Abstract
Objectives
To assess the diagnostic accuracy and reliability of MRI without contrast enhancement in the evaluation of JIA knee joint abnormalities.
Methods
JIA patients with clinically active knee involvement were prospectively studied using an 1-T open-bore magnet. MRI features were independently evaluated by two readers using the JAMRIS system. The first reading included unenhanced images, whereas complete image sets were available for the second reading.
Results
Imaging findings from 73 patients were analysed. Agreement between Gd-enhanced (+Gd) and Gd-unenhanced (−Gd) MRI scores of bone marrow changes, cartilage lesions and bone erosions was good concerning sensitivity, specificity, negative predictive value and positive predictive value. Inter-observer agreement was good for both −Gd and +Gd scores (ICC = 0.91–1.00, 0.93–1.00, respectively). Regarding the assessment of synovial hypertrophy, specificity of −Gd was high (0.97), but the sensitivity of unenhanced MRI was only 0.62. Inter-reader agreement for +Gd MRI was ICC = 0.94; however, omitting post-Gd acquisitions increased inter-reader variation (ICC = 0.86).
Conclusions
If Gd-enhanced MRI is the reference standard, omitting Gd contrast medium is irrelevant for the assessment of bone marrow changes, cartilage lesions and bone erosions as joint abnormalities in JIA. Omitting intravenous Gd in the MRI assessment of joints in JIA is inadvisable, because it decreases the reliability of detecting synovial disease.
Key Points
• Magnetic resonance imaging is increasingly used to assess juvenile idiopathic arthritis.
• Synovial hypertrophy, a marker of JIA activity, is well shown by MRI.
• Omitting intravenous contrast medium decreases the reliability of synovial hypertrophy scores.
• Bone marrow, cartilage and erosions can be reliably evaluated without contrast enhancement.
• In the evaluation of JIA disease activity, unenhanced MRI is inadvisable.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis (JIA) is the most common autoinflammatory musculoskeletal disease in childhood, with a prevalence that varies between 16 and 150 per 100,000 [1]. JIA is not a single disease, but a term that encompasses all forms of arthritis of unknown aetiology that begins before the age of 16 years and persists for more than 6 weeks [2]. It is characterised by prolonged synovial inflammation that can lead to the destruction of joints, pain and loss of function [1].
In JIA, early disease control improves long-term outcome. Therefore, sensitive measures to assess disease status, individual response to therapy and general efficacy of treatment in JIA are warranted [3, 4]. Physical examination, even by an experienced observer, has only limited reliability [5]. Conventional radiography is insensitive in detecting soft tissue changes such as synovitis, which is one of the critical hallmarks of disease activity in JIA, as well as in detecting the earliest stages of persistent erosive changes [6]. Within the past 10 years, the use of magnetic resonance imaging (MRI) and advances in MRI techniques have substantially improved the evaluation of joint abnormalities in JIA patients [7]. To date, MRI is considered to be the most suitable imaging technique in inflammatory joint disease as it is the most sensitive imaging technique for the detection of both synovial hypertrophy and bone marrow changes suggestive of bone marrow oedema [8].
Currently, evidence is lacking on the important practical issue of whether to use an intravenous injection of gadolinium-containing contrast agents (Gd) or not in paediatric JIA patients. Without the use of intravenous Gd, T2-weighted fat-saturated sequences display areas with high water content as hyper-intense areas, enabling the visualisation of inflamed oedematous synovium. Therefore, the aim of our study was to assess the diagnostic accuracy and reliability of MRI without Gd enhancement in the evaluation of disease in the most commonly affected joint in JIA (i.e. the knee) compared with Gd-enhanced MRI as the reference standard.
