Abstract
Research regarding renal involvement in SSc has almost exclusively focused on scleroderma renal crisis (SRC). There are relatively limited data regarding renal impairment in SSc beyond SRC. We performed an electronic search using the key words systemic sclerosis or scleroderma combined with each of the following: renal dysfunction, kidney, glomerular filtration rate (GFR), proteinuria and hematuria. We searched for reports relevant to renal dysfunction in SSc beyond SRC. In 796 SSc patients recruited in five studies. 251 (31.5%) had GFR < 90 ml/min whereas 155(19.5%) patients had GFR < 60 ml/min. Most data indicate that the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula should be considered as the most suitable tool for assessing renal function in SSc pts, since it provides similar results to measured GFR. These data indicate that renal dysfunction in SSc in not uncommon and therefore patients with SSc should have their renal function assessed by GFR estimation on a regular basis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a multisystem rheumatic disease characterized by vascular and fibrotic manifestations [1,2,3,4]; practically every organ can be affected including the kidneys [5]. The most severe form of renal involvement in SSc is scleroderma renal crisis (SRC), which up until the 1970s was the main cause of death in patients with SSc [6]. SRC is a complex vasculopathy affecting the kidneys leading to uncontrolled hypertension and rapidly progressive renal failure. Research regarding renal involvement in SSc has almost exclusively focused on SRC leading to a better understanding of the pathophysiology of this manifestation. Evidence showed that the main driver of SRC was the renin-angiotensin system (RAS); this knowledge led to the early use of drugs targeting RAS in SSc patients developing SRC. This therapeutic approach was highly successful leading to a significant reduction of mortality associated with SRC [7]. Nowadays interstitial lung disease and pulmonary hypertension have replaced SRC as leading causes of death [8].
Renal involvement in the context of systemic rheumatic diseases has been generally under-investigated with the exceptions of diseases that primarily affect the kidneys by immune mechanisms such as systemic lupus erythematosus or ANCA-associated vasculitides [9, 10]. In rheumatoid arthritis (RA), the most common rheumatic disease, data regarding renal dysfunction are relatively limited. For many years research has focused on the potential effects of nephrotoxic medications or inflammation. However, clinical evidence points to the direction that renal dysfunction in RA mainly associates with cardiovascular risk factors and not disease related factors or drugs [11, 12]. Accumulating data indicate that cardiovascular disease and renal dysfunction share many risk factors and appear to be tightly linked [13, 14]. In SSc, recent evidence suggests that cardiovascular disease is more prevalent that in general population and is responsible for 20–40% of mortality in SSc [15]. Taking into account that cardiovascular disease and renal dysfunction are strongly associated, we may hypothesize that renal dysfunction in SSc is not uncommon. There are relatively limited data regarding renal impairment in SSc beyond SRC. In this narrative review we focused on answering the following questions: (1) Is renal function impaired in SSc? (2) Do GFR predictive equations perform well in this population? (3) Are there alternative ways of assessing renal function in patients with SSc? and (4) do patients with SSc display significant proteinuria?
Methods
We performed an electronic search (Medline and Scopus) from December 2020 until March 2021 using the key words systemic sclerosis or scleroderma combined with each of the following: renal dysfunction, kidney, glomerular filtration rate, proteinuria and hematuria. Only papers published as full articles in English language were included and no time limit was set. We searched for reports relevant to renal dysfunction in SSc. Eligible studies were those reporting data regarding GFR or proteinuria in patients with SSc. Studies regarding SRC or review articles were excluded. A detailed flowchart of the search is depicted in Fig. 1.
-
Is renal function impaired in patients with SSc? Do GFR predictive equations perform well in this population?
Glomerular Filtration rate (GFR) is the gold standard for assessing renal function. It can either be measured directly or estimated via predictive equations. The established way to measure GFR (mGFR) is usingTc-99 m diethylenetriaminepentacetate acid (DTPA) [16]. In the kidney, DTPA is not subjected to either tubular secretion or reabsorption, making this molecule ideal for GFR measurement. Alternative ways to measure GFR are 51Cr-EDTA or iohexol clearance. GFR can also be estimated (eGFR) with specific equations with the most widely used being the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI), Modification of Diet in Renal Disease (MDRD 4- and 7-variable) and Cockroft-Gault (CG) formulas. Several studies provide data regarding GFR in patients with SSc.
