Abstract
The authors wish to highlight the evolution that has occurred in fetal ultrasound in recent years. A first significant evolution lies in the increasing contribution of first trimester ultrasound for the detection of fetal anomalies. Malformations of several organs and systems have been diagnosed during the first trimester. Furthermore the systematic measurement of the fetal neck translucency has led to increasing rate of detection of aneuploidies and heart malformations. For several years now, three-dimensional (3D) and 4D ultrasound (US) have been used as a complementary tool to 2D US for the evaluation of fetal morphology. This brings an improved morphologic assessment of the fetus. Applications of the techniques are increasing, especially for the fetal face, heart and extremities. The third field where fetal US is continuously providing important information is the knowledge of the natural history of diseases. This has brought significant improvement in the postnatal management of several diseases, especially urinary tract dilatation and broncho-pulmonary malformation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For more than 30 years ultrasound (US) has been applied for the evaluation of pregnancies. The main focuses have been fetal well-being and the development and screening of fetal abnormalities.
As equipment is improving, and as experience is growing, more and more precise diagnoses are obtained. Progress has been achieved in many directions; three among them should be underlined: (1) prenatal diagnosis in the first trimester, (2) the role of three-dimensional (3D) (and 4D) US and (3) the contribution of fetal US to the natural history and proper management of diseases.
Sonographic diagnosis during the first trimester
Thanks to the use of endovaginal probes, the developing pregnancy can be visualized earlier than with transabdominal US. Various anatomical landmarks can be analyzed and abnormalities can be detected already during the first trimester (10-14 weeks gestation) [1–4]. Furthermore, some specific signs have been used in order to find markers of fetal aneuploidy.
Congenital malformations
The detection of malformations of various organs has been reported during the first trimester. Some are obvious and their diagnosis is straightforward, while for others control examinations will be mandatory during later pregnancy in order to better characterize the anomaly.
The diagnosis is easy for major central nervous system (CNS) malformations, some renal or neck anomalies (Figs. 1,2,3). The diagnosis of spina bifida, limbs or heart malformations are possible, yet less easy during the first trimester [2,3] (Figs. 4, 5). In some instances, 3D (4D) ultrasound will help for a precise diagnosis (see below). The early detection will determine the need for complementary examination and see early detection of aneuploidies (Figs. 2, 3).
These potentialities of the first trimester US might bring in the future years a large discussion about the exact yield of the mid trimester examination that is considered at present time as the main screening examination [4].
Nuchal translucency (NT)
Increased NT describes the subcutaneous accumulation of fluid in the back of the fetal neck which can occur in early pregnancy.
On US, NT corresponds to the maximum thickness of subcutaneous translucency between the skin and the soft tissue overlying the cervical spine (Fig. 6). Abnormal NT is supposed to result from cardiac failure or delayed lymphatic connexions. Measurements of the NT should be obtained in a mid-sagittal section of the fetal neck with sufficient magnification. Calipers must be placed on the echogenic lines (on-to-on measurement). The NT increases with the gestational age (GA). A threshold of 3 mm is commonly used when measured between 10 and 14 weeks (90–95th centile). The 99th centile is about 3.5 mm.
The NT measurement is considered as an effective noninvasive screening method for trisomy 21 and other aneuploidies in an unselected population, especially in combination with serum free β HCG, pregnancy associated plasma protein-A (PAPP-A) and maternal age. Detection rates of 57–91% of trisomy 21 have been reported [5–8].
In chromosomally normal fetuses with increased NT (above the 95th centile) there is a higher incidence of poor prognosis because of a higher incidence of spontaneous abortion and structural anomalies. Anomalies of all systems have been reported. The largest percentage involves cardiac defects (Fig. 7). Only those with normal karyotype and no additional malformations on follow-up US have a good prognosis.
The NT can either regress or, on the contrary, increase after 14 weeks. An increasing size should suggest the possibility of an infection or a genetic syndrome. The anomaly can then evolve towards generalized hydrops with poor prognosis.
The management of pregnancies with increased NT will depend upon the thickness of the NT, the evolution and the associated findings. In euploid fetuses, the prevalence of fetal abnormalities and adverse pregnancy outcome increase exponentially with NT thickness above 3.5 mm.