Materials and methods
Patients
Patients visited one of the outpatient clinics of two tertiary paediatric rheumatology centres (Emma Children’s Hospital/Academic Medical Centre and Reade, both in Amsterdam, The Netherlands). All patients fulfilled the International League of Associations for Rheumatology (ILAR) criteria for JIA, defined as arthritis of unknown aetiology that begins before the age of 16 and persists for at least 6 weeks [2]. For ILAR classification, all newly diagnosed JIA patients were clinically evaluated and reclassified if necessary after a period of 6 months. Inclusion criteria were clinically active disease with knee involvement; therefore patients comprised newly diagnosed JIA patients and patients with clinically active arthritis due to relapsing disease. Exclusion criteria were a history of intra-articular corticosteroid injection within the last 6 months, the need for anaesthesia during the MRI examination and general contraindications for MRI. This study was approved by the institutional review board. Written informed consent was acquired from at least one parent of each child.
MRI protocol and image analysis
Magnetic resonance images were obtained using an open-bore 1.0-T magnet (Panorama HFO, Philips Medical Systems, Best, The Netherlands). The children were placed in the supine position with the knee joint centrally in the magnetic field in a dedicated knee coil. No sedation was used. See Table 1 for the sequences acquired.
The MRI data sets were independently scored twice by a musculoskeletal radiologist (MM, 17 years’ experience in musculoskeletal radiology) and a radiology trainee (RH, 4 years’ experience in musculoskeletal radiology) who were blinded to the clinical history, including the duration, extent and severity of the symptoms. The first reading (−Gd) included only images obtained without IV contrast (sagittal, coronal and axial T2-weighted fat-saturated images, plus sagittal T1-weighted images). For the second reading (+Gd) the complete MRI data set was available for scoring (additional data; sagittal T1-weighted images and axial T1-weighted fat-saturated images obtained after contrast medium injection). Time between the two reading sessions was at least 6 months.
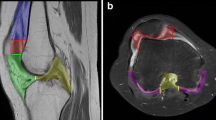
The MR images were scored in accordance with the Juvenile Arthritis MRI Scoring (JAMRIS) system. The reliability of JAMRIS and definitions according to the JAMRIS system are described elsewhere in detail [9]. Briefly, synovial hypertrophy was scored semi-quantitatively based on the maximal thickness in any slice (grade 0, <2 mm; grade 1, 2–4 mm; grade 2, >4 mm) at six sites of the knee joint (patellofemoral, suprapatellar recesses, infrapatellar fat pad, adjacent to the cruciate ligaments, and adjacent to the medial and lateral posterior condyle). Bone marrow changes suggestive of bone marrow oedema, cartilage lesions and bone erosions were scored in eight anatomical regions (medial and lateral patella, medial and lateral femoral condyle, medial and lateral weight-bearing femur, and medial and lateral tibial plateau) based on the percentage of the surface area/bone volume involved at each site (grade 0, none; grade 1, <10 % of surface area/bone volume; grade 2, 10–25 % of surface area/bone volume; grade 3, >25 % of surface area/bone volume).
Reference standard
Following both readings, MRI scores of cases with any discrepancy between readers were re-evaluated in consensus, whereafter the final score was given. Accordingly, the consensus score of contrast-enhanced MRI was considered to be the reference standard.
Statistics
Sensitivity, specificity, negative predictive value and positive predictive value of unenhanced MRIs were calculated (cutoff value of score ≥1) with Gd-enhanced MRI as the reference standard. The single-measure intraclass correlation coefficient (ICC) was used to analyse inter-reader reliability and was classified as follows: ICC <0.40 = poor, ≥0.40–0.60 = moderate, >0.60–0.80 = substantial and >0.80 = good reliability. All data were analysed using SPSS version 16.0 (SPSS, Chicago, IL, USA).