Caron et al. used the Canadian Scleroderma research group registry to assess eGFR by employing the CG formula annually, in 561 pts over 5 years [17]. Normal clearance was defined as eGFR > 60 ml/min. In this cohort, 5% suffered SRC and 20% had low eGFR without signs of SRC; the rate of eGFR decline was 0.89%/year. These data indicate that renal dysfunction is not uncommon in SSc. This is the largest cohort study to assess GFR in patients with SSc. However, this study did not provide comparative data with healthy subjects or disease controls and therefore cannot answer the question of whether decreased GFR is more common in SSc compared to other chronic diseases or the general population.
Scheja et al. performed a study from 1983 to 2004 to examine renal function in 461 SSc pts, using GFR measurement [18]. GFR was measured by 51Cr-EDTA or iohexol clearance and was given as an age-adjusted percentage of the mean values for healthy subjects and the measurements were repeated yearly. GFR < 70% was considered low and was found in 48 pts; renal dysfunction was mostly associated with hypertension and cardiovascular disease.
Gupta et al. performed a cross-sectional study to explore the prevalence of renal impairment in 87 SSc pts, over the course of 3.5 years [19]. None of the pts developed SRC. eGFR was calculated with the CG formula and was found < 90 ml/min in 75% (n = 66) of the pts. Almost 30% (n = 26) of the pts had eGFR < 60 ml/min, evident of CKD.
Rosato et al. performed a large-scale prospective study to assess prognostic factors of renal involvement in SSc [20]. Renal involvement was studied in 121 patients with SSc over a period of approximately 5 years. Color Doppler Ultrasound of kidney (CDU) was used to assess renal vasculature and eGFR was calculated by the CKD-EPI equation. CDU indicated significant intrarenal arterial stiffness in SSc, which was further worsened in patients with capillaroscopic abnormalities and digital ulcers. Despite these findings, renal function markers were preserved even in patients with longer disease duration. Mean serum creatinine was 0.75 mg/dl, 24-h proteinuria 200 mg/24 h and CKD-EPI-calculated GFR 93.8 ml/min.
Suebmee et al. explored the correlation between eGFR and Tc-99 m DTPA mGFR in 76 SSc pts in a cross-sectional study [21]. eGFR was calculated by four equations: CKD-EPI, 7-variable MDRD, CG and creatinine clearance from 24-h urine collections. Serum creatinine (sCr) of all pts was < 1.4 mg/dl with a median value of 0.8 mg/dl. mGFR (median value 100.1 ml/min) showed the greatest correlation with the CKD-EPI and MDRD eGFR (mean 96.8 and 97 ml/min, respectively). Thirty pts had a reduced mGFR < 90 ml/min (3 pts < 60 ml/min and 27 pts between 60 and 90 ml/min). The clinical parameter with the strongest association with GFR was systolic blood pressure (SBP). These data indicate that in the majority of patients with SSc GFR is not significantly impaired. Furthermore, CKD-EPI and MDRD (7-variable) show a good correlation to mGFR and can be used to detect reduced GFR in SSc pts, which might uncover subclinical renal impairment.
Gigante et al. also assessed the performance of GFR predictive equations in pts with SSc [22]. They explored whether eGFR correlates with mGFR by Tc-99 m DTPA in 41 SSc pts with normal serum creatinine and a median age of 46 years. The mean value of measured GFR was 84 ml/min. SSc pts with CVD or under treatment with ACE-inhibitors had a greater reduction in GFR. Finally, it was shown that CKD-EPI-calculated eGFR showed the highest correlation to mGFR compared to MDRD (4- and 7-variable) and CG formula.
However, there is a single study that did not show a good correlation of mGFR and eGFR [23]. Reem et al. explored renal involvement in 31 SSc pts and 31 healthy controls with normal sCr (mean value 0.7 mg/dl), using mGFR (Tc-99 mm DTPA) and eGFR (CG and MDRD) over a 2-year time period. All subjects had a normal kidney ultrasound and none of them were treated with ACE-inhibitors. SSc pts had a mean mGFR of 79.24 ml/min, which was significantly different from that of the controls (107.49 ml/min). Reduced mGFR (< 90 ml/min) was noted in 17 pts, whereas CG and MDRD calculated eGFR was found reduced in only 6 and 7 pts, respectively, raising concerns about the validity of GFR predictive equations in SSc. Nevertheless, this study indicated that SSc pts can indeed have renal dysfunction even with normal sCr values and that mGFR is a useful tool for detecting early renal damage in SSc.