The chances of delivering a baby with no major abnormalities are about 70% for NT between 3.5 and 4.4 mm, 50% between 4.5 and 5.4 mm, and 15% above 6.5 mm.
The parents should be reassured that once the presence of an aneuploidy is excluded and the fetus is shown to be normal on a subsequent 20–22 weeks US examination, the risk of adverse perinatal outcome is not increased [5–8].
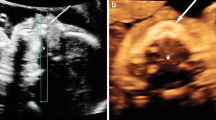
The ductus venosus (DV)
The ductus venosus connects the umbilical vein to the fetal heart and brings oxygenated blood from the placenta to the fetal circulation. Doppler analysis of the DV shows a biphasic pattern with velocities peaking at ventricular systole and early diastole.
The amount of blood shunted to the DV may be modified in particular conditions of hypovolemia and hypoxia.
In normal conditions, the direction of blood flow is towards the heart. Reversed velocities can be related to congenital heart disease or to heart failure (Fig. 8).
Early cardiac dysfunction leading to reversed end-diastolic velocity has been suggested as the underlying cause of increased NT observed in aneuploid fetuses during the first trimester [9].
Detection rates for aneuploidies with the use of DV blood flow studies range from 59 to 93% (2–21% false-positive rates). It can be used in combination with the nasal bones or NT measurements [9].
Noteworthily, diagnostic US has been used for many years with a remarkable history of safety. The use of Doppler US had raised some concern in early pregnancies. The introduction of pulsed and color Doppler determines higher levels of ultrasonic energy but the risks for the embryo and the fetus seem more theoretical than scientifically demonstrated.
Still, all ultrasound (US) scientific Societies emphasize the need for a cautious and limited use of Doppler in early pregnancy in accordance with the ALARA principles. This means that the use is not “prohibited” but the technique should be used only with clear medical indications [10].
3D (4D) US
These last years, the use of 3D and more recently 4D ultrasound has extended greatly and provides a clearer image of the fetus. The technique will always be used as a complementary tool to the 2D ultrasound examination of the fetus. It provides in selected indications additional information, especially when searching for dysmorphologic syndromes. The technique uses a special volumic abdominal or transvaginal transducer. The interesting area is defined by 2D US and a volume is acquired automatically through the special transducer. Three orthogonal planes are acquired and the surface rendering images can be displayed.
Not all patients will have beautiful images made of their fetuses (Figs. 9, 10). Gestational age is very important; the best 3D US images are obtained from 10 to 12 weeks using an endovaginal transducer and from 24 to 30 weeks using a transabdominal transducer [11].
Fetal position and any amniotic fluid adjacent to the structure are crucial factors affecting image quality. In general, 3D US studies take time, additional training and special equipment. Rapid technological development will allow real-time 3D ultrasound (4D) to provide improved patient care and increased knowledge of developmental anatomy;
Numerous studies have addressed on the usefulness of 3D US in the evaluation of fetal anatomy and anomalies [12, 13]; a recent study about the evaluation of fetal anomalies reports that 3D US images were consistently advantageous in cases of facial, hand and foot anomalies and axial spine section and neural tube defect [13]. Further applications of 3D US will clearly develop: for instance, a recent article demonstrates the contribution of 3D US for the measurement of normal fetal lung volume [14].
The exact clinical impact of 3D US is still under debate. With improvements in resolution and acquisition speed, image quality will improve, and 3D US will assume a greater role in imaging the embryo and fetal anomalies. Developments in 4D US technology now make it possible to view surface 3D images in real time. Rapid volume acquisitions open the door to the study of fetal “behavior” and motion. The use of telemedicine to send selected studies to experts is a promising field [15].
Fetal face
The fetal face is an area of considerable information and is included in all standard obstetrical examinations. The accurate detection of a facial anomaly would determine a complete survey for other structural malformations as well as chromosomal analysis.
There has been impressive progress in the US imaging of the fetus. Still, the fetal face can be analyzed only to a limited extent by conventional 2D US.
Three-dimensional US allows clearer surface images of the fetal face than 2D US. Both multiplanar and surface rendering images are helpful for the evaluation of the fetal face (Figs. 9,10,11).