Results
Patients
We prospectively collected data of 85 consecutive patients between December 2008 and June 2010. Twelve (14.1 %) patients were excluded: 1 was diagnosed with osteochondritis dissecans by MRI and 11 patients, who initially had suspected JIA, were later reclassified because of a non-rheumatological ailment. Therefore, findings from 73 JIA patients were analysed (60.3 % female patients). The mean age was 13.0 years (SD 3.3). The frequency of clinical JIA subtypes was as follows: 17 (23.3 %) persistent oligoarthritis, 13 (17.8 %) extended oligoarthritis, 27 (37.0 %) rheumatoid factor-negative polyarthritis, 1 (1.4 %) rheumatoid factor-positive polyarthritis, 1 (1.4 %) systemic disease, 2 (2.7 %) psoriatic arthritis, 10 (13.7 %) enthesitis-related arthritis and 2 (2.7 %) undifferentiated JIA. Of these patients, 13 (17.8 %) received no medication, 13 (17.8 %) used NSAIDs, 38 (52.1 %) used additional systemic DMARDs, and 9 (12.3 %) were also treated with a TNF-α inhibitor. The image quality was sufficient in all patients. All children had been able to finish the complete examination.
MRI findings
As shown in Table 2, the agreement between Gd-enhanced and Gd-unenhanced MRI scores regarding bone marrow changes, cartilage lesions and bone erosions were good concerning sensitivity, specificity, negative predictive value and positive predictive value. Moreover, the inter-observer agreement was good for both −Gd and +Gd scores (Table 3). Figures 1, 2 and 3 show the influence of Gd on the MRI assessment of bone marrow changes, cartilage lesions and bone erosions, respectively.
Bone marrow changes suggestive of bone marrow oedema, observed in both readings (−Gd and +Gd). Sagittal MR images obtained in a 14-year-old boy with bone marrow changes in the lateral weight-bearing femur (arrows). a Fat-saturated T2-weighted images, b T1-weighted images obtained before the administration of intravenous contrast agent and c T1-weighted images obtained after the administration of an intravenous contrast agent. The administration of intravenous Gd resulted in enhancement of the bone marrow oedema. However, it had no influence on the agreement or reliability
Cartilage lesion, observed in both readings (−Gd and +Gd). Sagittal MR images obtained in a 12-year-old girl with a cartilage lesion in the lateral femoral condyle (arrows). a Fat-saturated T2-weighted images, b T1-weighted images obtained before the administration of intravenous contrast agent and c T1-weighted images obtained after the administration of an intravenous contrast agent
Bone erosion observed in both readings (−Gd and +Gd). Sagittal MR images obtained in a 17-year-old girl with an evident bone erosion in the medial tibial plateau (arrows). a Fat-saturated T2-weighted images, b T1-weighted images obtained before the administration of intravenous contrast agent and c T1-weighted images obtained after the administration of an intravenous contrast agent show enhancement of the bone erosion. However, it had no influence on the agreement or reliability
Regarding the assessment of synovial hypertrophy the specificity of −Gd was high (0.97), although the sensitivity of unenhanced MRI was somewhat lower (0.62). Inter-reader agreement for +Gd MRI was ICC 0.94; however, omitting post-Gd acquisitions increased inter-reader variation (ICC 0.86). Grade 1 synovial hypertrophy was scored in 33.3 % of the cases as grade 0, 60.8 % as grade 1 and 5.9 % as grade 2 on −Gd MRI. Further, grade 2 was scored in 35.5 % as grade 1, while 64.5 % were scored as grade 2 on unenhanced MR images (Figs. 4 and 5).
