Abstract
Objective
To conduct a dose testing analysis of perfluorobutane microbubble (NC100100) contrast-enhanced ultrasound (CEUS) to determine the optimal dose for detection of liver metastases in patients with extra-hepatic primary malignancy.
Methods
157 patients were investigated with conventional US and CEUS. CEUS was performed following intravenous administration of perfluorobutane microbubbles (using one dose of either 0.008, 0.08, 0.12 or 0.36 μL/kg body weight). Three blinded off-site readers recorded the number and locations of metastatic lesions detected by US and CEUS. Contrast enhanced CT and MRI were used as the “Standard Of Reference” (SOR). Sensitivity, specificity and accuracy of liver metastasis detection with US versus CEUS, for each dose group were obtained. Dose group analysis was performed using the Chi-square test.
Results
165 metastases were present in 92 patients who each had 1–7 lesions present on the SOR. Sensitivity of US versus CEUS (for all doses combined) was 38% and 67% (p = 0.0001). The 0.12 dose group with CEUS (78%) had significantly higher sensitivity and accuracy (70%) compared to other dose groups (p < 0.05).
Conclusion
The diagnostic performance of CEUS is dose dependent with the 0.12 μL/kg NC100100 dose group showing the greatest sensitivity and accuracy in detection of liver metastases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The primary objective of this study is to determine the optimal concentration of NC100100 (Sonazoid®; Daiichi-Sankyo, Tokyo, Japan; GE Healthcare, Oslo, Norway) that provides the best diagnostic performance for detecting liver metastases. NC100100, a perfluorobutane microbubble ultrasound contrast agent (USCA) has a late hepatospecific phase of imaging (due to Kupffer cell uptake) that lasts up to 30 min [1–3]. Recent studies have shown that contrast enhanced ultrasound (CEUS) using NC100100 intravenous injection has greater sensitivity than conventional ultrasound (US) in detecting liver metastases [4–9]. However, as yet the optimal dose for diagnostic evaluation remains uncertain. Clearly, the performance of CEUS would benefit from selecting the most appropriate dose of contrast agent. In this study, 4 different doses of NC100100 (0.008, 0.08, 0.12, 0.36 μL/kg body weight) were used to assess the relationship of NC100100 dosage on sensitivity, specificity and accuracy of detection of liver metastases. The selected doses were determined based on data from a pre-existing unpublished phase II pilot study.
Materials and methods
Study population
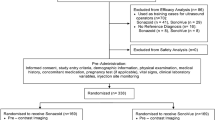
A prospective open-label phase III dose-finding study was conducted at 11 tertiary centres (9 in Europe and 2 in the USA) over a 10 month period. Local institutional review board and ethics committee approval was granted to participating institutions and written informed consent was obtained from all patients. The following inclusion criteria were used: 1) documented primary extra-hepatic malignancy, 2) age ≥18 years and 3) contrast enhanced CT and/or MRI performed in last 3 months. Exclusion criteria were: 1) NC100100 contraindication 2) medically unstable patient, 3) pulmonary hypertension, 4) unstable angina, 5) cardiac shunts and 5) pregnancy.
Injection procedure and dosage
NC100100 powder was reconstituted with 2 mL of sterile water and administered as a single IV bolus injection followed by a 10-mL saline flush. One of four doses (0.008, 0.08, 0.12, 0.36 μL suspension/kg body weight) was administered to each patient in accordance with a computer-generated randomization list. The readers and patients were blinded to the dose. Adverse events occurring up to 24 h post injection were recorded.
Ultrasound technique
US examinations were performed by sonographers with >5 years’ CEUS experience. Sonographers were blinded to the patient’s pre-existing clinical information. Philips HDI 5000 [Bothell, WA, USA], Siemens Elegra [Erlangen, Germany] and Acuson Sequoia [Erlangen, Germany]) ultrasound machines were used. The ultrasound protocol for both conventional US and CEUS was a standardized sequence of sweeps with different transducer orientations (transverse/sagittal/oblique) so as to evaluate the liver as completely as possible. All technical settings were optimised to achieve the best diagnostic results.