Cleft lip and palate are common cranio-facial malformations. A more accurate assessment of the extent of the cleft into the anterior alveolar ridge or the posterior palate can be achieved using multiplanar imaging (Figs. 12, 13, 14).
Surface rendering images are more easily understood by the parents and therefore more helpful in explaining to the family and to the surgeon.
The tooth-buds are also more easily demonstrated. Multiplanar reconstruction can display a true coronal view of the lips even if the original plane was different.
It has been shown that 3D US offers improved diagnostic capability in cases such as abnormal profile or micrognathia and seems to offer new possibilities in prenatal dysmorphology. This is an area of considerable interest and research activity at present time (Fig. 11) [16–18].
A recent development using the “3D reverse face view” has been shown to ensure a more accurate diagnosis of clefts of the posterior palate. By rotating the face by 180°, it is approached from the posterior plate to the anterior plate and this renders the anatomical delineation easier [19].
Fetal spine and skeleton
Three- or four-dimensional US offers a great advantage in imaging the fetal spine and skeleton, since it allows the examiner to obtain an integrated overview of the continuity and curvature of the spine by using rendered reconstructions (Fig. 15).
Spinal anomalies, such as neural tube defects, scoliosis and hemi-vertebrae, are common congenital defects. Two-dimensional US can determine accurately the location of a neural tube defect within one vertebral body in 79% of cases; however, 3D US localizes fetal neural defects with more accuracy and helps in demonstrating the extent of neural tube defects. Rendered and planar images can be magnified for better visualization and the rendered image may be used as a reference for individual planar view. Simultaneous display of orthogonal images through the same vertebral body allows the examiner to identify more accurately the specific level of that vertebral body. Abnormal spine curvature in cases of scoliosis of the spine may be demonstrated with 3D US [20] (Fig. 16).
Cranial sutures may also be displayed (Fig. 17), allowing the precise location of an encephalocele mass or the characterisation of craniosynostosis [21, 22].
The use of 3D US has also proved useful in the assessment of limb extremities malformation especially in case of amputation of hands and feet and position anomalies [23] (Fig. 18).
Finally, the 3D US technology can be used to examine the fetal brain. The image of the fetal brain is improved with a transvaginal approach. Tomographic sections can be generated in all three conventional planes. The possibility “to travel” in the brain volume enables location of the three horns view (anterior, posterior and inferior) and evaluation of fetal brain pathology. Monteagudo and co-workers describe how to obtain and magnify the information stored as a 3D volume of the fetal brain by using the transvaginal approach [24] (Fig. 19).
Fetal heart
Congenital heart defects (CHD) are frequent malformations (six to eight cases for 1,000 births) that are too rarely diagnosed antenatally. This can be explained by the fact that this type of diagnosis is highly dependent on the operator education, experience and skill. Computer-assisted US imaging is expected to facilitate CHD identification by recording tight heart view sequences in an automated way and providing volume rendering. Normal and abnormal 3D US images of the fetal heart are presented, including tetralogy of Fallot, complete transposition of the great arteries and ventricular septal defects.
The multiplanar display coupled with 3D surface rendering clearly demonstrates the heart anatomy and the presence of any malformations.
Three-dimensional US allows a greater number of cardiac views to be extracted from volume data than 2D US. The four chambers view is obtained in a similar proportion with both techniques but the left and right outflow tract views are obtained much more frequently with 3D US than with 2D US. Three-dimensional US allows a larger number of cardiac views to be extracted from volume data than did 2D US [25, 26] (Fig. 20).
Recently, the efficacy of the technique has been improved through the introduction of the spatio-temporal image correlation (STIC) acquisition technique.
The STIC technique is an automatic volume acquisition through the fetal heart. It results in a complete fetal cardiac cycle that is displayed in motion in a continuous 3D cineloop sequence. The entire information can be analyzed online or sent to experts. This screening is of great potential in order to optimize the perinatal work-up and management [15].
The natural history of diseases: the example of mild urinary tract dilatation
Mild urinary tract dilatation
Dilatation of the renal pelvis is a common finding on obstetrical US. Its frequency is evaluated around 1–4% of all pregnancies. Yet, all dilatations do not have the same clinical relevance; furthermore, their antenatal and postnatal evolution is variable. This has led to abundant and somewhat controversial literature about the best work-up and follow-up after birth [27–29].
