Abstract
Objective
To assess anatomical risk factors in patients after lateral patellar dislocation (LPD) and controls using MRI.
Methods
MR images of 186 knees after LPD and of 186 age- and gender-matched controls were analysed. The presence of trochlear dysplasia was assessed by evaluation of trochlear inclination, facet asymmetry, and trochlear depth; patella alta was evaluated by the Insall-Salvati index and Caton-Deschamps index; the lateralised force vector was measured by the tibial tuberosity-trochlear groove (TT-TG) distance.
Results
Compared with controls, dislocators had significantly lower values for all three parameters of trochlear dysplasia (−32 %, −32 %, −44 %) and significantly higher values for patella alta (+14 %,+13 %) and TT-TG (+49 %) (all P < 0.001). Trochlear dysplasia was observed in 112 dislocators (66 %), of whom 61 (36 %) additionally had patella alta and 15 (9 %) an abnormal TT-TG. As isolated risk factors, patella alta (15 %) and abnormal TT-TG (1 %) were rare. Only 25 dislocators (15 %) had no anatomical risk factors. Trochlear dysplasia in conjunction with abnormal TT-TG or patella alta is associated with a 37- and 41-fold higher risk.
Conclusion
Most dislocators have anatomical risk factors, varying in severity and constellation.
Key Points
• Magnetic resonance imaging provides unique information about anatomical variation within the knee.
• Anatomical variants increase the risk for lateral patellar dislocation (LPD)
• Trochlear dysplasia is the main risk factor for LPD.
• Patellar alta and abnormal tibial tuberosity-trochlear groove distance may be additional factors.
• Patient-specific evaluation of risk factors following LPD may help future management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The aetiology of patellofemoral instability and subsequent lateral patellar dislocation is not yet fully elucidated. Multifactorial causation is assumed involving developmental anatomical variants of the patellofemoral joint. The resulting structural and functional imbalance appears to predispose individuals to patellar dislocation. The first dislocation is often associated with a traumatic event, which may be minor [1], and can give rise to recurrent dislocations and chronic patellofemoral instability with considerable damage to the knee joint and a loss of quality of life [2–4].
The three most important anatomical variants that have been implicated in lateral patellar dislocation include trochlear dysplasia, patella alta, and an abnormal tibial tubercle-to-trochlear groove (TT-TG) distance [5]. The severity of dislocation-induced damage and the presence and severity of underlying anatomical risk factors are crucial for deciding whether conservative management or surgical correction is the best therapeutic option. Complex surgical correction may be indicated in patients with several anatomical variants. A tailored approach ensuring optimal treatment of each patient crucially relies on an accurate analysis of the underlying pathomechanism, and this is where magnetic resonance imaging (MRI) can make an important contribution [6–8].
An individual patient’s anatomical risk factors can be assessed by determination of a set of standardised parameters from the initial MR images [9]. How exactly the three main risk factors interact and bring about patellofemoral instability is still a matter of debate as patients with patellar instability may have none or all three risk factors and also differ with regard to the severity and constellation of anatomical risk factors present. A consistent body of evidence is not available because published studies are limited by the use of different methods, investigation of small patient populations, or the failure to comprehensively investigate all risk factors and their various combinations [10–15]. The authors of a recent meta-analysis state that our current knowledge does not allow a definitive appraisal of the validity and reliability of the radiologic assessment of patellofemoral instability, concluding that well-designed studies are needed to overcome this situation [16].
The aim of our study was to analyse the three major risk factors—trochlear dysplasia, patella alta, and abnormal TT-TG distance—in a large patient population with a history of patellar dislocation and in an age- and sex-matched control group using MRI. This analysis was done to quantify and compare the prevalences and risk profiles of the individual factors and their patterns in dislocators and controls.
Subjects and methods
Study population
After having obtained approval by the institutional review board, we conducted a database search to identify patients with lateral patellar dislocation (LPD) who had undergone MRI of the knee at one of the three clinical sites of Charité University Medical Center from July 2000 through March 2012.
