with 2–3 min per bed position. Low-dose computed tomography (CT) (Biograph 40 TruePoint PET-CT and Biograph mCT), full-dose CT (Philips Gemini TOF PET-CT) or a line source (Allegro) was used for attenuation correction of the PET images, which were reconstructed with OSEM (Biograph 40 TruePoint PET-CT, Biograph mCT, and Philips Gemini TOF PET-CT) or 3D-RAMLA (Allegro) iterative reconstruction. Axial, sagittal, coronal and maximum intensity projections were created. PET images were coregistered (i.e. side-by-side display and software-based fusion) to low-dose (Biograph 40 TruePoint PET-CT and Biograph mCT) or full-dose (Philips Gemini TOF PET-CT and Allegro) CT images.
BMB
Unilateral BMB of the posterior iliac crest was performed by different haematologists as part of routine clinical care. Biopsies were interpreted by different experienced haematopathologists who were blinded to whole-body MRI, FDG-PET and other imaging findings.
Image analysis
Whole-body MRI and FDG-PET data sets were transferred to a Picture Archiving and Communications System (PACS, Sectra Medical Systems). A board-certified radiologist (R.A.J.N.) with more than 15 years of clinical experience with (body) MRI and 1 year of experience with whole-body MRI at the start of this study, who was blinded to BMB and FDG-PET findings, evaluated the whole-body magnetic resonance images for the presence or absence of bone marrow involvement. At whole-body MRI, bone marrow involvement was considered present if both the T1W sequences demonstrated any focal areas with signal intensity equal to or lower than that of surrounding muscle and intervertebral discs, and the T2W-STIR sequence demonstrated that the same area had signal intensity higher than that of surrounding muscle. In addition, bone marrow infiltration was considered present if DWI showed any focal area with a signal intensity that exceeded that of the surrounding background. When findings were questionable, any signal intensity higher than that of the spinal cord was considered positive for bone marrow involvement at DWI. Diffusely (non-focal) increased signal intensity at T2W-STIR and DWI may be due to red bone marrow hyperplasia [12, 13] and was not considered positive for lymphomatous bone marrow infiltration.
A board-certified nuclear medicine physician (B.d.K., with more than 6 years of clinical experience with FDG-PET) who was blinded to BMB and whole-body MRI findings evaluated the FDG-PET images for the presence or absence of bone marrow involvement. At FDG-PET, focally increased FDG uptake relative to the surrounding bone marrow was considered positive for bone marrow involvement. Concomitant low-dose or full-dose CT images were used to localise foci of increased FDG uptake. Diffusely increased bone marrow FDG uptake may be due to paraneoplastic red bone marrow activation/inflammation [20] and was not considered positive for lymphomatous bone marrow infiltration.
Both the whole-body MRI reader and FDG-PET reader were aware that the patients had lymphoma, but were unaware of the lymphoma subtype and grade. Observers were aware that BMB may have been performed before (whole-body MRI or FDG-PET) imaging. Note that BMB usually causes a mild signal change (on MRI) at a limited portion of the posterior iliac crest, with a characteristic shape (on both MRI and CT), making differentiation from lymphomatous bone marrow involvement relatively straightforward.
Statistical analysis
As BMB can miss focal bone marrow involvement (previous studies have shown that 10–60 % patients with unilaterally proven bone marrow involvement have a negative contralateral BMB of the iliac crest [7–10], and that in 33 % of paired ipsilateral BMBs of the iliac crest, only one specimen is positive for bone marrow infiltration [9]), BMB is not a suitable reference standard for calculating specificity and negative and positive predictive values of whole-body MRI and FDG-PET. Furthermore, most patients did not undergo follow-up whole-body MRI studies and were thus not available for assessing the nature of bone marrow lesions seen at pretreatment whole-body MRI. Therefore, only (patient-based) sensitivities of whole-body MRI and FDG-PET for diagnosing bone marrow involvement could be calculated (using BMB as the reference standard), along with binomial exact 95 % confidence intervals (CIs). An imaging investigation was considered to be sufficiently sensitive to (partially) replace BMB if sensitivity was equal to or higher than 95 %. For whole-body MRI, sensitivities were calculated for all lymphomas together and for aggressive and indolent lymphomas separately. For FDG-PET, sensitivities were calculated for only aggressive and indolent lymphomas separately, as it is well-known that diagnostic performance of FDG-PET depends on the aggressiveness of the lymphoma [18, 19]. Hodgkin lymphomas were classified as aggressive lymphomas for analytical purposes. Nodular paragranuloma (an uncommon subtype of Hodgkin lymphoma) and mantle cell lymphoma were classified as intermediate-grade lymphomas (and therefore excluded from the aggressive vs. indolent lymphoma analyses). Differences in sensitivities of whole-body MRI and FDG-PET between aggressive and indolent lymphoma were assessed using the McNemar test. Differences in sensitivity between whole-body MRI and FDG-PET (for aggressive and indolent lymphomas separately) were assessed using Fisher’s exact test. Furthermore, it was determined in how many patients the detection of bone marrow involvement by whole-body MRI would change the Ann Arbor stage [as determined by standard clinical CT, FDG-PET (if available) and BMB]. P values less than 0.05 were considered to indicate a significant difference. Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS), version 17.0.