Subtle synovial hypertrophy, only observed during the second reading (+Gd). MR images obtained in a 10-year-old girl with subtle synovial hypertrophy: patellofemoral (arrows) and suprapatellar. a Sagittal fat-saturated T2-weighted images, b sagittal T1-weighted images obtained before the administration of intravenous contrast agent, c sagittal T1-weighted images obtained after the administration of an intravenous contrast agent and d axial fat-saturated T1-weighted images after the administration of an intravenous contrast agent
Marked synovial hypertrophy, observed in both readings (−Gd and +Gd). MR images obtained in a 16-year-old boy with evident synovial hypertrophy: patellofemoral, suprapatellar (arrows), infrapatellar and adjacent to the cruciate ligaments (arrows). a Sagittal fat-saturated T2-weighted images, b T1-weighted images obtained before the administration of intravenous contrast agent and c sagittal T1-weighted images obtained after the administration of an intravenous contrast agent. Notice the extended joint effusion in the suprapatellar recesses (*), d sagittal T1-weighted images obtained after the administration of an intravenous contrast agent and d axial fat-saturated T1-weighted images after the administration of an intravenous contrast agent
Discussion
In this study we explored to what extent omitting intravenous contrast agents has an impact on the reliability of MRI assessment scores of JIA knee joint abnormalities. Gd enhancement appeared to be unimportant to MRI scores of bone marrow changes, cartilage lesions and bone erosions. However, when contrast-enhanced MRI was considered the reference standard, unenhanced MRI scores were not as accurate as contrast-enhanced MRI in the assessment of synovial hypertrophy.
The synovial membrane encompasses a small rim of tissue adjacent to the articular surface. It shows a relatively low signal intensity on both T1- and T2-weighted MR images. As reflection of disease activity the signal intensity of inflamed synovium is low to intermediate on T1-weighted MR images and high on T2-weighted images, i.e. indistinguishable from joint effusion. Consequently, Gd is recommended for MRI assessment of joint changes in rheumatoid arthritis (RA), particularly synovial hypertrophy [10]. Most MRI studies of JIA joints have obtained T1-weighted MR images before and after intravenous Gd injection, which facilitates better differentiation between joint effusion and synovial hypertrophy [11–13]. However, the diagnostic accuracy of unenhanced MRI compared with contrast-enhanced MRI for the assessment of JIA joint abnormalities has not been studied systematically to date.
As early disease control improves long-term outcome [3, 4], sensitive and reliable measures to assess individual response to therapy and general efficacy of treatment in JIA are warranted [7]. In JIA the physical examination is only of limited reliability [5], and conventional radiography is insensitive in the detection of early stages of persistent erosive changes [14]. Currently, MRI is the most sensitive imaging tool able to visualise the early inflammatory changes of the synovial membrane, bone marrow changes, and erosive changes of cartilage and bone [6]. Therefore, MRI is considered the most suitable imaging technique for the evaluation of the disease status in patients with JIA [7]. The administration of intravenous Gd in paediatric JIA patients is a relevant issue because the use of Gd markedly prolongs the examination time, increases costs and patient discomfort, and adds the risk of allergic reactions to the contrast agent. Thus, the additional value of contrast-enhanced MRI in the assessment of disease activity in JIA should outweigh its disadvantages. The assessment of synovial hypertrophy is markedly affected by omitting the contrast-enhanced images, unlike the assessments of bone marrow changes, cartilage lesions and bone erosions. Since the development of highly effective antiinflammatory therapies for arthritis, the main goal of treatment has been to obtain total suppression of joint inflammation to prevent destructive changes. Hence, outcome measures in clinical trials should comprise sensitive and reliable measures of joint inflammation. Furthermore, substantial proportions of both RA and JIA patients showed the presence of MRI-based synovial hypertrophy in spite of normalised clinical and laboratory parameters [15–18]. Therefore, accurate evaluation of disease status is warranted. Given the fact that omission of intravenous Gd leads to an increase in inter-reader variation and a decrease in agreement between contrast-enhanced and non-enhanced synovial hypertrophy scores, omitting Gd enhancement in MRI of joints in JIA is inadvisable. This implies that MRI for the evaluation and monitoring of JIA disease status should always be performed with intravenous Gd, which has been shown to be a feasible technique [9].
