Abstract
We report a new lateral approach for ultrasound visualization of the distal biceps tendon. A cadaver specimen was dissected to study distal biceps anatomy relevant to this approach. Sonograms obtained in volunteers and patients are provided to illustrate this alternative method.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The distal biceps tendon may be affected by diverse pathologic conditions such as rupture, tendinosis, and bursitis. Ruptures are clinically important since early surgical reattachment to the radial tuberosity is recommended [1]. Ultrasound is an excellent tool to identify complete tears, assess tendon retraction, and provide a grading of the tear [2, 3]. Magnetic resonance (MR) imaging also provides diagnostic imaging of the elbow allowing diagnosis of biceps tears [4]. MR imaging is more time consuming, and in our experience precise assessment of the grade of injury may remain difficult with this method [5]. The biceps tendon is typically examined from an anterior approach [6]. This often results in difficulty to obtain diagnostic images of the distal part of the tendon and the insertion on the radius. This problem is related to the course of the distal part of the biceps in the depth away from the transducer [6, 7]. Alternative approaches with ultrasound have been described [2]. In this report we present a different alternative method to investigate the distal part of the biceps from a lateral approach. We found this approach helpful and easy to perform in clinical practice. This approach is somewhat similar to an alternative MR approach that was previously reported [4]. We dissected a cadaveric specimen to study the distal biceps and demonstrate its relationship with adjacent musculature. Sonograms obtained in volunteers and patients are provided to further illustrate this lateral approach. IRB approval was obtained for the study.
Anatomic considerations
The distal biceps tendon forms from a fibrous band in the distal aspect of the biceps muscle. The lateral portion of the fibrous band forms the biceps tendon, whereas the medial portion forms the lacertus fibrosus (Figs. 1 and 2) [8]. The lacertus fibrosus inserts on the superficial fascia at the level of the antecubital fossa. The lacertus fibrosus is a strong fibrous band that can limit retraction of the biceps muscle even with complete tears of the distal biceps tendon. The biceps tendon proper courses into the depth adjacent to the brachial artery. It becomes located deep and medial to the extensor musculature of the forearm. A few centimeters before the radial insertion, the biceps becomes located medially to the supinator muscle belly. The radial insertion is in a medial position with pronation of the forearm, but assumes a more anterior position with supination of the forearm. The brachioradial bursa is located in between the distal biceps tendon and the radius.
Line drawing of elbow showing anterior view and cross-sectional view of biceps tendon insertion area. Note biceps muscle forming medially directed lacertus fibrosus (black arrow), and distal biceps tendon insertion (white arrow). Lateral to biceps insertion supinator muscle (S) and extensor muscle (E) are seen. Note transducer position (rectangle, T)
Ultrasound of the distal biceps tendon
With the classic anterior approach the ultrasound transducer is placed above the antecubital fossa in the transverse plane. The biceps muscle is then followed inferiorly and the biceps tendon can then be accurately identified. Once the biceps tendon is identified the probe can be turned in the sagittal plane (Fig. 3). An initial transverse approach is recommended since it may be difficult to identify the correct location of the biceps in the sagittal plane. It is also recommended to start the examination somewhat above the level of the elbow joint, over the distal portion of the biceps muscle. A fibrous hyperechoic intramuscular band that forms the biceps tendon can be clearly identified. When displacing the transducer distally, the fibrous band gradually turns into the biceps tendon proper. The biceps tendon can be followed distally where it courses in the depth. Visualization of the distal portion is important since most biceps ruptures occur in this region. Typically the distal portion is hard to depict, and even when it is seen, refraction and anisotropy artifacts are so prominent that assessment is difficult. Anisotropy represents a change in echogenicity of the tendon due to changes in inclination of the probe. When the probe is not perpendicular the tendon tends to become hypoechoic and more difficult to assess. Some ultrasound machines can steer the ultrasound beam along the long axis of the transducer, which may reduce anisotropy. From the transverse plane the probe can be gently repositioned into the sagittal plane; however, the same limitation regarding visualization of the distal portion remains (Fig. 3).
