Abstract
We evaluated an MRI protocol at 3 T for the assessment of morphological and functional properties of the common carotid artery (CCA) in 32 healthy volunteers and 20 patients with high-grade internal carotid artery stenosis. Wall thickness of the CCA was measured by using multislice 2D T2 dark blood fast spin echo sequences and compared with intima-media thickness (IMT) determined by ultrasound. Carotid distensibility coefficient (DC) quantified by blood pressure and CCA diameter change during the cardiac cycle was measured by ECG gated 3D T1 CINE MRI and M-mode ultrasound. Apart from generally higher values in MRI high agreement was found for wall thickness and compliance in volunteers and patients. Remaining differences between both methods may be attributed to slightly different methods for measuring IMT and DC. Our findings indicate that MRI at 3 T is a feasible and promising tool for the comprehensive assessment of normal carotid geometry and function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Increased carotid intima-media thickness (IMT) reflects morphological changes associated with atherosclerosis and is a strong predictor for future clinical cardiovascular events [1]. The most reliable parameter for the assessment of carotid stiffness is the distensibility coefficient (DC) which can be calculated by considering the maximum diameter change over the cardiac cycle and central blood pressure [2]. DC was strongly associated with atherosclerosis at various sites in the vascular tree [3]. In particular, the combination of DC with IMT was valuable for the comprehensive analysis of the individual atherosclerotic burden and improved prediction of aortic atherosclerosis [4]. Although both parameters can be easily obtained by high-resolution ultrasound, this technique is limited by its observer-dependency, two-dimensional nature of data and only rough plaque characterization.
Owing to its intrinsic high soft tissue contrast, MRI is increasingly used for the detailed analysis of internal carotid artery (ICA) plaques [5, 6]. Moreover, numerous MRI studies of carotid artery wall thickness and distensibility based on 2D imaging with submillimetre spatial resolution revealed good agreement with ultrasound and allowed for the diagnosis of atherosclerosis at an early stage [7–12]. While one 3D T1-weighted fast spin echo (FSE) black blood MR technique resulted in improved visualization of small plaque components of ICA stenosis but reduced reliability for image quality [13], excellent reliability was demonstrated in another 3D study using black blood balanced steady state free precession (SSFP) for the evaluation of wall thickness [14]. Furthermore, semiautomated or automated data analysis tools improved reproducibility and accelerated vessel wall analysis [15, 16]. Such MRI studies showed similar repeatability for the assessment of carotid wall thickness and small differences compared with ultrasound, most probably due to the inclusion of the adventitia by MRI [17]. Similarly, a recent study reported high reproducibility of carotid wall and area measurements at 3 T [18].
In contrast to these previous studies, our MRI protocol provided a combined assessment of both carotid wall thickness and distensibility at 3 T. The time-resolved cine 3D T1-weighted MRI applied here allowed us to optimally evaluate the carotid arteries with multiplanar reformats placed orthogonally to the vessel wall thereby reducing partial volume effects. In addition, common carotid artery haemodynamics were monitored and wall thickness and compliance in MRI were measured analogously to ultrasound in order to provide optimal comparability in a larger cohort of volunteers and patients with high-grade ICA stenosis.
Materials and methods
Subject population
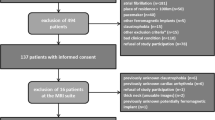
Thirty-two healthy volunteers and 20 patients with high-grade internal carotid artery (ICA) stenoses were prospectively included. Mean age of the 32 healthy volunteers was 25.1 ± 3.1 years and 17 (53.1%) were female. Fifteen patients underwent carotid endarterectomy, four patients underwent stent angioplasty and one patient did not receive recanalization therapy. The study was approved by the local ethics committee and written informed consent was obtained from all participants. Cardiovascular risk factors were prospectively documented and defined as previously described [19]. In the healthy volunteer group only subjects without cardiovascular risk factors, history of cardiovascular events and without inflammatory vessel disease were included. In addition, subjects with blood pressure during MR measurement exceeding 140 mmHg or 95 mmHg in systole or diastole, respectively, were excluded. All expert readers of ultrasound and MRI data were blinded to the complementary imaging modalities as well as to the individual patient’s demographic data.