The patient population included 186 knees (109 left, 77 right) in 180 individuals (101 women, 79 men). The patients had a mean age of 25.4 years (range, 10.3–57 years). Inclusion criteria were a convincing history of patellar dislocation and/or typical MRI signs such as oedema of the inferomedial patella and lateral condyle and tear of the medial patellofemoral ligament. Exclusion criteria were metal implants in the knee area or status post osteotomy on the basis of MR images. Data on the number of prior patellar dislocations were retrieved from the medical records and served to assign the patients to one of two groups: first-time dislocators (one event only) or recurrent dislocators (more than one event). In addition, mechanisms of injury were elucidated and classified according to Balcarek et al. as follows: no-risk pivoting activities (e.g., swimming, cycling, walking), low-risk pivoting activities (e.g., running, hiking, yoga, dancing), high-risk pivoting activities (e.g., soccer, basketball), and direct hits [17]. Data on the number of dislocations were available for 152 dislocators (82.6 %) and data on the mechanism of injury for 83 dislocators (44.6 %).
MRI data sets of 186 knees (89 left, 97 right) from 184 subjects (105 women, 79 men) with knee pain, who were referred for knee MRI by the orthopaedic outpatient service of our hospital, served as controls. The mean age of the control group was 26 years (range, 12.2–47 years) and did not differ significantly from the mean age of the dislocators (P = 0.514). The control group included only patients whose MRI reports described mild meniscal or cartilaginous conditions as the only knee conditions. Patients with significant effusion, meniscal tears, cruciate ligament rupture, or significant cartilage lesions were not accepted as controls.
Magnetic resonance imaging
MR imaging was performed at 1.0 to 3.0 T in one of three associated hospitals on one of seven MRI systems using either a dedicated knee coil or an extremity coil. All patients were imaged in supine position with the knee in mild flexion, depending on the coil used. By way of example, we here present the pulse sequences used in most cases: axial T2-weighted fat-saturated turbo spin echo sequence; coronal T1-weighted spin echo sequence and coronal turbo inversion recovery magnitude sequence; sagittal dual-turbo spin echo sequence with proton-density-weighted and T2-weighted sequences. The protocols used on MR systems C-G were not substantially different.
Imaging evaluation
MR images were evaluated separately on a PACS workstation (Centricity RIS-i 4.2 Plus, GE Healthcare, Milwaukee, WI, USA). The parameters were measured in random order by two readers in consensus. The first reader had 3 years of experience in musculoskeletal radiology and the second reader 9 years. The two readers were blinded to clinical history and data on dislocations. The readers could freely set display parameters such as zoom, brightness, and contrast. Intra- and interobserver repeatability was assessed by calculating intraclass correlation coefficients (ICC) for all analysed parameters for 30 randomly selected cases (15 dislocators/15 controls).
Imaging evaluation of trochlear dysplasia
Trochlear dysplasia was assessed by using three standardised parameters, which are based on the results of Pfirrmann and coworkers [14] (Figs. 1 and 4). The first parameter, lateral trochlear inclination (LTI), is the angle formed between the plane of the subchondral bone of the lateral trochlea and the line connecting the two posterior femoral condyles. This parameter is measured in the most superior axial section showing trochlear cartilage. An angle <11° is defined as trochlear dysplasia. The second parameter is trochlear facet asymmetry (TFA) and is calculated as the ratio of medial trochlear facet width to lateral trochlear facet width. TFA is measured 3 cm above the joint space. A ratio of less than 0.4 is considered abnormal (i.e., the width of the medial facet is less than 40 % that of the lateral facet). Trochlear depth (TD) is the third parameter and refers to the depth of the trochlear groove relative to the medial and lateral trochlear facets. It is calculated as the mean of the lengths of the medial and lateral trochlear facets and subtracting the length of the trochlear groove. The lengths are measured relative to a line tangent to the posterior surfaces of the femoral condyles. According to Pfirrmann and coworkers, trochlear depth using a cutoff of 3 mm has 100 % sensitivity and 96 % specificity for trochlear dysplasia [14]. For our analysis, we therefore used a TD of less than 3 mm to classify a subject as positive for trochlear dysplasia. Intra- and interobserver repeatability was 0.855 and 0.843 for LTI, 0.87 and 0.887 for TFA, and 0.935 and 0.926 for TD.