Conventional US examinations were performed using fundamental B-mode imaging. CEUS examinations were performed in the post vascular phase (late phase) at 5 min post injection using 2 settings; the first set of sweeps was obtained at low MI (0.3 to 0.4) with the focal zone set in the near-field (<5 cm) and the second set was acquired at intermediate MI (0.7 to 0.8) with the focal zone set in the far-field (10 cm). The first scan at low MI and near field focal zone was designed to detect superficial lesions, while the second scan at intermediate MI with a deeper focal zone was intended to detect deeper lesions.
US and CEUS studies for each patient were separately recorded as digital cine clip files. Patient details were masked and an identifying code number inserted for later blinded review.
For US, a lesion was considered a metastasis if it did not fulfil the sonographic criteria for either 1) a simple cyst (well-defined round or ovoid lesion with a uniform thin wall and anechoic fluid contents or 2) a typical haemangioma (well-defined, round or lobulated solid lesion with uniform increased echogenicity). For CEUS, a lesion was considered metastatic if it showed reduced enhancement (washout) (Figs. 1 and 2) and benign if it showed iso- or hyper-enhancement (Fig. 3), compared to the surrounding liver in the post vascular phase (late phase).
a. A 74-year-old man with a history of pulmonary cancer and radical prostatectomy for adenocarcinoma. (A) A hyperechoic (arrow) lesion is seen in segment VII on conventional US b. On the post vascular phase (late phase) CEUS, the lesion (arrow) shows hypoenhancement compared to normal adjacent liver parenchyma. This is consistent with a metastasis
a. A 54-year-old man with papillary cancer of the ureter. (A) No focal liver lesions are identified on conventional US. * relates to an intra-hepatic vessel. b. Post vascular phase (late phase) CEUS shows multiple hypoenhancing lesions consistent with metastases. Vessel (*) seen in (2A) is not seen in (2B)
a. A 62 year-old man with a history of lung cancer. (A) A hypoechoic lesion (arrowheads) is seen in segment VII on conventional US b. On the post vascular phase (late phase) CEUS, the lesion (arrowheads) shows hyperenhancement compared to the adjacent liver parenchyma. The lesion was considered to be a focal nodular hyperplasia based on the MRI pattern and the interval size stability on follow-up imaging
Standard of reference (SOR)
The SOR consisted of on-site combined readings of contrast enhanced CT and MRI by radiologists with at least 7 years’ experience. The imaging studies were assessed together with all available medical information. CT and MRI examinations were performed within 30 days before or after the US examinations.
Examinations met the following specifications:
-
1)
CT examinations included at least two post contrast phases acquired after administration of an iodinated contrast agent (2 mL/kg body weight, 350 mg/mL) at a rate of 3 mL/s. Arterial phase acquisition was performed 20–30 s post injection and portal phase at 60–70 s. Slice thickness was ≤5 mm and the pitch was adapted to cover the entire abdomen within a single breath-hold.
-
2)
MRI examinations included at least a T2-weighted spin-echo sequence, a T1-weighted spin-echo or gradient-echo sequence, and a dynamic T1-weighted gadolinium-enhanced study. Post-contrast arterial, portal and late phase acquisitions were performed. The slice thickness was set at <8 mm and the interslice gap was <20% of the slice thickness.
On all patients, the SOR assessment recorded 1) the number of liver lesions detected, 2) diagnosis for each detected lesion. Lesions were classified according to established imaging criteria (Table 1) [10, 11].
Patients were stratified into 3 groups depending on the number of liver lesions identified by the SOR: Group A (0 lesions), Group B (1 to 7 lesions) and Group C (more than 7 lesions). Only Group B was analysed as there were technical difficulties in analysing data from the other groups.
Safety assessment
Baseline assessments of medical history, concomitant medications, demographic information, and safety variables (symptoms, physical examination, blood and serum biochemistry and haematology, vital signs, 12-lead ECG, and pulse oximetry) were obtained. Vital signs, including ECG and pulse oximetry were assessed at 1 and 24 h post Sonazoid administration. All adverse events occurring up to 24-hour post injection were recorded.