Monitoring of haemodynamic conditions
Ultrasound and MRI measurements were performed on the same day in order to achieve optimal comparability of both methods. Haemodynamic baseline conditions were monitored in all participants of this study with subjects in a supine position. During ultrasound, heart rate and arterial oxygen saturation (%) were measured by optical pulse oximetry. Systolic and diastolic arterial blood pressure (ABP) were evaluated with a standard oscillometric technique by applying a cuff to the patient’s upper right arm (Dinamap plus, Criticon, Tampa, USA). Identical parameters were monitored during MRI examination (Millennia 315MVS, Invivo Research Inc, Orlando, USA). After establishing stable values during rest for 10 min, measurements were started. Parameters were recorded in 5-min intervals and averaged for the comparison of ultrasound and MRI.
B-mode ultrasound
Carotid intima-media thickness
Carotid arteries were assessed with a 7- to 12-MHz linear-array probe (Logiq 7, GE Healthcare, USA) by one trained sonographer. Accordingly, spatial resolution of the ultrasound probe for the examination of the common carotid artery was 0.30 mm. This is significantly higher compared with ultrasound used in clinical routine (5-MHz probe, spatial resolution ca. 0.5 mm) and enables improved accuracy for the measurement of wall thickness and vessel diameter [20]. Measurements were performed in a supine position with the head of the subjects turned by 45° to the contralateral side. As a result, optimal anterolateral longitudinal views of the right and left CCA were obtained with a clear delineation of the far wall (related to the ultrasound probe) over a minimum distance of 3 cm. Accordingly, the dorsomedial wall of the CCA was examined in all subjects. Images were triggered using the R wave of the ECG. IMT was measured at four locations of the far wall. Thickness was quantified on both sides of the CCA at a plaque-free location 2 cm proximal to the carotid bifurcation (Figs. 1a–c, 2a and b). For comparison with MRI values of mean IMT of both CCA were considered.
Measurement of intima-media thickness (IMT) and wall thickness in one volunteer. Ultrasound (top): Overview of the carotid bifurcation indicating the location of IMT measurement 2 cm proximal to the bifurcation (a). Longitudinal view (b) and magnification (c) of the left CCA for the calculation of IMT. Normal IMT was measured by electronic calipers (yellow arrows) at the far wall of the CCA (related to the ultrasound probe). MRI (bottom): Time-of-flight angiography (d) was used to determine axial slides in T2-weighted imaging 2 cm distal to the bifurcation (e). Analogously, the dorsomedial wall was measured in magnification (f) by electronic calipers (yellow arrows). Image quality for both techniques was graded excellent. ICA internal carotid artery, ECA external carotid artery, IJV internal jugular vein
Measurement of the carotid wall thickness in a 76-year-old patient. Ultrasound (top): Overview of the common carotid artery (CCA) in longitudinal view (a), and in magnification (b) for the calculation of IMT of the left CCA as performed in the healthy volunteer in Fig. 1. The IMT of the far wall is significantly increased (yellow arrows). MRI (bottom): Time-of-flight angiography indicates the measurement site 2 cm proximal to the bifurcation (c). Axial overview of the neck (d) and measurement of carotid wall thickness at the dorsomedial wall in magnification using electronic calipers (yellow arrows) (e). Similar to ultrasound, a significantly increased wall thickness can be appreciated. Image quality for both techniques was graded excellent. ICA internal carotid artery, ECA external carotid artery, IJV internal jugular vein
Carotid compliance
CCA stiffness was determined in M-mode by assessing the maximal change in diameter during systole and diastole (Fig. 3a) as described in a previous study [4] and expressed by the distensibility coefficient:
where Δd is the change in diameter, Dd the end diastolic diameter and ΔP the pulse pressure. Pulse pressure (ΔP) was calculated as the difference between maximal systolic and diastolic blood pressures derived from the average of six measurements. Measurements were performed 2 cm proximal to the carotid bifurcation of the right and left CCA at a plaque-free site and mean values of both sides were used for further analysis.