Measurements for diagnosis of trochlear dysplasia. Trochlear depth is determined by calculating the mean of the lengths of the medial (a) and lateral (c) trochlear facets and subtracting the length of the trochlear groove (b): (a + c)/2—b. Facet asymmetry is the ratio of medial trochlear facet length (d) to lateral trochlear facet length (e) and is given as a percentage: d/e—100 %. Lateral trochlear inclination is defined as the angle formed between the plane of the subchondral bone of the lateral trochlea (f) and a tangential line through the posterior femoral condyles (g)
Imaging evaluation of patella alta
Patellar height for identification of patella alta was assessed using two parameters—the Insall-Salvati index (ISI) and the Caton-Deschamps index (CDI) (Figs. 2 and 4). The Insall-Salvati index describes the ratio of the length of the patellar tendon, measured from the apex of the patella to the tibial tuberosity, to the maximum superoinferior length of the patella; the ISI is determined from sagittal images on which both structures are clearly depicted [18]. Patella alta is assumed when the Insall-Salvati index is ≥1.3 [19]. The Caton-Deschamps index is determined by measuring the distance from the lower border of the patella to the tibial plateau and the length of the retropatellar surface articulating with the femur and calculating the ratio [20]. Patella alta is assumed for a Caton-Deschamps index of ≥1.2 [15]. Patellar height could not be evaluated in three patients with a chronically dislocated patella and three controls for whom no sagittal images were available. For the analysis of combinations of risk factors, patella alta was assumed to be present based on the results of the Caton-Deschamps index. Intra- and interobserver repeatabilities were 0.843 and 0.841 for ISI and 0.769 and 0.724 for CDI.
Measurement for diagnosis of patella alta. The Insall-Salvati index is calculated as the length of the patellar tendon from the patellar apex to the tibial tuberosity divided by the maximum superoinferior extent of the patella Patella (a/b). The Caton-Deschamps index is calculated as the length of the distance from the lower edge of the patella to the tibial plateau divided by the retropatellar surface: c/d
Imaging evaluation of TT-TG distance
Lateralisation of the patellofemoral force vector was evaluated by measuring the tibial tubercle-to-trochlear groove (TT-TG) distance using a method proposed by Schoettle et al. [21] (Figs. 3 and 4). The TT-TG is determined by the horizontal distance between the deepest point of the trochlear groove at the femur and the tibial tuberosity. In our analysis, a TT-TG distance >20 mm was classified as abnormal. Incomplete visualisation of the tibial tuberosity precluded analysis of the TT-TG distance in 14 patients and 13 controls. Intra- and interobserver variability for TT-TG was 0.754 and 0.834, respectively.
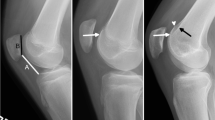
Patients after lateral patellar dislocation. MRI scans obtained in two patients immediately after lateral patellar dislocation. The first patient (upper panel) has trochlear dysplasia as the only risk factor, while patellar height and TT-TG distance are normal (TD 2 mm, CDI 1.18, TT-TG 14 mm). The second patient (lower panel) has marked trochlear dysplasia, a high-riding patella, and an abnormal TT-TG distance (TD 0 mm, CDI 1.5, TT-TG 23 mm)
Statistical analysis
Descriptive statistics of the study group and controls were calculated. Differences in mean age and risk factors between dislocators and controls were evaluated using Student’s t-test. The chi-square test was used to identify differences in sex distribution. Univariate analysis of variance (ANOVA) with Bonferroni corrections was performed to test differences between the subgroups of mechanisms of injury. Associations between the severity of a risk factor and the frequency of dislocations and associations between risk factors were quantified using Spearman correlation. Logistic regression analysis was performed to determine how the presence of the three risk factors investigated—trochlear dysplasia, patella alta, and abnormal TT-TG distance—affected the overall risk for patellar dislocation. The level of significance was set at 5 % (P < 0.05); values being significant at a 1 % level (P < 0.01) were defined as highly significant. Statistical analysis was performed using SPSS version 19.0 (Chicago, IL).
Results
Trochlear dysplasia
The mean values of the parameters determined to diagnose trochlear dysplasia—TFA, LTI, and TD—were significantly lower in dislocators compared with controls (31.9 %, 31.6 %, and 44.4 %, all P < 0.001) (Table 1). Using a cutoff of 3 mm, TD had 64.5 % sensitivity and 95.7 % specificity for LPD. Trochlear dysplasia was associated with a 36 times higher risk of LPD. With each 1-mm increase in trochlear depth, the risk of patellar dislocation decreased by a factor of 0.31 (odds ratio). Using TFA, 76 dislocators (40.9 %) and 6 controls (3.2 %) had trochlear dysplasia (42.5 % sensitivity, 96.2 % specificity). With LTI, 49 dislocators (26.3 %) and 2 controls (1.1 %) were positive for trochlear dysplasia (26.9 % sensitivity, 98.9 % specificity). Fifteen dislocators without trochlear dysplasia based on TD were positive for trochlear dysplasia when TFA was used. A significant difference in TD between men and women was only found for the control group (males 4.8 ± 0.1, females 4.3 ± 0.1, P = 0.006). There were no significant differences in mean values between acute and recurrent dislocators and no significant correlations between severity and the frequency of dislocations. There were no significant differences in mean values among the four subgroups of mechanisms of injury.