A total of 1038 patients (83.8% female) have been recruited in 9 studies and had their GFR measured or estimated. The mean GFR of these patients was 85.4 ml/min as shown in Table 1. Data regarding GFR categories (GFR < 90 ml/min and GFR < 60 ml/min) could be extracted from 5 studies with a total of 796 SSc patients. Out of those, 251(31.5%) had GFR < 90 ml/min whereas 155(19.5%) patients had GFR < 60 ml/min. These data indicate that renal dysfunction in SSc in not uncommon and therefore patients with SSc should have their renal function assessed by GFR estimation on a regular basis.
Most data indicate that CKD-EPI should be considered as the most suitable tool for assessing renal function in SSc pts, since it provides similar results to mGFR. Taking into account that direct GFR measurements are technically challenging and not available in everyday clinical practice, eGFR appears as an acceptable alternative and sensitive tool for early detection of renal impairment in SSc.
-
Renal Functional Reserve and SSc,
Renal Functional Reserve (RFR) is an established method of measuring kidney’s ability to increase GFR after an oral or intravenous amino acid load stimulation [24]. Under normal circumstances, GFR is increased following amino acid load (stimulated GFR) as a physiological response to protein loading. RFR is calculated as the percentile increase of stimulated GFR and the formula used is RFR = (stimulated GFR-baseline GFR)/baseline GFR × 100. RFR > 10% following protein loading is considered normal.
There are several studies that assessed whether RFR could be used as an alternative method to assess renal function in SSc. Amin et al. aimed at exploring whether RFR can detect preclinical nephropathy in SSc [25]. Thirty SSc pts with normal serum creatinine and 30 healthy controls were recruited. GFR was measured with Tc-99 m DTPA at baseline and following oral protein load. All controls had normal baseline GFR, stimulated GFR, RFR and urine protein levels. RFR was normal in only 6 Ssc pts. All SSc pts with PAH and most pts with disease duration over 4 years had abnormal RFR.
Livi et al. studied RFR fluctuation in 28 normotensive SSc pts with normal renal function (GFR > 70 ml/min), no history of diabetes and no urinary abnormalities over a 5-year period [26]. Abnormal RFR was found in 19 pts; these patients had a mean CCr reduction after 5 years of 15.4% compared to only 2.6% of those with normal RFR indicating that RFR may a strong predictor of future GFR decline.
Livi et al. also assessed RFR in patients with SSc compared to healthy subjects [27]. The investigators evaluated GFR, ERPF (effective renal plasma flow) and TRVR (total renal vascular resistance) prior to and following an amino acid load in 21 SSc pts and 10 healthy controls. The authors found that in controls GFR and ERPF were increased and TRVR was decreased after the load, as expected, whereas only 6 SSc pts managed to have a RFR comparable to that of the controls. More specifically, there was a 34.8% increase in GFR of controls as compared to only 1.9% increase in SSc pts. The analysis showed that low RFR was related to higher basal mean arterial pressure and shorter disease duration. These findings suggest that patients with SSc may have early renal involvement without signs or symptoms of clinically evident renal disease.
The above data point to the direction that RFR could be used as a sensitive tool for early detection of subclinical renal dysfunction in SSc. However, this method is technically challenging and time consuming, factors that limit its use in everyday clinical practice.
-
Do patients with SSc display significant proteinuria?
There are relatively limited data regarding proteinuria in SSc. Seiberlich et al. measured urine albumin and total protein excretion and performed urinary electrophoresis in 80 SSc pts and 18 healthy controls [28]. Albumin excretion rate (AER) was determined by measurement of the albumin-creatinine ratio (ACR) in the urine. Microalbuminuria was defined as 17 mg/g ≤ AER < 200 mg/g creatinine (for males) and 25 mg/g ≤ ACR < 300 mg/g creatinine (for females). Albuminuria (defined as at least microalbuminuria) was found in 20 pts (25%) and was correlated to increased systolic blood pressure (SBP) and disease duration. Fourteen pts (17.5%) had increased total protein excretion (200 mg/g creatinine) and this was correlated to pulmonary involvement. Protein composition in urine was evaluated by gel electrophoresis. The results were graded as: low molecular weight proteinuria (LMWP-excretion of albumin and proteins smaller than albumin), intermediate (IMWP- excretion of albumin and proteins larger than albumin but smaller than immunoglobulins) and high (HMWP- excretion of proteins including immunoglobulins). Abnormal electrophoresis was noted in 39 pts. No patient or control had HMWP but IMWP was found in 25 pts and was associated to gastrointestinal involvement, diffuse type of SSc and increased SBP. LMWP was found in 14 pts and 4 controls but had no correlations. This study showed that abnormal urinary protein excretion is common in SSc and therefore urinary dipsticks should be performed routinely in SSc pts to detect early renal involvement.