We evaluated synovial hypertrophy by comparison between T1-weighted images obtained before and after intravenous Gd. Although this technique allows direct visualisation and measurements of the inflamed synovial membrane, it is not able to quantify the heterogeneous biological activity of the synovial membrane. In both JIA and RA, dynamic contrast-enhanced MRI has been suggested as a potentially more objective imaging biomarker to make a distinction in that respect—even when the disease activity is heterogeneously distributed throughout the synovium [19–22]. Another advanced MRI technique that may be valuable in the quantitative evaluation of synovial hypertrophy is diffusion-weighted imaging (DWI) [23]. The contrast-free approach of DWI is attractive, especially in children, but challenges in implementation and analysis currently limit the utility of this technique. To date, these advanced imaging techniques are being used particularly in the scope of research and to a lesser extent in clinical practice.
In the current study, the JAMRIS system for the knee has been used for standardised assessment of inflammatory and destructive changes in JIA, and it has proved to be an easy-to-use and reliable assessment score as the inter-reader reliability of all scored MRI features was good, ranging from ICC 0.86 up to ICC 0.94. These values are comparable to reliability scores described previously [9].
The limitations of our study should be considered. MR images were obtained by using an open-bore 1.0-T magnet. Higher-field MRI units (1.5 T, 3.0 T) could provide greater agreement between the assessments of unenhanced and contrast-enhanced MR images. We used a standardised MRI protocol. By using other/additional sequences—e.g. more post-contrast images with fat-saturation—it could improve agreement between the assessments of unenhanced and contrast-enhanced MR images, but in all probability only to a very limited extent. Another limitation is the lack of MR images of age-matched healthy controls. Because growing joints are subject to change, it may be difficult to establish whether differences in the appearance of the knee joint are pathological or form part of normal maturation. For instance, the prevalence of bony depressions and signal changes suggestive of bone marrow oedema in the wrists and knees of healthy children is high [24, 25].
In conclusion, our study showed that unenhanced MRI enables reliable assessment of bone marrow changes, cartilage lesions and bone erosions as joint abnormalities in knees of patients with proven JIA. However, omission of intravenous Gd leads to an increase in inter-reader variation and decreases the sensitivity for scores of synovial hypertrophy. Omitting intravenous Gd in the MRI assessment of joints in JIA is therefore not advised.
References
Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet 369:767–778
Petty RE, Southwood TR, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
Albers HM, Wessels JA, van der Straaten RJ et al (2009) Time to treatment as an important factor for the response to methotrexate in juvenile idiopathic arthritis. Arthritis Rheum 61:46–51
Vilca I, Munitis PG, Pistorio A et al (2010) Predictors of poor response to methotrexate in polyarticular-course juvenile idiopathic arthritis: analysis of the PRINTO methotrexate trial. Ann Rheum Dis 69:1479–1483
Guzman J, Burgos-Vargas R, Duarte-Salazar C, Gomez-Mora P (1995) Reliability of the articular examination in children with juvenile rheumatoid arthritis: interobserver agreement and sources of disagreement. J Rheumatol 22:2331–2336
Doria AS, Babyn PS, Feldman B (2006) A critical appraisal of radiographic scoring systems for assessment of juvenile idiopathic arthritis. Pediatr Radiol 36:759–772
Miller E, Uleryk E, Doria AS (2009) Evidence-based outcomes of studies addressing diagnostic accuracy of MRI of juvenile idiopathic arthritis. AJR Am J Roentgenol 192:1209–1218
Gylys-Morin VM, Graham TB, Blebea JS et al (2001) Knee in early juvenile rheumatoid arthritis: MR imaging findings. Radiology 220:696–706