Various criteria are used in order to objectivate renal dilatation. The best criterion is the measurement of the A-P diameter of the renal pelvis on a transverse scan of the fetal abdomen (Fig. 21). Using this measurement, several threshold values have been applied in order to be able to predict the postnatal outcome especially in cases with moderate dilatation (less than 15 mm). Most authors agree that the upper limit should be 4 mm during the second and 7 mm during the third trimesters of the pregnancy. These limits are set in order to detect not only patients that will need eventual corrective surgery (in case of obstructive dilatation) but also the majority of fetuses and neonates presenting vesico-ureteric reflux. These patients are at risk for developing complications and eventually worsen renal function [30–32].
Other sonographic evidence of an abnormality of the urinary tract includes the visibility of the fetal ureter at any moment of the pregnancy (Fig. 22a) and the demonstration of an enlarged bladder (Fig. 23) (over 3 cm in length during the second and 5 cm during the third trimesters).
Noteworthy, pyelectasis refers to a visible renal pelvis below the significant threshold. During the second trimester, it is considered as a minor sign of chromosomal anomaly [33].
Abnormalities of the urinary tract can be found at any time during the pregnancy. Interestingly, most cases of urinary tract dilatation are diagnosed during the third trimester; this might be due to the higher urinary output of the fetal kidneys in which the nephrogenesis has ended and where all glomeruli are functional. The third trimester examination is therefore of utmost importance in order to detect nonlethal uropathies. Furthermore, the degree of dilatation may increase or decrease during each trimester. Therefore, in order to screen all potentially abnormal cases, one sonographic examination should be performed during each trimester [34].
Once a dilatation has been detected in utero, the subsequent evaluation should answer to three interrogations: the origin of the dilatation, the co-exsistence of associated anomalies and finally the prognosis of the malformation.
The origin of the dilatation can be obstruction, non obstructive dilatation or/and reflux. The sonographic analysis should include the kidneys, the bladder and the ureters. The most common causes of obstruction are related to the ureteropelvic junction (UPJ) or ureterovesicle junction (UVJ) obstruction and to complicated duplex systems. Interestingly, thanks to the systematic sonographic screening during pregnancies, more cases of nonobstructive dilatation and vesico-ureteric reflux have been reported. Furthermore, main cause of fetal dilatation has become vesico-ureteric as demonstrated by systematic neonatal VCUG (Fig. 22b). Urinary tract dilatation can also result from infra-vesical obstruction especially in male fetuses (Fig. 23). In such cases the bladder will be enlarged and the urinary tract eventually markedly dilated.
In most cases, the sonographic evaluation will be able to differentiate between most etiologies of urinary tract dilatation. In selected cases, fetal magnetic resonance (MR) imaging will provide additional information that will help to better assess the uropathy. This is particularly true in cases with bilateral or complex uropathies [35–37].
Urinary tract dilatation can be associated to other organ malformations and therefore the sonographic survey should be as meticulous and complete as possible. Furthermore, bilateral renal dilatation and bladder outlet obstruction have an increased risk of associated chromosomal anomalies, and therefore in such cases an evaluation of fetal chromosomes may be warranted.
Once the condition has been evaluated completely and a favourable prognosis established, a sonographic follow-up is necessary in order to verify the evolution of the dilatation.
It is of utmost importance that any information relevant for the proper postnatal management is correctly transmitted to the postnatal team that will be in charge of the newborn.
After birth, some conditions require an immediate confirmation and therapeutic maneuvers. For instance, obstructive posterior urethral valves or prolapsed ectopic ureterocele into the urethra leading to oligo-anuria necessitate an immediate treatment. Whenever useful, US and voiding cysto-urethrogram (VCUG) can be performed immediately after birth in order to confirm the anomaly [37].
In all other cases, the work-up can be planned without emergency. A large debate arose regarding the respective role of ultrasound and VCUG in the postnatal work-up.
Practically, we have applied an algorithm based on US examination at birth (Table 1). A first US should be performed during the first week of life in order to verify the urinary tract, including the kidneys, bladder and ureters. The sonographic analysis should be as detailed as possible (Table 2) and any significant anomaly should lead to performance of a VCUG. If the examination is normal, a control sonographic examination should be performed at the age of 1 month. Again if any abnormality is found, a VCUG should be performed, but if no anomaly is demonstrated no further evaluation is needed. At this stage, any prophylactic antibiotherapy should be stopped [38–41].