Post hoc analysis
To support the hypothesis that whole-body MRI and FDG-PET may be complementary to BMB, those cases in which both imaging techniques were positive for bone marrow involvement but BMB was negative were reviewed. Using a combination of pretreatment CT (evident cortical bone destruction was considered positive for bone marrow involvement, based on the fact that the bone marrow is the first location that is affected in malignant bone involvement, then followed by the cortical bone [21]) and/or follow-up FDG-PET and MRI [a decrease in bone marrow FDG uptake and decrease in bone marrow signal abnormalities after therapy were considered positive for (initial) bone marrow involvement] as the reference standard, an attempt was made to resolve discrepancies between whole-body MRI/FDG-PET and BMB.
Results
Table 2 shows all whole-body MRI, FDG-PET and BMB results according to lymphoma subtype. Sensitivity of whole-body MRI in all lymphomas was 45.5 % [95 % confidence interval (CI): 29.8–62.0 %] (Table 3). Sensitivity of whole-body MRI in aggressive lymphoma [88.9 % (95 % CI: 54.3–100 %)] was significantly higher (P = 0.0029) than that in indolent lymphoma [23.5 % (95 % CI: 9.1–47.8 %)] (Tables 4 and 5). Sensitivity of FDG-PET in aggressive lymphoma [83.3 % (95 % CI: 41.8–98.9 %)] was also significantly higher (P = 0.026) than that in indolent lymphoma [12.5 % (95 % CI: 0–49.2 %)] (Tables 6 and 7). There were no significant differences in sensitivities between whole-body MRI and FDG-PET in both aggressive and indolent lymphomas (P = 1.00 for both). Detection of bone marrow involvement by whole-body MRI would change the Ann Arbor stage in 7 (6 %) of 116 patients.
Interestingly, whole-body MRI and FDG-PET suggested lymphomatous bone marrow involvement in several cases in which BMB was negative (whole-body MRI: 27 out of 83 cases in all lymphomas, 18 out of 58 cases in aggressive lymphoma, 9 out of 22 cases in indolent lymphoma; FDG-PET: 8 out of 47 cases in aggressive lymphoma and 2 out of 12 cases in indolent lymphoma) (Tables 3, 4, 5, 6 and 7). Post-hoc analysis revealed that seven out of eight whole-body MRI-positive/FDG-PET-positive/BMB-negative cases were true positive for lymphomatous bone marrow involvement (Fig. 1), while one case remained unresolved.