Schuster et al. investigated whether therapy with ACE-inhibitors was able to reverse the course of proteinuria in SSc patients during a 12-month period [29]. Proteinuria was evaluated with urine protein microelectrophoresis. All SSc patients (n = 31) had pathological urine microelectrophoresis and following treatment with an ACEI recession of proteinuria was found in 74% of patients, especially in those with recent onset proteinuria and shorter disease duration. The investigators showed that treatment with ACE inhibitors can reverse proteinuria in SSc pts. Whether this decrease may lead to better CVD outcomes needs to be further explored.
Discussion
SSc is the prototype systemic fibrotic disease that also has a significant vascular component. Rheumatologists focus on early detection of fibrotic manifestations such as interstitial lung disease [30, 31] or vascular manifestations such as pulmonary arterial hypertension or SRC because these manifestations largely dictate prognosis. However, comorbidities such as cardiovascular disease and renal dysfunction are often neglected in patients with SSc despite the fact that they may contribute to morbidity and mortality. In this literature review we found that 31.5% of patients with SSc have GFR < 90 ml/min, whereas 19.5% have GFR < 60 ml/min. Unfortunately, there are very limited data from comparative studies and therefore we cannot directly answer the question of whether renal function in SSc is significantly different compared to age- and sex-matched healthy controls. However, there are a lot of data regarding eGFR in the general population and an indirect comparison is feasible. In a large scale study of 7000 adults, it was shown that the percentage of subjects with GFR < 60 ml/min ranges from 2.1% to 6.9% depending on the predictive equation used [32]. Taking into account that our analysis showed that 19.5% of patients with SSc have GFR < 60 ml/min we may conclude that renal impairment appears more prominent in SSc compared to the general population. Perhaps, it would be more useful to explore whether patients with SSc have worse, similar or better renal function compared to patients with other chronic rheumatic diseases that do not primarily target the kidneys, such as RA. There are several studies that have assessed the prevalence of renal dysfunction in RA. Hickson et al. studied renal function in 813 RA patients compared to 813 controls and found that 9% had an eGFR < 60 ml/min [33]. Two other large scale studies assessing renal dysfunction in RA have shown that 8.8% [12] and 12.75% [11] of patients with RA have eGFR < 60 ml/min. These data indicate that patients with SSc may have worse renal function compared to patients with RA. However, definite conclusions cannot be drawn since studies directly comparing patients with RA and SSc do not exist.
In clinical practice, rheumatologists caring for patients with SSc mostly pay attention to pulmonary function tests, echocardiography and evolution of skin thickening but tend to neglect eGFR measurements and possible decline over time. Based on the results of our analysis, renal dysfunction in SSc is not uncommon; therefore, GFR estimation with CKD-EPI formula should be performed in every patient with SSc as a part of their routine follow-up. We have limited data regarding the main factors that associate with renal dysfunction in SSc; the few available studies have shown associations mostly with hypertension/cardiovascular disease. It is therefore reasonable to suggest that patients with SSc should be regularly subjected to cardiovascular risk assessment and receive appropriate treatment when indicated.
Data availability
All data are included in the current manuscript.