Using this algorithm, very few abnormal cases escape the work-up and the risk of complications is very low. At the end of the work-up, about 70% of cases will end with a precise diagnosis, whereas in 30% the origin of the dilatation will not be established (i.e., nonobstructive, nonrefluxing dilatation, etc.), but clearly no complications will be expected in such cases and the child can be managed conservatively.
Congenital broncho-pulmonary malformation (BPM)
Obstetrical US and fetal MR imaging allow the proper characterization of BPM. Congenital cystic adenomatoid malformation (CCAM) and pulmonary sequestration (PS) are the most common abnormalities reported [42–46].
The diagnosis is based upon the demonstration of an echogenic mass usually affecting one lung (even through CCAM can appear bilaterally) and more commonly in the lower lobes (even through mediastinal and infradiaphragmatic PS do occur and CCAM can affect the entire lung).
Both can display a mixed echogenic pattern with small or large cysts.
The demonstration of a feeding vessel arising from the aorta is characteristic of PS. Both malformations may coexist in the same patient.
Most diagnoses are achieved during the second trimester. The criteria of good or bad prognosis have been reported (i.e., fetal hydrops as the criterion of bad prognosis).
Thanks to the US follow-up of pregnancies and to MR imaging in some selected cases, it became obvious that some of these malformations underwent a reduction in size with ongoing pregnancy. This reduction in size was either absolute and corresponded to a true involution, or in other patients, the reduction was considered as relative: the malformation did not really diminish while the rest of the fetus grew. The origin of the apparent resolution is unknown but could be related to a reduction in the vascularization (Figs. 24, 25) [43–46].
BP foregut malformation. a Transverse scan of the fetal abdomen: the hyperechoic malformation (arrow) is located between the spine and stomach. b MR imaging at birth. T2-weighted sequence. The BPM appears cystic and septated. c MR imaging at age 6 months. The anomaly has almost completely disappeared
This potential involution of BPM brought a significant change in the management of such patients. To date no termination of pregnancy on the basis of an isolated BPM should be proposed anymore; instead a US follow-up should monitor the evolution of the size of the malformation and the effects on fetal well-being. The findings should be transmitted to the pediatric team that will manage the patient at birth.
At birth, there should not be emergency surgery unless the patient experiences respiratory or heart failure.
A chest X-ray and US should be performed in order to evaluate the sequelae of the malformation. CT scan or better MR imaging can be used for the presurgical assessment. In asymptomatic newborns, a conservative attitude has been advocated as opposed to systematic surgery. Some debate has arisen about this alternative. Large follow-up studies are necessary in order to confirm this choice [47].
To date no obvious malignant transformation of an antenatal diagnosis has been demonstrated. The controversy seems similar to the one that occurred in the 1980s about a conservative nonsurgical treatment of multicystic dysplastic kidney.
In conclusion, many technical improvements have occurred in US equipment. This has been beneficial to embryo-fetal US. Earlier and clearer diagnoses are provided. Also, systematic US evaluation and follow-up provided information about the natural history of diseases.