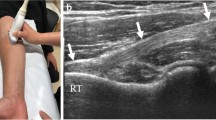
The approach for lateral visualization includes positioning of the forearm in supination and 90° of flexion. The biceps tendon becomes taut secondary to the supination and is palpable at the anterior aspect of the elbow. The insertion of the biceps on the radius will be situated in the same coronal plane as that in which the distal biceps can be palpated in the above-described arm position. The transducer is thus placed in the coronal plane on the lateral aspect of the elbow. From this position the extensor muscle belly, the supinator muscle belly, and the radius can be easily identified (Figs. 4–6). The distal part of the biceps and the insertion on the radius can be depicted with this approach. The prominent refraction and anisotropy artifacts occurring with an anterior approach are entirely absent given that the transducer is now parallel to the biceps tendon. The only limitation consists in a small area of refraction artifact at the edge of the supinator muscle (Fig. 6). The most distal few millimeters of the biceps insertion are also more difficult to depict due to interposition of the radius. This artifact, however, can be corrected for by slightly decreasing the degree of supination. A dynamic study of the biceps is also possible in this position by pronating and supinating the forearm, and assessing continuity of tendon fibers in real time. This can confirm continuity of the tendon and this maneuver cannot be accomplished with the anterior approach.
Reconstructed CT image illustrating image obtained by lateral approach (compare with Figs. 6 and 7). Note lateral extensor muscle (E), supinator muscle (S) adjacent to radius, and biceps tendon insertion (arrows) on radius (R) (image is rotated so that lateral is at top of image, and anterior is on left side of image)
The lateral approach may provide information that is difficult to obtain by the anterior approach. We illustrate the use of our technique in two patients with a clinical suspicion of distal biceps tendon tears (Figs. 7 and 8).
A 45-year-old man with clinical suspicion of biceps tear. a Anterior ultrasound shows apparently normal biceps tendon (arrows). Distal insertion site cannot be seen. b Lateral ultrasound shows reactive fluid in bicipitoradial bursa (arrowheads) adjacent to the tendon insertion (arrows). Extensor muscle (E), supinator muscle (S), radius (R)
A 25-year-old man with clinical suspicion of distal biceps tear. a Anterior ultrasound shows fibers discontinuity (asterisk) at musculotendinous junction of biceps (B) corresponding to complete tear. b Lateral view shows complete absence of biceps tendon (arrows) with proximal stump significantly retracted from insertion site. Extensor muscle (E), supinator muscle (S), radius (R)
In conclusion, we discuss a lateral approach for ultrasound visualization of the distal biceps insertion. This method can be considered as an adjunct to the anterior approach, and helps to visualize the more distal aspect of the tendon which may be more difficult with the anterior approach.
References
El Hawary R, Macdermid JC, Faber KJ, Patterson SD, King GJ (2003) Distal biceps tendon repair: comparison of surgical techniques. J Hand Surg Am 28:496–502
Kayser R, Mahlfeld K, Scheller W, Muller J, Schmidt W, Jeyde CE (2005) Sonographic imaging of the distal biceps tendon—an experimental and clinical study. Ultraschall Med 26:17–23
Weiss C, Mittelmeier M, Gruber G (2000) Do we need MR images for diagnosing tendon ruptures of the distal biceps brachii? The value of ultrasonographic imaging. Ultraschall Med 21:284–286
Giuffre BM, Moss MJ (2004) Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol 182:944–946
Chew ML, Giuffri BM (2005) Disorders of the distal biceps brachii tendon. Radiographics 25:1227–1237
Miller TT, Adler RS (2000) Sonography of tears of the distal biceps tendon. AJR Am J Roentgenol 175:1081–1086
Belli P, Constantini M, Mirk P, Leone A, Pastore G, Marano P (2001) Sonographic diagnosis of distal biceps tendon rupture: a prospective study of 25 cases. J Ultrasound Med 20:587–595
Athwal GS, Steinman SP, Rispoli DM (2007) The distal biceps tendon: footprint and relevant clinical anatomy. J Hand Surg Am 32:1225–1229
Acknowledgement
We thank Anna Browning. Illustrator, University of Michigan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalume Brigido, M., De Maeseneer, M., Jacobson, J.A. et al. Improved visualization of the radial insertion of the biceps tendon at ultrasound with a lateral approach. Eur Radiol 19, 1817–1821 (2009). https://doi.org/10.1007/s00330-009-1321-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1321-x