A 67-year-old man with follicular lymphoma in whom whole-body MRI and FDG-PET were positive for a bone marrow lesion in the right ilium, whereas blind bone marrow biopsy (BMB) of the right posterior iliac crest was negative. Coronal T1W (a), T2W-STIR (b), greyscale inverted DWI (c) and axial FDG-PET (d) (with concomitant CT [e] for anatomical localisation) all show a lesion in the bone marrow of the right ilium (arrows), suggestive of lymphomatous infiltration. Post-treatment coronal T1W (f), T2W-STIR (g), greyscale inverted DWI (h) and axial FDG-PET (i) (with concomitant CT [j] for anatomical correlation) show resolution of the right iliac bone marrow lesion (only slightly high signal intensity can still be seen at T2W-STIR (g, dashed arrow). These follow-up findings are strongly suggestive that both whole-body MRI and FDG-PET were true positive for lymphomatous bone marrow involvement, whereas BMB was false negative
Discussion
This investigation revealed several clinically relevant findings. First, although the results of this study show that whole-body MRI is still insufficiently sensitive for the detection of lymphomatous bone marrow involvement (in line with our previous analysis in 48 patients [16]), the same applies to FDG-PET; its sensitivity is also too low to (partially) replace BMB, both in aggressive and indolent lymphomas. Sensitivity of FDG-PET in aggressive lymphoma was found to be significantly higher than that in indolent lymphoma, which is in line with previous studies [18, 19]. One explanation for this finding may be the well-known higher FDG avidity for aggressive lymphoma [22, 23]. Remarkably, the sensitivity of whole-body MRI in aggressive lymphoma was also significantly higher than that in indolent lymphoma. This rather unexpected finding cannot be completely explained. However, it can be speculated that lymphomatous bone marrow involvement in indolent lymphoma may be either less extensive and/or may present with less densely packed lymphomatous cells in the bone marrow compared with aggressive lymphoma, thus decreasing its visibility at both MRI and FDG-PET. However, a previous study reported no significant differences in ADCs of lymph nodes between indolent and aggressive lymphomas [24], which does not support this hypothesis. Thus, further research is required to elucidate the relationship between lymphoma subtype and visibility of lymphomatous bone marrow lesions at MRI. In this study, sensitivities of whole-body MRI and FDG-PET were not significantly different in either aggressive or indolent lymphoma. Another intriguing finding was that seven out of eight whole-body MRI-positive/FDG-PET-positive/BMB-negative cases were classified post hoc as true positive for lymphomatous bone marrow involvement. Thus, there is compelling evidence that both whole-body MRI and FDG-PET are complementary to BMB (i.e. improve its sensitivity); this potential may be realised as either blind BMB combined with imaging or imaging in combination with image-guided BMB. Positive imaging findings in these BMB-negative patients may also have prognostic consequences [25].
Two previous studies [14, 15] reported the value of whole-body MRI for bone marrow assessment compared with BMB. Brennan et al. [14] investigated 23 patients with lymphoma, 17 of whom were in clinical remission and 6 were being actively treated for disease. BMB results were available in 18 patients. MRI correctly predicted bone marrow invasion in two patients, yielding a patient-based sensitivity of 100 % (95 % CI: 34.2–100 %) [14]. In another study by Ribrag et al. [15] in 43 patients with newly diagnosed lymphoma, both whole-body MRI and FDG-PET showed focal bone marrow abnormalities in 9 patients, 2 of whom had confirmation by BMB. Their results also correspond to a high patient-based sensitivity of 100 % (95 % CI: 34.2–100 %) [15]. A major limitation of the studies by Brennan et al. [14] and Ribrag et al. [15] is that a very low number of patients with histologically proven bone marrow involvement was included (n = 2 in both studies); this explains the very wide 95 % CIs for sensitivity in their studies. Furthermore, Brennan et al. [14] only included four patients with indolent lymphomas, whereas Ribrag et al. [15] exclusively included patients with aggressive lymphomas. Thus, the results of previous studies on the value of whole-body MRI for diagnosing bone marrow involvement are rather inconclusive and are mainly applicable to patients with aggressive lymphomas. Moreover, no comprehensive comparison was made between whole-body MRI and FDG-PET by these studies [14, 15].