Measurement of diameter change of the CCA during the cardiac cycle in one volunteer by ultrasound and MRI. Ultrasound (top): After an optimal axial image of the CCA was obtained diameter change was determined by M-mode ultrasound 2 cm proximal to the bifurcation. Maximum systolic and end diastolic diameter were measured manually (a). MRI (bottom): Reconstructed longitudinal view of the carotid bifurcation based on reformatted 3D T1 CINE images (b) and the perpendicular longitudinal axis (c) allowed for precise angulation and generation of axial planes 2 cm proximal to the bifurcation (d and e). Minimum and maximum vessel area during end diastole (d) and early systole (e) were identified by manually outlining the vessel lumen contours. Image quality for both techniques was graded excellent. ICA internal carotid artery, ECA external carotid artery
MRI
MRI measurements were performed on a routine 3 T MRI system (TIM TRIO, Siemens, Erlangen, Germany) using a combined 12-element head and six-element neck coil.
Initially, time-of-flight (TOF) angiography covering the carotid arteries on both sides was performed to determine the exact location of the left and right bifurcation (voxel size 0.8 × 0.5 × 1.0 mm3, field of view (FOV) 176 × 200 mm2, echo time (TE)/repetition time (TR) 3.69 ms/20 ms, flip angle 25°, bandwidth 250 Hz/pixel). For patients, additional CE-MRA was performed after injection of 0.1 mmol/kg body weight Gadolinium-based contrast agent (gadobenate dimeglumine, Multihance, Bracco, Italy) at 3.5 mL/s (voxel size 0.8 × 0.6 × 0.7 mm3, FOV 225 × 300 mm2, TE/TR 1.31 ms/3.11 ms, flip angle 20°, bandwidth 650 Hz/pixel. TOF or CE-MRA data were used to position an axial 3D volume for T1 3D CINE imaging and 2D dark blood T2 imaging covering the CCA and carotid bifurcation of both sides.
3D T1 CINE imaging based on rf-spoiled gradient echo acquisition was performed using prospective ECG gating and the following parameters: temporal resolution 73.6 ms, voxel size 0.9 × 0.7 × 0.8 mm3, FOV 176 × 220 mm2, TE/TR 1.872 ms/3.8 ms, flip angle 15°, bandwidth 450 Hz/pixel. 2D T2-weighted images based on fast spin echo acquisitions were acquired in multislice mode (20 slices) with in-plane pixel size 0.4 × 0.4 mm2, slice thickness 3 mm, FOV 176 × 220 mm2, TE/TR 89 ms/5,230 ms, refocusing flip angle 140°, bandwidth 202 Hz/pixel. Carotid wall thickness was measured using T2-weighted imaging with the black blood technique in order to allow clear differentiation of the arterial wall. Dark blood contrast was achieved by the long echo time (outflow effect) and additional saturation slabs above and below the 2D slice package.
MRI vessel wall analysis was performed using a multiplanar reformating tool (J-Vision, Tiani Medgraph AG, Innsbruck, Austria) to navigate within the reconstructed 3D or multislice 2D data and generate planes normal to the CCA 1 cm proximal to the ICA bulb of each side. In subjects without clear delineation of the bulb, measurements were performed 2 cm proximal to the carotid bifurcation (Fig. 1d). For precise identification of the exact location of individual analysis planes the localizer function within the maximum intensity projection (MIP) of the arterial phase of the TOF angiography in volunteers or the CE-MR angiography in patients was used (Fig. 1d).
In volunteers both 2D T2 and 3D T1 CINE sequences were acquired. As a result of the relatively long data acquisition times, only some of the acutely ill patients tolerated the 3D T1 CINE sequences used for the determination of carotid compliance.
MR imaging was assessed by two experienced readers, one neurologist with 8 years of experience in vascular ultrasound and 4 years of experience in vascular MRI, and one physician with more than 3 years of experience in vascular MRI.
Carotid arterial wall thickness
In order to ensure comparable measurements in MRI, axial slices in T2-weighted imaging were divided into four areas of equal size as outlined by one anterior-posterior and a second perpendicular line. In concordance with ultrasound, the dorsomedial quarter was chosen for measurements. Determination of wall thickness was performed by manually positioning electronic calipers in the transverse view (Figs. 1f, 2e). At a plaque-free site the distance between the external vessel wall border and the border between the vessel wall and the hypointense lumen was recorded at two sites in two slice locations for each CCA. As a result, eight values of CCA vessel wall thickness were obtained per subject.