Patella alta
The mean Insall-Salvati and Caton-Deschamps indices were 13.8 % and 12.6 % higher in dislocators than in controls (both P < 0.001) (Table 1). The CDI had 59 % sensitivity and 74.9 % specificity for LPD (Table 2). When the ISI was used with a threshold of 1.3, 123 dislocators (66.1 %) and 63 controls (33.9 %) had patella alta (68.3 % sensitivity, 63.9 % specificity). Individuals with patella alta as the only risk factor had a 3.3-fold higher risk of patellar dislocation (CDI). Only with use of the ISI did we see a significant difference between men and women in the control group (men 1.17 ± 0.02, women 1.27 ± 0.02, P < 0.001). There were no significant differences between first-time and recurrent dislocators.
TT-TG distance
TT-TG distance was on average 48.5 % greater in dislocators compared with controls (P < 0.001) (Table 1). An abnormal TT-TG distance (>20 mm) was found in 29 dislocators (15.6 %) and 3 controls (1.6 %), a borderline TT-TG distance (15–20 mm) was observed in 49 dislocators (26.3 %) and 14 controls (7.5 %). In the dislocator group, TT-TG difference was significantly greater in men (men 15.7 ± 0.6, women 13.9 ± 0.6, P = 0.034). There were no significant differences between first-time and recurrent dislocators. A TT-TG distance >20 mm was associated with an 8.4 times higher risk of patellar dislocation.
Synopsis
An overview of the distribution of risk factors in dislocators presenting with trochlear dysplasia only and with trochlear dysplasia in combination with additional risk factors is presented in Fig. 5. Twenty-five individuals (14.8 %) of all dislocators had none of the three risk factors investigated. Forty-five patients (26.6 %) had trochlear dysplasia and no other risk factors. Twenty-six dislocators (15.4 %) had only patella alta, and two dislocators (1.2 %) had an abnormal TT-TG distance as the only risk factor. Sixty-one dislocators (36.1 %) had concomitant trochlear dysplasia and patella alta. With these two risk factors, there is an odds ratio of 41.4 for patellar dislocation. Six dislocators (3.6 %) had trochlear dysplasia and an abnormal TT-TG distance but no patella alta. Fifteen dislocators (8.9 %) had all three risk factors. In an individual with all three risk factors, there is a probability of 82 % that they have experienced prior patellar dislocation. In the control group, 123 subjects (72.4 %) had no anatomical risk factor, 44 subjects (25.9 %) had at least one risk factor, and 3 subjects (1.8 %) had two risk factors. No subject in the control group had all three risk factors.
Patterns of anatomical risk factors for patellar instability. Distribution of the three risk factors investigated among dislocators with trochlear dysplasia (n = 122, 66 %). Assessed risk factors were trochlear dysplasia (trochlear depth <3 mm), patella alta (Caton-Deschamps index >1.2), and increased TT-TG (>20 mm). Note that 64 (34 %) out of all dislocators (n = 186) had no trochlear dysplasia (not displayed in the diagram)
Discussion
The aim of our study was to systematically evaluate the effects of the three most relevant anatomical risk factors for the occurrence of lateral patellar dislocation using MRI and to compare the findings in dislocators to those of a control group. For all three risk factors, we found significant differences between dislocators and controls. Trochlear dysplasia was very common, affecting two thirds of those with a history of LPD, and was frequently combined with patella alta and occasionally with an abnormal TT-TG distance. Our results also suggest that there is no difference in the severity of risk factors between first-time and recurrent dislocators. Current orthopaedic treatment concepts attach great importance to a dedicated analysis of underlying risk factors, assigning a crucial role to MRI for assessing joint damage after patellar dislocation and analysing each patient’s underlying anatomical risk profile.