Imaging analysis
Analysis was performed off-site by 3 blinded readers who independently evaluated the digital files of US and CEUS studies in a computer generated randomized fashion. Readers were instructed to localize lesions according to Couinaud’s classification and to estimate lesion diameter. All readers had more than 5 years’ CEUS experience.
Study end-point
The optimal dose of NC100100 was determined by analysing the sensitivity, specificity and accuracy of detection of liver metastases across dose groups.
Individual lesions on US and CEUS were classified as correctly detected only when they corresponded with lesions recorded by the SOR within the same anatomical segment. Lesions recorded with US or CEUS but not with the SOR were considered as false positives (Fig. 4). Lesions recorded with the SOR but not recorded in the US or CEUS were considered as false negatives. Lesions were classified as metastatic or benign.
Statistical analysis
Statistical analysis was performed using SPSS version 10.0 (SPSS Inc, Chicago, IL). The analysis was performed on the averaged results from the 3 independent blinded readers. Sensitivity, specificity and accuracy were calculated for detection of metastases. Comparison between dose-groups was performed using the Chi-square test and McNemar’s test (for differences between US and CEUS).
Results
Patient details are given in Table 2.
Of the 165 patients enrolled into the study, 2 were withdrawn before NC100100 administration: 1 before the beginning of the US examination on the subject’s own request and 1 by the investigator because of the large number of lesions noted on the US examination. The remaining 163 patients received NC100100. This comprised 94 males and 69 females (M: F = 1.4: 1). Their mean (SD) age was 62.4 (±11.7) years, age range 30–86 years and mean (SD) weight was 72.3 (±15.5) kg. The most common sites of primary cancer were the colon (n = 81), the breast (n = 11), the pancreas (n = 11), the lung (n = 10), and the kidney (n = 10).
Of the 163 patients who received NC100100, 7 were excluded because of protocol deviations: primary hepatocellular carcinoma (2 patients), absence of extra-hepatic cancer (1 patient), and no available SOR (4 patients). 59% of patients were assigned to Group B (i.e. had 1–7 liver lesions). Metastasis was the most common detected liver lesion, with a similar distribution across the dose groups (Table 2). The mean (SD) diameter of the lesions was 20.6 (19.7) mm (Table 2). The mean lesion size across dose groups was similar (Kruskal-Wallis test, p = 0.64).
Study end-point
Sensitivity, specificity and accuracy of conventional US and CEUS in the detection of liver metastases for the individual dose groups and all doses combined are summarized in Table 3.
CEUS produced a significant improvement compared to conventional US in the sensitivity of lesion detection for each dose group (p < 0.05) and for all doses combined (p < 0.0001). The 0.12 dose group produced the best results—sensitivity increased from 28% to 78%; and accuracy from 28% to 70%. The 0.12 dose group improvement was significantly higher compared to the other groups (p < 0.05). Compared with conventional US, the specificity of CEUS was greater in all dose groups combined (p > 0.01) but only the 0.008 dose group reached significance on its own (p = 0.045).
Analysis by lesion size
Regardless of lesion size, the sensitivity of CEUS was significantly greater than conventional US (p < 0.001) with the greatest improvement found for smaller lesions. For metastases <1 cm, 1–2 cm and >2 cm, the conventional US sensitivities were 16%, 31% and 65% respectively versus 58%, 66% and 88% respectively for CEUS (Table 4). Accuracy for lesions measuring <1 cm, 1–2 cm and >2 cm were 11%, 26% and 59% for conventional US and 36%, 54% and 80% for CEUS. The increase in accuracy from US to CEUS was significant for all lesion size categories (p < 0.001)
False positives
7, 7, 2 and 10 false positive results for metastases were detected on conventional US scans in the 0.008, 0.08, 0.12, and 0.36 dose groups, respectively. The number of false positives for CEUS was 6, 12, 7 and 8 in the 0.008, 0.08, 0.12 and 0.36 dose groups, respectively.