Carotid compliance
Carotid compliance was measured using T1 3D CINE MRI with the imaging volume covering the CCA of both sides. Data were transferred to a commercially available software package (AquariusNet, TeraRecon, San Mateo, USA) permitting interactive definition and angulation of 2D analysis planes within the 3D volume which was oriented perpendicular to the vessel segment of interest (Fig. 3b, c). Maximum and minimum lumen area during systole and diastole were determined by using manually drawn regions on the MRI images for each of the 12–15 time points during the cardiac cycle (Fig. 3d, e). Mean diameter (d) in systole and diastole was calculated individually as \(d = 2 \times \sqrt {\left( {{A \mathord{\left/ {\vphantom {A \pi }} \right. \kern-\nulldelimiterspace} \pi }} \right)} \) (mm) where A is the vessel lumen area. Calculation of DC was performed analogously to ultrasound.
Grading of image quality
Quality of T2-weigthed 3D T1 CINE MRI and 2D Duplex sonography images was graded as follows: low, i.e. vessel wall not visible due to severe blurring; moderate, i.e. blurring, but vessel wall measurable with a sufficient level of confidence; good, i.e. only slight blurring, entire vessel wall visible; excellent, i.e. no blurring, excellent visibility of the complete vessel wall. Images with low image quality were excluded from analysis.
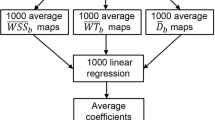
Statistical analysis
MRI imaging including haemodynamic data acquisition was repeated in ten volunteers (i.e. 20 common carotid arteries) in order to enable one to assess reproducibility and intra- and interobserver agreement in terms of wall thickness and compliance measurements. The 95% confidence intervals (95%CI) were calculated as plus or minus two standard deviations. To detect statistically significant differences between continuous variables, paired t tests were applied. The comparison between ultrasound and MRI measurements regarding carotid wall thickness and stiffness were evaluated by the approach of Bland and Altman [21] by calculating the mean (d) and SD (ς d ) of the difference. From these data, the limits of agreements (d − 2ςd and d + 2ςd) were calculated. All significance tests were two-sided and used a significance level of 5%. All analyses were performed by using the SPSS statistical package (Version 15.0).
Results
Baseline characteristics
In all 32 volunteers and 20 patients IMT was measured by both ultrasound and MRI. In all volunteers but in only seven patients carotid compliance was measured by MRI due to limited patient cooperation. Baseline data of the 20 patients are given in Table 1.
Image quality
MRI
2D T2 imaging was performed in all 52 subjects and quality was graded low in 5 (9.6%), moderate in 7 (13.5%), good in 18 (34.6%) and excellent in 22 patients (42.3%). 3D T1 CINE sequences were performed in 39 subjects and quality was graded low in 1 (2.6%), moderate in 2 (5.1%), good in 9 (23.1%) and excellent in 27 patients (69.2%).
Ultrasound
Quality for the determination of carotid IMT was graded moderate in 4 (7.7%), good in 3 (5.8%) and excellent in 45 subjects (86.5%). Image quality was graded low in none of the patients. As a result, wall thickness of 47 (90.4%) and compliance of 38 subjects (73.1%) was available for comparison of MRI and ultrasound.
CCA wall thickness and compliance in ultrasound and MRI
Ultrasound and MRI data of all subjects are given in Tables 2 and 3. Wall thickness measured by MRI was significantly higher than that obtained using ultrasound (p < 0.01). This difference was more pronounced in healthy volunteers than patients. For seven patients, the values of carotid distensibility determined using MRI were considerably higher than those measured by ultrasound. However, excellent agreement of both techniques was observed for DC in the 32 healthy volunteers. These findings are confirmed by the limits of agreement given in the Bland–Altman plots in Figs. 4 and 5. With increasing wall thickness, i.e. in patients, discrepancies between ultrasound (US) and MRI increased without indication of a systematic error (Fig. 5a). For the distensibility coefficient, there was a trend of MRI to underestimate US measurements without indication of a systematic error.