References
Lazanes E (2003) What’s new in first trimester US. Radiol Clin N Amer 41:663–679
Souka AP, Nicolaides KH (1997) Diagnosis of fetal abnormalities at the 10–14 week scan. Ultrasound Obstet Gynecol 10:429–442
Whitlow BJ, Chatzipapas IK, Lazanakis ML et al (1999) The value of sonography in early pregnancy for the detection of fetal abnormalities in an unselected population. Br J Obstet Gynaecol 106:929–936
Crane JP, LeFevre ML, Winborn RC et al (1994) A randomised trial of prenatal ultrasonographic screening impact on the detection, management, and outcome of anomalous fetuses. Am J Obstet Gynecol 171:392–399
Souka AP, von Kaisenberg CS, Hyetts JA, Sonek JD, Nicolaides KH (2005) Increased nuchal translucency with normal karyotype. Am J Obstet Gynecol 192:1005–1021
Cicero S, Spencer K, Avigdou K, Faiola S, Nicolaides KH (2005) Maternal serum biochemistry at 11–13th weeks in relation to the presence or absence of fetal nasal bone on US in chromosomally abnormal fetuses. Prenatal Diagn 25:977–983
Gyselaers WJA, Vereecken AJ, Van Herck EJH et al (2005) Population screening for fetal trisomy 21. Prenat Diagn 25:984–990
Ganapathy R, Guven M, Sethna F et al (2004) Natural history and outcome of prenatally diagnosed cystic hygroma. Prenat Diagn 24:965–968
Borell A (2004) The ductus venosus in early pregnancy and congenital anomalies. Prenat Diagn 24:688–692
Kurjak A (1999) Are color and pulsed Doppler sonography safe in early pregnancy ? J Perinat Med 27:423–430
Platt LD (2000) Three-dimensional ultrasound. Ultrasound Obstet Gynecol 16:295–298
Campbell S (2002) 4D, or not 4D: that is the question. Ultrasound Obstet Gynecol 19:1–4
Bega G, Lev-toaff A, Kuhlman K, Kurtz A, Goldberg B, Wapner R (2001) Three-dimensional ultrasonographic imaging in Obstetrics, present and future applications. J Ultrasound Med 20:391–408
Gerards FA, Engels MA, Twisk JW, van Vugt JM (2006) Normal fetal lung volume measured with three-dimensional ultrasound. Ultrasound Obstet Gynecol 27:134–144
Vinals F, Mandujano L, Vargas G, Giuliano A (2005) Prenatal diagnosis of congenital heart disease using four-dimensional spatio-temporal image correlation (STIC) telemedicine via an Internet link: a pilot study. Ultrasound Obstet Gynecol 25:25–31
Rotten D, Levaillant JM, Martinez H, Ducou le pointe H, Vicaut E (2002) The fetal mandible: a 2D and 3D sonographic approach to the diagnosis of retrognathia and micrognathia. Ultrasound Obstet Gynecol 19:122–130
Pretorius DH, House M, Nelson TR, Hollenbach KA (1995) Evaluation of normal and abnormal lips in fetuses: comparison between three-and two-dimensional sonography. AJR Am J Roentgenol 165:1233–1237
Ulm MR, Kratochwil A, Lum B, Lee A, Berttelheim D, Bernaschek G (1999) Three-dimensional ultrasonographic imaging of fetal tooth buds for characterization of fetal clefts. Early Hum Dev 55:67–75
Campbell S, Lees C, Moscoco G, Mall P (2005) US antenatal diagnosis of cleft palate by a new technique: the 3D “reverse face” view. Ultrasound Obstet Gynecol 25:12–18
Johnson D, Pretorius D, Riccabona M, Budorick N, Nelson T (1997) Three-dimensional ultrasound of fetal spine. Obstet Gynecol 89:434–438
Pretorius D, Nelson T (1994) Prenatal visualization of cranial sutures and fontanelles with three-dimensional ultrasonography. J Ultrasound Med 13:871–876
Chaoui R, Levaillant JM, Benoit B, Faro C, Wegrzyn P, Nicolaides KH (2005) Three-dimensional sonographic description of abnormal metopic suture in second- and third-trimester fetuses. Ultrasound Obstet Gynecol 26:761–764
Kos M, Hafner T, Funduk-Kurjak B, Bozek T, Kurjak A (2002) Limb deformities and three-dimensional ultrasound. J Perinat Med 30:40–47
Monteagudo A, Timor Tritsch, Mayberry P (2000) Three-dimensional transvaginal neurosonography of fetal brain: “navigating” in the volume scan. Ultrasound Obstet Gynecol 16:307–311
Bega G, Kuhlman K, Lev-Toaff A, Kurtz A, Wapner R (2001) Application of three-dimensional ultrasonography in the evaluation of the fetal heart. J Ultrasound Med 20:307–313