Hemke R, van Rossum MA, van Veenendaal M et al (2012) Reliability and responsiveness of the Juvenile Arthritis MRI Scoring (JAMRIS) system for the knee. Eur Radiol. doi:10.1007/s00330-012-2684-y
Østergaard M, Peterfy C, Conaghan P et al (2003) OMERACT Rheumatoid Arthritis Magnetic Resonance Imaging Studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol 30:1385–1386
Gardner-Medwin JM, Irwin G, Johnson K (2009) MRI in juvenile idiopathic arthritis and juvenile dermatomyositis. Ann N Y Acad Sci 1154:52–83
Graham TB, Laor T, Dardzinski BJ (2005) Quantitative magnetic resonance imaging of the hands and wrists of children with juvenile rheumatoid arthritis. J Rheumatol 32:1811–1820
Murray JG, Ridley NT, Mitchell N, Rooney M (1996) Juvenile chronic arthritis of the hip: value of contrast-enhanced MR imaging. Clin Radiol 51:99–102
Doria AS, de Castro CC, Kiss MH et al (2003) Inter- and intrareader variability in the interpretation of two radiographic classification systems for juvenile rheumatoid arthritis. Pediatr Radiol 33:673–681
Lamer S, Sebag GH (2000) MRI and ultrasound in children with juvenile chronic arthritis. Eur J Radiol 33:85–93
Brown AK, Quinn MA, Karim Z et al (2006) Presence of significant synovitis in rheumatoid arthritis patients with disease-modifying antirheumatic drug-induced clinical remission: evidence from an imaging study may explain structural progression. Arthritis Rheum 54:3761–3773
Nistala K, Babar J, Johnson K et al (2007) Clinical assessment and core outcome variables are poor predictors of hip arthritis diagnosed by MRI in juvenile idiopathic arthritis. Rheumatology (Oxford) 46:699–702
Hemke R, van Veenendaal M, Kuijpers TW, van Rossum MA, Maas M (2012) Increasing feasibility and patient comfort of MRI in children with juvenile idiopathic arthritis. Pediatr Radiol 42:440–448
Malattia C, Damasio MB, Basso C et al (2010) Dynamic contrast-enhanced magnetic resonance imaging in the assessment of disease activity in patients with juvenile idiopathic arthritis. Rheumatology (Oxford) 49:178–185
Workie DW, Graham TB, Laor T et al (2007) Quantitative MR characterization of disease activity in the knee in children with juvenile idiopathic arthritis: a longitudinal pilot study. Pediatr Radiol 37:535–543
van der Leij C, van de Sande MG, Lavini C, Tak PP, Maas M (2009) Rheumatoid synovial inflammation: pixel-by-pixel dynamic contrast-enhanced MR imaging time-intensity curve shape analysis—a feasibility study. Radiology 253:234–240
Axelsen M, Stoltenberg M, Poggenborg R et al. (2012) Dynamic gadolinium-enhanced magnetic resonance imaging allows accurate assessment of the synovial inflammatory activity in rheumatoid arthritis knee joints: a comparison with synovial histology. Scand J Rheumatol 41:89–94
Agarwal V, Kumar M, Singh JK, Rathore RK, Misra R, Gupta RK (2009) Diffusion tensor anisotropy magnetic resonance imaging: a new tool to assess synovial inflammation. Rheumatology (Oxford) 48:378–382
Müller LS, Avenarius D, Damasio B et al (2011) The paediatric wrist revisited: redefining MR findings in healthy children. Ann Rheum Dis 70:605–610
Jans LB, Jaremko JL, Ditchfield M, Verstraete KL (2011) Evolution of femoral condylar ossification at MR imaging: frequency and patient age distribution. Radiology 258:880–888
Acknowledgment
This work was supported by a research grant received from the Reumafonds, Dutch Arthritis Association (Amsterdam, The Netherlands). The Dutch Arthritis Association was not involved in designing and conducting this study, did not have access to the data, and was not involved in data analysis or preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hemke, R., Kuijpers, T.W., van den Berg, J.M. et al. The diagnostic accuracy of unenhanced MRI in the assessment of joint abnormalities in juvenile idiopathic arthritis. Eur Radiol 23, 1998–2004 (2013). https://doi.org/10.1007/s00330-013-2770-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2770-9