Several risk factors are assumed to contribute to patellofemoral instability; however, their precise aetiology is not yet fully understood. Current treatment approaches aim at addressing the individual patient’s underlying pathomechanism. MRI has an important role in that it not only provides an accurate diagnosis of dislocation and the damage caused by it but also allows quantitative assessment of the presence and severity of the most important anatomical risk factors [9]. The three parameters most commonly assessed are trochlear dysplasia, patella alta, and TT-TG distance [5].
In our study, approximately two thirds of the patients who underwent MRI after LPD had trochlear dysplasia, but also 4 % of the controls. Published data on the prevalence of trochlear dysplasia in patellar dislocators vary widely, which appears to be mainly attributable to the use of different measurement techniques. The role of a dysplastic trochlea in patellofemoral instability was mainly brought to attention by Caton et al.[20]. In this much-quoted study, 85 % of dislocators had trochlear dysplasia, which was defined as the presence of the so-called crossing sign and a trochlear depth of <4 mm. Comparison of our results with those of published MRI-based studies using a similar approach shows good agreement for the mean values of trochlear inclination, facet asymmetry, and trochlear depth [12, 13, 17]. Discrepancies in the prevalence of trochlear dysplasia may be attributable to differences in study populations with regard to the proportion of women, who have been reported to have more severe trochlear dysplasia [17]. Mild to moderate trochlear dysplasia in control subjects has also been reported by other investigators. Mean dysplasia parameters in control subjects in the studies of Pfirrmann et. al. and Carillon et al. are in very good agreement with our findings [11, 14]. Overall, the three parameters are highly reliable and specific, while sensitivity is only moderate. Differences in prevalences are attributable to the fact that trochlear dysplasia can have different manifestations, and with each parameter measuring different aspects of this abnormality, a borderline case on the basis of one parameter may be classified as normal or abnormal when the other parameters are used.
With regard to the diagnosis of patella alta, the results again depend on the imaging modality used and the measurement performed. Both the Insall-Salvati index, which was originally developed for conventional radiographs, and the Caton-Deschamps index show good reproducibility and can be derived from sagittal MR images with good agreement [19, 22, 23]. The Insall-Salvati index used to be the most common measure for assessing patellar height in the past [24]. In our study, use of the Insall-Salvati index with the generally accepted threshold of 1.3 identified patella alta in one third of the control group; we therefore used the Caton-Deschamps index for further analysis. With the latter, only a quarter of control subjects had patella alta. Overall, the Caton-Deschamps index had a slightly lower sensitivity but higher specificity for LPD, and hence it is the more conservative index. Measuring the CDI on conventional radiographs, Dejour et al. found patella alta in only 24 % of dislocators. In an MRI study, Escala et al. found 69.5 % sensitivity of patella alta for dislocation using a lower cutoff of 1.1 [13]. In another MRI study, Weber-Spickchen et al., using a cutoff of 1.2, diagnosed patella alta in 61 % of dislocators, which is in good agreement with our findings [15]. Overall, patella alta appears to contribute less to the risk of patellar instability compared with trochlear dysplasia [13].
An increase in the TT-TG distance contributes to patellar instability because it results in a larger lateral force vector on the patella. Several comparative studies have shown that a TT-TG distance of more than 20 mm is a significant risk factor for patellar dislocation [5, 10, 17, 25, 26]. However, there are considerable differences in reported prevalences of abnormal TT-TG in dislocators. In a small population, only 5 % of dislocators were found to have abnormal TT-TG [15], while a larger CT analysis performed by Dejour et al. identified abnormal TT-TG in 56 % of dislocators [5]. Differences are again predominantly attributable to differences in the study populations investigated, a significant factor being the sex distribution as women have higher TT-TG values after dislocation than men [10]; however, in our study, men had higher TT-TG values. While CT is the gold standard for measuring TT-TG distance, it is also possible to use MRI for this measurement [21]. Overall, an abnormal TT-TG distance appears to be a highly specific parameter for patellofemoral instability since our results and published data suggest that nondislocators have markedly lower mean TT-TG values of <13 mm and only rarely show abnormal values [5, 17, 27].