Comparison of common carotid artery (CCA) wall thickness determined by ultrasound (US) and MRI. a Bland–Altman plot of mean values of intima-media thickness (IMT) determined by ultrasound versus wall thickness determined by MRI for all subjects assessable (n = 47). Black dots represent volunteers, red dots represent patients. Mean of difference was 0.02 mm, SD of difference was 0.01 mm and limits of agreements were mean −1.96 × SD = −0.01 mm and mean +1.96 × SD = 0.05 mm. b Box plots indicate higher values of wall thickness determined by MRI compared with ultrasound (p < 0.001)
Comparison of common carotid (CCA) distensibility coefficient (DC) measured by MRI and ultrasound (US) and MRI. a Bland–Altman plot of mean intima-media thickness (IMT) determined by ultrasound versus mean wall/plaque thickness determined by MRI for all subjects assessable by both methods (n = 38). Black dots represent volunteers (n = 31), red dots represent patients (n = 7). Mean of difference was 2.3, SD of difference was 9.1 mm and limits of agreements were mean −1.96 × SD = 15.4 and mean +1.96 × SD = 20.0 (10−3/kPa). b Box plots show that there was no significant difference of DC measurement between both techniques (for all patients assessable)
Reproducibility and intra- and interobserver agreement
For MRI measurements of wall thickness confidence intervals for reproducibility and intra- and interobserver agreement were mean 0.056, 95%CI −0.004 to 0.004 cm; mean 0.055, 95%CI −0.004 to 0.004 cm; mean 0.055, 95% CI −0.006 to 0.006 cm, respectively. For the calculation of distensibility coefficient using MRI, confidence intervals for reproducibility and intra- and interobserver agreement were mean 39.3, 95%CI −15.8 to 15.8; mean 39.0, 95%CI −12.6 to 12.6; mean 40.2, 95%CI −16.6 to 16.6 10−3/kPa, respectively.
Discussion
The results of this study demonstrate the feasibility of wall thickness measurements in both volunteers and patients with advanced stages of atherosclerosis, i.e. high-grade ICA stenosis, by high-resolution 2D dark blood T2-weighted MRI at 3 T. In comparison to previous MRI studies investigating the wall properties of the CCA [10, 13, 15–17] we additionally provide data on carotid artery compliance. In particular, we took the potential influence of haemodynamic conditions such as pulse pressure on both ultrasound and MRI measurements into account as these affect the calculation of the distensibility coefficient. We observed high concordance of MRI and ultrasound for the determination of vessel compliance in healthy volunteers. In the small group of patients available for additional compliance measurement by MRI, however, correlation with ultrasound was limited although haemodynamic parameters were not significantly different between measurements. We speculate that the currently limited accuracy may be related to the small number of patients investigated and the limited cooperation compared with the much younger volunteers. This may have resulted in artefacts induced by swallowing and head movements during the relatively long 3D T1 CINE measurements. Thus, navigator gating for the compensation of swallowing, as presented by Crowe et al. [22], could be helpful to reduce image artefacts in future patient studies. As a result of the small subgroup of patients available for carotid compliance measurements the statistical relevance of the results presented here is limited. Findings demonstrate the feasibility of this technique in patients with progressive carotid atherosclerosis. Future studies evaluating carotid compliance by using 3D CINE T1 in larger cohorts of patients are required to test the feasibility and accuracy of this method for clinical routine.
Similar to previous studies we observed higher values of wall thickness determined by MRI compared with intima-media thickness determined by ultrasound. We obtained excellent values for intra- and interobserver agreement and reproducibility of MRI measurements. Thus, differences compared with ultrasound are especially due to the inclusion of the adventitia in the MRI measurement [9, 11, 16, 17]. Accordingly, differences were higher in volunteers than in patients presenting with an increased thickness of all arterial wall layers due to atherosclerosis. Thereby, the relative proportion of the intima-media complex and the measurement difference between MRI and ultrasound is reduced with increasing wall thickness. Other explanations include the lower spatial resolution and partial volume effects in MRI which can in part be compensated by an increase of in-plane spatial resolution in future studies. As a result, cutoff values from large ultrasound studies on IMT indicating physiological and pathological values cannot simply be transferred to MRI measurements. As a result of the increasing application of vascular MRI and the clear advantages in terms of plaque imaging, future studies acquiring representative and age-dependent normal values in large cohorts of healthy volunteers are needed, cf. ultrasound studies [23], to identify pathological wall changes at an early stage.