The present study had several limitations. First, only patients with newly diagnosed lymphoma were included. Second, the diagnostic performance of whole-body MRI and FDG-PET in specific lymphoma subtypes could not be assessed because of the low numbers of patients included for each lymphoma subtype. Rather, lymphomas were categorised as either aggressive or indolent lymphoma. Perhaps BMB can be omitted in certain lymphoma subtypes, as has been indicated by recent FDG-PET studies in Hodgkin lymphoma [26, 27]. Third, most BMBs were obtained before whole-body MRI and FDG-PET. However, it was not possible to schedule all imaging examinations before BMB for logistic reasons at our institutions. Nevertheless, the observers were aware of this issue, and post-biopsy changes can easily be recognised on whole-body MRI and FDG-PET (with concomitant CT) and differentiated from lymphomatous infiltration. Fourth, only T1W and T2W-STIR sequences were acquired of the entire body, whereas DWI and FDG-PET only covered the area from the base of the skull to mid femur. Nevertheless, malignant bone marrow lesions are most frequently localised in the red marrow because of its richer blood supply compared with yellow marrow [12, 13]. In addition, most of the red bone marrow of this mainly adult population (by the age of 25 years, the red marrow is predominantly seen in the axial skeleton and in the proximal part of the appendicular skeleton) was included in the field of view (FOV) of both DWI and FDG-PET. Furthermore, a previous study has shown that whole-body MRI does not detect any clinically relevant lesions (i.e. lesions that change Ann Arbor stage) outside the FOV of an MRI protocol that only includes the head/neck and trunk [28]. Fifth, BMB is an imperfect reference standard, but it was practically and ethically impossible to obtain biopsies of all imaging-positive bone marrow locations. Because BMB was used as reference standard, it was also impossible to assess the negative predictive values of whole-body MRI and FDG-PET. Sixth, inter-rater agreements of whole-body MRI and FDG-PET were not assessed.
In conclusion, sensitivity of whole-body MRI for detecting lymphomatous bone marrow involvement is still too low to (partially) replace BMB in lymphoma. Sensitivity of whole-body MRI is significantly higher in aggressive lymphoma than in indolent lymphoma, and is equal to FDG-PET in both entities. Both whole-body MRI and FDG-PET are complementary to BMB.
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Connors JM (2005) State-of-the-art therapeutics: Hodgkin’s lymphoma. J Clin Oncol 23:6400–6408
Shankland KR, Armitage JO, Hancock BW (2012) Non-Hodgkin lymphoma. Lancet 380:848–587
Lister TA, Crowther D, Sutcliffe SB et al (1989) Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswolds meeting. J Clin Oncol 7:1630–1636
Armitage JO (2005) Staging non-Hodgkin lymphoma. CA Cancer J Clin 55:368–376
Bain BJ (2006) Morbidity associated with bone marrow aspiration and trephine biopsy - a review of UK data for 2004. Haematologica 91:1293–1294
Brunning RD, Bloomfield CD, McKenna RW, Peterson LA (1975) Bilateral trephine bone marrow biopsies in lymphoma and other neoplastic diseases. Ann Intern Med 82:365–366
Coller BS, Chabner BA, Gralnick HR (1977) Frequencies and patterns of bone marrow involvement in non-Hodgkin lymphomas: observations on the value of bilateral biopsies. Am J Hematol 3:105–119
Haddy TB, Parker RI, Magrath IT (1989) Bone marrow involvement in young patients with non-Hodgkin’s lymphoma: the importance of multiple bone marrow samples for accurate staging. Med Pediatr Oncol 17:418–423
Wang J, Weiss LM, Chang KL et al (2002) Diagnostic utility of bilateral bone marrow examination: significance of morphologic and ancillary technique study in malignancy. Cancer 94:1522–1531
Bairey O, Shpilberg O (2007) Is bone marrow biopsy obligatory in all patients with non-Hodgkin’s lymphoma? Acta Haematol 118:61–64
Vande Berg BC, Malghem J, Lecouvet FE, Maldague B (1998) Magnetic resonance imaging of normal bone marrow. Eur Radiol 8:1327–1334
Vande Berg BC, Lecouvet FE, Michaux L, Ferrant A, Maldague B, Malghem J (1998) Magnetic resonance imaging of the bone marrow in hematological malignancies. Eur Radiol 8:1335–1344