Safety
Twenty-three adverse events occurred with a similar frequency in the 0.008, 0.08 and 0.12 dose groups and marginally higher in the 0.36 dose group. These included pain at the cannula site (2), fever (1), sensation of temperature change (2), headache (4), hypertonia (1), diarrhoea (2), eructation (1), flatulence (1), nausea (2), prolonged QT (1), supraventricular tachycardia (1), skeletal pain (1), insomnia (1), coughing (1) and taste abnormality (1). 5 adverse events were judged as being related to the use of NC100100. These were pain at the cannula site, sensation of temperature change, diarrhoea, prolonged QT and taste abnormality. 4 of these events occurred in the 0.36 dose group, and 1 in the 0.08 dose group. All reported events were mild in intensity and resolved within the 24 h observation period.
Discussion
Compared to existing studies on NC100100 (Sonazoid®), this study is the largest in terms of patients (n = 157), metastases (n = 165) and participating centres (n = 11). This study highlights several important findings.
Firstly, CEUS using NC100100 improves the diagnostic evaluation of liver metastases. Irrespective of the dose used (0.008, 0.08, 0.12, 0.36 μL suspension/kg), sensitivity and specificity for detecting metastases were higher with CEUS than conventional US. Sugimoto K et al. (57 liver metastases) [8] and Luo W et al. (61 liver metastases) [9] performed CEUS exclusively in the post vascular phase (late phase). Sugimoto K et al. found that combined US imaging (US and CEUS) improved sensitivity for detection of metastases from 41.6% (US alone) to 72.2% (combined) as assessed by off-site reviewers. Luo W et al. found that CEUS had a sensitivity of 75% for the detection of liver metastases, similar to the 78% seen in our 0.12 dose group.
Secondly, this study confirms that the efficacy of CEUS is dose dependent. The 0.12 dose group was associated with the best results (78% sensitivity with 50% improvement compared to US; 70% accuracy and 42% improvement compared to US) and the 0.36 dose group with the least improvement (61% sensitivity with 17% improvement; 49% accuracy with 14% improvement compared to US). The dose-dependence is not unexpected: there is a minimum contrast differential between metastases and normal liver parenchyma below which detection is compromised, so the dose of contrast has to be sufficient. Conversely, if too much contrast is administered, shadowing from the contrast itself obscures lesions lying deep within the liver [12]. This may explain the variation in results for the different dose groups [Table 3] in the study. The 0.12 dose group associated with the greatest improvement in sensitivity (50%) was not associated with any improvement (0%) in specificity; this in itself may not be a practical concern. Whilst US is often used to facilitate the biopsy of indeterminate lesions, a significant proportion of these interventions fail as the lesions are occult on conventional US. In such cases, use of CEUS improves the detection of lesions for biopsy. Another important clinical application of NC100100 is the detection of metastatic lesions in real time; thereby facilitating US guided local ablative therapies such as radiofrequency ablation (RFA). Addition of USCAs improves the therapeutic capability of US guided RFA and other local ablative therapies by improving the sensitivity for detecting lesions [13].
Thirdly, CEUS markedly improved the detection of smaller metastases. The sensitivity for CEUS in the detection of lesions measuring <1 cm was 58% compared to 16% for US (all doses combined). In addition, for lesions measuring between 1–2 cm, the sensitivity for CEUS (66%) compared favourably to that of US (31%) (all doses combined).
The study suffers from several limitations.
The design of any blinded-reader study of US faces a major limitation compared with trials assessing the performance of CT or MRI. US is a real-time examination with no specific standardization of probe positioning. The field of view is limited by the sector sweep of the probe and there are few anatomical landmarks for reference, sometimes making it difficult to assign lesions accurately to Couinaud segments. Incorrect lesion assignment may have led to some true positive lesions on US or CEUS being erroneously labelled as false positive lesions on the SOR.
The variety of US equipment, transducer bandwidth, contrast-specific sequence and true acoustic output power used could have affected both US and CEUS acquisitions. This limitation is inherent to multi-centre studies.
The use of the blinded readers’ analysis of an imaging technique that is highly operator-dependent is likely to underestimate the actual lesion detection rate. Underestimation of the true performance of both US and CEUS by the blinded readers is therefore not surprising.
In this study neither arterial or portal phase enhancement of lesions was used to optimize lesion characterisation. This could have limited CEUS performance using NC100100 for hypervascular metastases (e.g. melanoma, thyroid, and neuroendocrine) that are optimally detected during the arterial phase.