Carotid distensibility was successfully measured using a 3D turbo spin echo imaging protocol in a previous study on ten healthy volunteers providing larger coverage of the vessel and thus more information [8]. However, MRI was not compared with ultrasound providing significantly higher spatial and temporal resolution. Comparison with ultrasound in another ten healthy volunteers and five hypertensive subjects revealed good agreement of both techniques [9]. Our results showed comparable agreement in a larger cohort of volunteers and patients at 3 T. Higher magnetic fields have the potential to improve image quality owing to the significant gain in signal-to-noise ratios or reduced velocity noise as shown for ex vivo plaque characterization or phased contrast flow measurements [24, 25]. The major advantage of the higher field strength of 3 T in this study compared with 1.5 T MRI is related to the substantial increase in the signal-to-noise ratio (SNR). This results in improved in-plane spatial resolution, which in turn could improve the accuracy of the measurements owing to improved depiction of the vessel wall as shown in previous studies on carotid artery imaging [26, 27]. Additionally, for a given spatial resolution, the enhanced SNR for 3 T MRI in conjunction with parallel imaging can be used to shorten overall examination times compared with 1.5 T MRI. Such imaging protocols may help to reduce motion artefacts, which is particularly relevant for the critically ill patient.
The current spatial resolution of 3D T1 CINE imaging of 0.8 mm3 was most probably the reason for limited intra- and interobserver agreement and reproducibility. In addition, temporal resolution was currently considerably lower compared with ultrasound. Thus, further increase of spatial and temporal resolution is needed to provide a reliable 3D assessment of compliance within the carotid bifurcation. In this context, advanced spatiotemporal image acceleration may help to achieve higher spatial resolution while keeping the duration of individual sequences down to acceptable levels [28, 29]. Moreover, findings of the current study need to be validated in larger patient studies in order to test the reliability of compliance measurements.
Both 2D dark blood T2-weighted and 3D T1 CINE imaging were successfully performed with high image quality by using 3 T MRI in this study. The combined measurement of morphological and functional properties of the CCA wall allows a more detailed characterization of the carotid arteries compared with the measurement of wall thickness alone. Such an analysis has the potential to precisely assess the vessel walls for longitudinal studies e.g. testing the influence of lipid lowering therapy. Furthermore, this combined measurement strategy could be applied to predict of complex aortic plaques in patients with ischemic stroke as recently shown for carotid ultrasound [4]. Compared with previous 2D studies on carotid compliance by MRI, 3D T1 CINE sequences allow for the analysis of local compliance at every site of the carotid bifurcation and could be ideally combined with current protocols for the characterization of ICA stenosis morphology.
References
Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M (2007) Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation 115:459–467
O’Rourke MF, Staessen JA, Vlachopoulos C, Duprez D, Plante GE (2002) Clinical applications of arterial stiffness; definitions and reference values. Am J Hypertens 15:426–444
van Popele NM, Grobbee DE, Bots ML et al (2001) Association between arterial stiffness and atherosclerosis: the Rotterdam Study. Stroke 32:454–460
Harloff A, Strecker C, Reinhard M et al (2006) Combined measurement of carotid stiffness and intima-media thickness improves prediction of complex aortic plaques in patients with ischemic stroke. Stroke 37:2708–2712
Saam T, Hatsukami TS, Takaya N et al (2007) The vulnerable, or high-risk, atherosclerotic plaque: noninvasive MR imaging for characterization and assessment. Radiology 244:64–77
Saam T, Underhill HR, Chu B et al (2008) Prevalence of American Heart Association type VI carotid atherosclerotic lesions identified by magnetic resonance imaging for different levels of stenosis as measured by duplex ultrasound. J Am Coll Cardiol 51:1014–1021
Sanz J, Fayad ZA (2008) Imaging of atherosclerotic cardiovascular disease. Nature 451:953–957