Our study has some limitations. Because of the retrospective design of our study, data on the number of prior dislocations or the mechanism of injury were not available in all cases. Therefore, it was not possible to perform all subgroup comparisons in all study subjects. Another limitation is that the examinations were performed on different MRI systems and with different coils. In some instances, there were also differences in the pulse sequences used. These factors might have led to slightly different measurement results. However, we believe that it is not possible to recruit a large enough population of patients who underwent imaging using the same MRI machine. The consensus reading performed in our study is another potential limitation.
In conclusion, our results suggest that patellar dislocators vary widely with regard to the presence, severity, and constellation of anatomical risk factors. Trochlear dysplasia appears to be the most important anatomical factor in LPD. Patellar dislocators may have trochlear dysplasia alone or in conjunction with patella alta and/or abnormal TT-TG distance, but they rarely have patella alta or abnormal TT-TG distance as the only risk factor. To identify an individual patient’s specific form of underlying patellofemoral instability, these three factors should be evaluated in a standardised manner.
References
Redziniak DE, Diduch DR, Mihalko WM et al (2009) Patellar instability. J Bone Joint Surg Am 91:2264–2275
Fithian DC, Paxton EW, Stone ML et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Vollnberg B, Koehlitz T, Jung T et al (2012) Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation. Eur Radiol 22:2347–2356
von Engelhardt LV, Raddatz M, Bouillon B et al (2010) How reliable is MRI in diagnosing cartilaginous lesions in patients with first and recurrent lateral patellar dislocations? BMC Musculoskelet Disord 11:149
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg Am 90:2751–2762
Mulford JS, Wakeley CJ, Eldridge JD (2007) Assessment and management of chronic patellofemoral instability. J Bone Joint Surg Br 89:709–716
White BJ, Sherman OH (2009) Patellofemoral instability. Bull NYU Hosp Jt Dis 67:22–29
Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics 30:961–981
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA (2000) Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology 216:582–585
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225:736–743
Escala JS, Mellado JM, Olona M, Gine J, Sauri A, Neyret P (2006) Objective patellar instability: MR-based quantitative assessment of potentially associated anatomical features. Knee Surg Sports Traumatol Arthrosc 14:264–272
Pfirrmann CW, Zanetti M, Romero J, Hodler J (2000) Femoral trochlear dysplasia: MR findings. Radiology 216:858–864
Weber-Spickschen TS, Spang J, Kohn L, Imhoff AB, Schottle PB (2011) The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: an MRI evaluation. Knee 18:185–188
Smith TO, Davies L, Toms AP, Hing CB, Donell ST (2011) The reliability and validity of radiological assessment for patellar instability. A systematic review and meta-analysis. Skeletal Radiol 40:399–414
Balcarek P, Jung K, Ammon J et al (2010) Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med 38:2320–2327
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104
Miller TT, Staron RB, Feldman F (1996) Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol 167:339–341
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Barnett AJ, Prentice M, Mandalia V, Wakeley CJ, Eldridge JD (2009) Patellar height measurement in trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 17:1412–1415
Seil R, Muller B, Georg T, Kohn D, Rupp S (2000) Reliability and interobserver variability in radiological patellar height ratios. Knee Surg Sports Traumatol Arthrosc 8:231–236
Insall J, Goldberg V, Salvati E (1972) Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res 88:67–69
Balcarek P, Ammon J, Frosch S et al (2010) Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy 26:926–935
Tsujimoto K, Kurosaka M, Yoshiya S, Mizuno K (2000) Radiographic and computed tomographic analysis of the position of the tibial tubercle in recurrent dislocation and subluxation of the patella. Am J Knee Surg 13:83–88
Pandit S, Frampton C, Stoddart J, Lynskey T (2011) Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: normal values for males and females. Int Orthop 35:1799–1803
Acknowledgements
Edzard Wiener and Gerd Diederichs contributed equally to this article.
Two additional research projects were carried out in subgroups of this cohort: (1) One subgroup of the cohort received additional scans for rotational alignment of the lower limb. The manuscript with the title “MRI analysis of rotational alignment in patients with patellar dislocation” is accepted for publication in the American Journal of Sports Medicine. (2) Another subgroup was analysed for cartilage defects. This article entitled “Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation” was already published in European Radiology (DOI 10.1007/s00330-012-2493-3).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Köhlitz, T., Scheffler, S., Jung, T. et al. Prevalence and patterns of anatomical risk factors in patients after patellar dislocation: a case control study using MRI. Eur Radiol 23, 1067–1074 (2013). https://doi.org/10.1007/s00330-012-2696-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2696-7