Nelson TR, Pretorius DH, Sklansky MS, Hangen-Ansert S (1996) Three-dimensional echocardiographic evaluation of fetal heart anatomy and function: acquisition, analysis and display. J Ultrasound Med 15:1–9
Ismaili K, Avni EF, Piepsz A, Wissing KM, Cochat P, Aubert D, Hall M (2004) Current management of infants with renal pelvis dilation: a survey by French speaking pediatric nephrologists and urologists. Pediatr Nephrol 19:966–971
Gunn TR, Mora D, Pease P (1995) Antenatal diagnosis of urinary tract abnormalities by ultrasonography after 28 weeks gestation: incidence and outcome. Am J Obstet Gynecol 172:479–482
Ismaili K, Hall M, Donner C, Thomas D, Vermeylen D, Avni FE (2003) Results of systematic screening for minor degrees of fetal renal pelvis dilatation in an unselected population. Am J Obstet Gynecol 188:242–246
Stocks A, Richards D, Frentzen B, Richard G (1996) Correlation of prenatal renal pelvic anteroposterior diameter with outcome in infancy. J Urol 155:1060–1062
Elder J (1992) Commentary: importance of antenatal diagnosis of vesicouretearal reflux. J Urol 148:1750–1754
Maizels M, Reisman ME, Flom LS, Nelson J, Fernbach S, Firlit CF, Conway JJ (1992) Grading nephro-ureteral dilatation detected in the first year of life: correlation with obstruction. J Urol 148:609–614
Chudleigh T (2001) Mild pyelectasis. Prenat Diagn 21:916–941
Economou G, Egginton JA, Brookfield SK (1994) The importance of late pregnancy scans for renal tract abnormalities. Prenat Diagn 14:177–180
Montemarano H, Bulas DI, Rushton G, Selby D (1998) Bladder distension and pyelectasis in the male fetus. J Ultrasound Med 17:743–749
Blachar A, Blachar Y, Livne PM, Zurkowski L, Pelet D, Mogilner B (1994) Clinical outcome and follow-up of prenatal hydronephrosis. Prenat Diagn 8:30–35
Avni FE, Garel L, Hall M, Rypens F (2002) Perinatal approach to anomalies of the urinary tract, adrenals and genital system. In: Avni EF (ed) Perinatal imaging. Springer, Berlin Heidelberg New York, pp 153–196
Yerkes EB, Adams MC, Pope JC, Brock JW (1999) Does every patient with prenatal hydronephrosis need voiding cystourethrography? J Urol 162:1218–1220
Ismaili K, Avni FE, Hall M (2002) Results of systematic voiding cystourethrography in infants with antenatally diagnosed renal pelvis dilation. J Pediatr 141:21–24
Ismaili K, Avni FE, Wissing M, Hall M (2004) Long-term clinical outcome of infants with mild and moderate pyelectasis: validation of neonatal ultrasound as a screening tool to detect significant nephro-uropathies. J Pediatr 144:759–765
John U, Kahler C, Schulz S, Mentzel HJ, Vogt S, Misselwitz (2004) The impact of fetal renal pelvic diameter on post natal outcome. Prenat Diagn 24:591–595
Johnson AM, Hubbard AM (2004) Congenital abnormalies of the fetal/neonatal chest. Semin Roentgenol 39:197–214
Levine D, Barnewolt CE, Mehta TS, Trop I, Estroff J, Wong G (2003) Fetal thoracic abnormalities: MR imaging. Radiology 228:379–388
Langer B, Donato L, Riethmuller C, Becmeur F, Dreyfus M, Favre R, Schlaeder G (1995) Spontaneous regression of fetal pulmonary sequestration. Ultrasound Obstet Gynecol 6:33–39
Hsu KF, Wu MH, Chang CH, Yao BL, Chang FM (1995) Complete intrauterine resolution of fetal congenital cystic adenomatoid malformation of the lung type III. J Ultrasound Med 14:871–875
Achiron R, Strauss S, Seidman DS, Lipitz S, Mashiach S, Goldman B (1995) Fetal lung hyperechogenicity: prenatal ultrasonographic diagnosis, natural history and neonatal outcome. Ultrasound Obstet Gynecol 6:40–42
Thorpe-Beeston JG, Nicolaides KH (1994) Cystic adenomatoid malformation of the lung: prenatal diagnosis and outcome. Prenat Diagn 14:677–688
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Avni, F.E., Cos, T., Cassart, M. et al. Evolution of fetal ultrasonography. Eur Radiol 17, 419–431 (2007). https://doi.org/10.1007/s00330-006-0307-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0307-1