Crowe LA, Gatehouse P, Yang GZ et al (2003) Volume-selective 3D turbo spin echo imaging for vascular wall imaging and distensibility measurement. J Magn Reson Imaging 17:572–580
Crowe LA, Ariff B, Keegan J et al (2005) Comparison between three-dimensional volume-selective turbo spin-echo imaging and two-dimensional ultrasound for assessing carotid artery structure and function. J Magn Reson Imaging 21:282–289
Mani V, Aguiar SH, Itskovich VV et al (2006) Carotid black blood MRI burden of atherosclerotic disease assessment correlates with ultrasound intima-media thickness. J Cardiovasc Magn Reson 8:529–534
Leeson CP, Robinson M, Francis JM et al (2006) Cardiovascular magnetic resonance imaging for non-invasive assessment of vascular function: validation against ultrasound. J Cardiovasc Magn Reson 8:381–387
Wiesmann F, Petersen SE, Leeson PM et al (2004) Global impairment of brachial, carotid, and aortic vascular function in young smokers: direct quantification by high-resolution magnetic resonance imaging. J Am Coll Cardiol 44:2056–2064
Balu N, Chu B, Hatsukami TS, Yuan C, Yarnykh VL (2008) Comparison between 2D and 3D high-resolution black-blood techniques for carotid artery wall imaging in clinically significant atherosclerosis. J Magn Reson Imaging 27:918–924
Koktzoglou I, Chung Y-C, Carroll TJ, Simonetti OP, Morasch MD, Li D (2007) Three-dimensional black-blood MR imaging of carotid arteries with segmented steady-state free precession: initial experience. Radiology 243:220–228
Varghese A, Merrifield RD, Crowe LA et al (2006) Evaluation of carotid artery wall volume measurement using novel semiautomated analysis software. J Magn Reson Imaging 24:1401–1408
Underhill HR, Kerwin WS, Hatsukami TS, Yuan C (2006) Automated measurement of mean wall thickness in the common carotid artery by MRI: a comparison to intima-media thickness by B-mode ultrasound. J Magn Reson Imaging 24:379–387
Boussel L, Serusclat A, Skilton MR et al (2007) The reliability of high resolution MRI in the measurement of early stage carotid wall thickening. J Cardiovasc Magn Reson 9:771–776
Alizadeh Dehnavi R, Doornbos J et al (2007) Assessment of the carotid artery by MRI at 3 T: a study on reproducibility. J Magn Reson Imaging 25:1035–1043
Harloff A, Handke M, Geibel A et al (2005) Do stroke patients with normal carotid arteries require TEE for exclusion of relevant aortic plaques? J Neurol Neurosurg Psychiatry 76:1654–1658
Touboul PJ, Hennerici MG, Meairs S et al (2007) Mannheim carotid intima-media thickness consensus (2004–2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis 23:75–80
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Crowe LA, Keegan J, Gatehouse PD et al (2005) 3D volume-selective turbo spin echo for carotid artery wall imaging with navigator detection of swallowing. J Magn Reson Imaging 22:583–588
de Groot E, van Leuven SI, Duivenvoorden R et al (2008) Measurement of carotid intima-media thickness to assess progression and regression of atherosclerosis. Nat Clin Pract Cardiovasc Med 5:280–288
Koops A, Ittrich H, Petri S et al (2007) Multicontrast-weighted magnetic resonance imaging of atherosclerotic plaques at 3.0 and 1.5 Tesla: ex-vivo comparison with histopathologic correlation. Eur Radiol 17:279–286
Lotz J, Döker R, Noeske R et al (2005) In vitro validation of phasecontrast flow measurements at 3 T in comparison to 1.5 T: precision, accuracy, and signal-to-noise ratios. J Magn Reson Imaging 21:604–610
Yarnykh VL, Terashima M, Hayes CE et al (2006) Multicontrast black-blood MRI of carotid arteries: comparison between 1.5 and 3 tesla magnetic field strengths. J Magn Reson Imaging 23:691–698
Anumula S, Song HK, Wright AC, Wehrli FW (2005) High-resolution black-blood MRI of the carotid vessel wall using phased-array coils at 1.5 and 3 Tesla. Acad Radiol 12:1521–1526
Breuer FA, Kellman P, Griswold MA, Jakob PM (2005) Dynamic autocalibrated parallel imaging using temporal GRAPPA (TGRAPPA). Magn Reson Med 53:981–985
Tsao J, Boesiger P, Pruessmann KP (2003) k-t BLAST and k-t SENSE: dynamic MRI with high frame rate exploiting spatiotemporal correlations. Magn Reson Med 50:1031–1042
Conflicts of Interest Disclosure
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harloff, A., Zech, T., Frydrychowicz, A. et al. Carotid intima-media thickness and distensibility measured by MRI at 3 T versus high-resolution ultrasound. Eur Radiol 19, 1470–1479 (2009). https://doi.org/10.1007/s00330-009-1295-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1295-8