Only rarely did the SOR include pathological diagnosis, introducing the possibility that apparent false positive results for CEUS may in fact represent a failure of CT or MRI to detect a true lesion. However, there are ethical and practical problems in carrying out biopsies for all lesions.
Conclusion
The diagnostic performance of CEUS using NC100100 in the detection of liver metastases is dose dependent. Of the 4 dose groups (0.008, 0.08, 0.12, 0.36 μL/kg body weight), the 0.12 group was associated with the highest sensitivity (78%) and accuracy (70%) and largest percentage improvement of these variables (50% and 42%) over conventional ultrasound (p < 0.05).
References
Yanagisawa K, Moriyasu F, Miyahara T et al (2007) Phagocytosis of ultrasound contrast agent microbubbles by Kupffer cells. Ultrasound Med Biol 33:318–325
Kindberg GM, Tolleshaug H, Roos N et al (2003) Hepatic clearance of Sonazoid perfluorobutane microbubbles by Kupffer cells does not reduce the ability of the liver to phagocytose or degrade albumin microspheres. Cell Tissue Res 312:49–54
Watanabe R, Matsumura M, Munemasa T et al (2007) Mechanism of hepatic parenchyma specific contrast of microbubble based contrast agent for ultrasonography: microscopic studies in rat liver. Invest Radiol 42:643–651
Nakano H, Ishida Y, Hatakeyama T et al (2008) Contrast-enhanced intraoperative ultrasonography equipped with late Kupffer-phase image obtained by sonazoid in patients with colorectal liver metastases. World J Gastroenterol 14:3207–3211
Sugimoto K, Shiraishi J, Moriyasu F et al (2009) Computer-aided diagnosis of focal liver lesions by use of physicians’ subjective classification of echogenic patterns in baseline and contrast-enhanced ultrasonography. Acad Radiol 16:401–411
Luo W, Numata K, Morimoto M et al (2009) Focal liver tumours: Characterization with 3D perflubutane microbubble contrast agent enhanced US versus 3D contrast enhanced multidetector CT. Radiology 251:287–295
Hatanaka K, Kudo M, Minami Y et al (2008) Differential diagnosis of hepatic tumours: Value of contrast enhanced harmonic sonography using the newly developed contrast agent, Sonazoid. Intervirology Suppl 51:61–69
Sugimoto K, Shiraishi J, Moriyasu F et al (2009) Improved detection of hepatic metastases with contrast-enhanced low mechanical-index pulse inversion ultrasonography during the liver-specific phase of sonazoid: observer performance study with JAFROC analysis. Acad Radiol 16:798–809
Luo W, Numata K, Kondo M et al (2009) Sonazoid-enhanced ultrasonography for evaluation of the enhancement patterns of focal liver tumours in the late phase by intermittent imaging with a high mechanical index. J Ultrasound Med 28:439–48
Nino-Murcia M, Olcott EW, Jeffrey RB Jr et al (2000) Focal liver lesions: pattern-based classification scheme for enhancement at arterial phase CT. Radiology 215:746–51
Elsayes KM, Narra VR, Yuming Y et al (2005) Diagnostic value of enhancement pattern approach with contrast enhanced 3D gradient echo MR imaging. Radiographics 25:1299–1320
Edey AJ, Ryan SM, Beese RC et al (2008) Ultrasound imaging of liver metastases in the delayed parenchymal phase following administration of Sonazoid using a destructive mode technique (Agent Detection Imaging). Clin Radiol 63:1112–20
Leen E, Kumar S, Khan SA et al (2009) Contrast-enhanced 3D ultrasound in the radiofrequency ablation of liver tumours. World J Gastroenterol 15:289–99
Acknowledgement
This study was supported by a grant from Amersham AG, Oslo, Norway.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Correas, JM., Low, G., Needleman, L. et al. Contrast enhanced ultrasound in the detection of liver metastases: a prospective multi-centre dose testing study using a perfluorobutane microbubble contrast agent (NC100100). Eur Radiol 21, 1739–1746 (2011). https://doi.org/10.1007/s00330-011-2114-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2114-6