Brennan DD, Gleeson T, Coate LE, Cronin C, Carney D, Eustace SJ (2005) A comparison of whole-body MRI and CT for the staging of lymphoma. AJR Am J Roentgenol 185:711–716
Ribrag V, Vanel D, Leboulleux S et al (2008) Prospective study of bone marrow infiltration in aggressive lymphoma by three independent methods: whole-body MRI, PET/CT and bone marrow biopsy. Eur J Radiol 66:325–331
Kwee TC, Fijnheer R, Ludwig I et al (2010) Whole-body magnetic resonance imaging, including diffusion-weighted imaging, for diagnosing bone marrow involvement in malignant lymphoma. Br J Haematol 149:628–630
Delbeke D, Stroobants S, de Kerviler E, Gisselbrecht C, Meignan M, Conti PS (2009) Expert opinions on positron emission tomography and computed tomography imaging in lymphoma. Oncologist 14:30–40
Pakos EE, Fotopoulos AD, Ioannidis JP (2005) 18F-FDG PET for evaluation of bone marrow infiltration in staging of lymphoma: a meta-analysis. J Nucl Med 46:958–963
Chen YK, Yeh CL, Tsui CC, Liang JA, Chen JH, Kao CH (2011) F-18 FDG PET for evaluation of bone marrow involvement in non-Hodgkin lymphoma: a meta-analysis. Clin Nucl Med 36:553–559
Salaun PY, Gastinne T, Bodet-Milin C et al (2009) Analysis of 18F-FDG PET diffuse bone marrow uptake and splenic uptake in staging of Hodgkin’s lymphoma: a reflection of disease infiltration or just inflammation? Eur J Nucl Med Mol Imaging 36:1813–1821
Basu S, Torigian D, Alavi A (2008) Evolving concept of imaging bone marrow metastasis in the twenty-first century: critical role of FDG-PET. Eur J Nucl Med Mol Imaging 35:465–471
Weiler-Sagie M, Bushelev O, Epelbaum R et al (2010) (18)F-FDG avidity in lymphoma readdressed: a study of 766 patients. J Nucl Med 51:25–30
Tsukamoto N, Kojima M, Hasegawa M et al (2007) The usefulness of (18)F-fluorodeoxyglucose positron emission tomography ((18)F-FDG-PET) and a comparison of (18)F-FDG-pet with (67)gallium scintigraphy in the evaluation of lymphoma: relation to histologic subtypes based on the World Health Organization classification. Cancer 110:652–659
Kwee TC, Ludwig I, Uiterwaal CS et al (2011) ADC measurements in the evaluation of lymph nodes in patients with non-Hodgkin lymphoma: feasibility study. MAGMA 24:1–8
Tsunoda S, Takagi S, Tanaka O, Miura Y (1997) Clinical and prognostic significance of femoral marrow magnetic resonance imaging in patients with malignant lymphoma. Blood 89:286–29
Moulin-Romsee G, Hindié E, Cuenca X et al (2010) (18)F-FDG PET/CT bone/bone marrow findings in Hodgkin’s lymphoma may circumvent the use of bone marrow trephine biopsy at diagnosis staging. Eur J Nucl Med Mol Imaging 37:1095–1105
El-Galaly TC, d’Amore F, Mylam KJ et al (2012) Routine bone marrow biopsy has little or no therapeutic consequence for positron emission tomography/computed tomography-staged treatment-naive patients with Hodgkin lymphoma. J Clin Oncol 30:4508–4514
Kwee TC, Akkerman EM, Fijnheer R et al (2011) MRI for staging lymphoma: whole-body or less? J Magn Reson Imaging 33:1144–1150
Acknowledgments
This project was financially supported by the Dutch Organisation for Health Research and Development (ZonMw) Programme for Health Care Efficiency Research (grant no. 80-82310-98-08012) and by a ZonMW AGIKO stipend (grant no. 92003497). Data collection, data analysis and interpretation of data, writing of the paper and the decision to submit were left to the authors’ discretion and were not influenced by ZonMw.
Forty-eight of 116 included patients were included in our previously published preliminary analysis (Kwee TC, Fijnheer R, Ludwig I, et al. (2010) Whole-body magnetic resonance imaging, including diffusion-weighted imaging, for diagnosing bone marrow involvement in malignant lymphoma. Br J Haematol 149:628–630). In that previous study, however, no definitive conclusions could be drawn, no comparison was made with FDG-PET, and no analyses were made for aggressive and indolent lymphomas separately. The present study provides substantially new information and allows drawing more definitive conclusions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adams, H.J.A., Kwee, T.C., Vermoolen, M.A. et al. Whole-body MRI for the detection of bone marrow involvement in lymphoma: prospective study in 116 patients and comparison with FDG-PET. Eur Radiol 23, 2271–2278 (2013). https://doi.org/10.1007/s00330-013-2835-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2835-9