References
Cutolo M, Soldano S, Smith V (2019) Pathophysiology of systemic sclerosis: current understanding and new insights. Expert review of clinical immunology, vol 15. Taylor and Francis Ltd, Milton Park, pp 753–764
Smith V, Scirè CA, Talarico R, Airo P, Alexander T, Allanore Y et al (2018) Systemic sclerosis: State of the art on clinical practice guidelines. RMD Open, vol 4. BMJ Publishing Group, London, p 20
Asano Y (2020) The pathogenesis of systemic sclerosis: an understanding based on a common pathologic cascade across multiple organs and additional organ-specific pathologies. J Clin Med 9(9):2687
Barsotti S, Orlandi M, Codullo V, Di Battista M, Lepri G, Della RA et al (2019) One year in review 2019: systemic sclerosis. Clin Exp Rheumatol 119:S3-14
Denton CP, Khanna D (2017) Systemic sclerosis, vol 390. Lancet Publishing Group, London, pp 1685–1699
Steen VD, Medsger TA (2007) Changes in causes of death in systemic sclerosis, 1972–2002. Ann Rheum Dis 66(7):940–944
Bose N, Chiesa-Vottero A, Chatterjee S (2015) Scleroderma renal crisis. Seminars in arthritis and rheumatism, vol 44. W.B. Saunders, Philadelphia, pp 687–694
Perelas A, Silver RM, Arrossi AV, Highland KB (2020) Systemic sclerosis-associated interstitial lung disease. The Lancet respiratory medicine, vol 8. Lancet Publishing Group, London, pp 304–320
Anders HJ, Saxena R, Zhao-hui M, Parodis I, Salmon JE, Mohan C (2020) Lupus nephritis. Vol. 6. Nature Reviews Disease Primers. Nature Research
Binda V, Moroni G, Messa P (2018) ANCA-associated vasculitis with renal involvement. J Nephrol (Springer) 31:197–208
Daoussis D, Panoulas VF, Antonopoulos I, John H, Toms TE, Wong P et al (2010) Cardiovascular risk factors and not disease activity, severity or therapy associate with renal dysfunction in patients with rheumatoid arthritis. Ann Rheum Dis 69(3):517
Couderc M, Tatar Z, Pereira B, Tiple A, Gilson M, Fautrel B et al (2016) Prevalence of renal impairment in patients with rheumatoid arthritis: results from a cross-sectional multicenter study. Arthritis Care Res (Hoboken) 68(5):638–644
Vallianou NG, Mitesh S, Gkogkou A, Geladari E (2018) Chronic kidney disease and cardiovascular disease: is there any relationship? Curr Cardiol Rev 15(1):55–63
Amann K, Wanner C, Ritz E (2006) Cross-talk between the kidney and the cardiovascular system. J Am Soc Nephrol 17(8):2112–2119
Pagkopoulou E, Arvanitaki A, Daoussis D, Garyfallos A, Kitas G, Dimitroulas T (2019) Comorbidity burden in systemic sclerosis: beyond disease-specific complications. Rheumatol Int 39(9):1507–1517
Vart P, Grams ME (2016) Measuring and assessing kidney function. Seminars in nephrology (W.B. Saunders) 36: 262–72.
Caron M, Hudson M, Baron M, Nessim S, Steele R, Pope J et al (2012) Longitudinal study of renal function in systemic. J Rheumatol 39(9):1829–1834
Scheja A, Bartosik I, Wuttge DM, Hesselstrand R (2009) Renal function is mostly preserved in patients with systemic sclerosis. Scand J Rheumatol 38(4):295–298
Gupta R, Bammigatti C, Dinda AK, Marwaha V, Gupta S (2007) Prevalence of renal involvement in Indian patients with systemic sclerosis. Indian J Med Sci 61(2):91–96
Rosato E, Gigante A, Barbano B, Gasperini ML, Cianci R, Muscaritoli M (2018) Prognostic factors of renal involvement in systemic sclerosis. Kidney Blood Press Res 43(3):682–689
Suebmee P, Foocharoen C, Mahakkanukrauh A, Suwannaroj S, Theerakulpisut D, Nanagara R (2016) Correlation of glomerular filtration rate between renal scan and estimation equation for patients with scleroderma. Am J Med Sci 352(2):166–171
Gigante A, Rosato E, Massa R, Rossi C, Barbano B, Cianci R et al (2012) Evaluation of chronic kidney disease epidemiology collaboration equation to estimate glomerular filtration rate in scleroderma patients. Rheumatology 51(8):1426–1431
Mohamed RHA, Zayed HS, Amin A (2010) Renal disease in systemic sclerosis with normal serum creatinine. Clin Rheumatol 29(7):729–737
Jufar AH, Lankadeva YR, May CN, Cochrane AD, Bellomo R, Evans RG (2020) Renal functional reserve: From physiological phenomenon to clinical biomarker and beyond. Am J Physiol Regul Integr Comp Physiol 319:R690-702
Amin A, El-Sayed S, Taher N, Sedki M, Nasr H (2012) Tc-99m diethylenetriamine pentaacetic acid (DTPA) renal function reserve estimation: is it a reliable predictive tool for assessment of preclinical renal involvement in scleroderma patients. Clin Rheumatol 31(6):961–966
Livi R, Guiducci S, Perfetto F, Ciuti G, Grifoni E, Conforti L et al (2011) Lack of activation of renal functional reserve predicts the risk of significant renal involvement in systemic sclerosis. Ann Rheum Dis 70(11):1963–1967
Livi R, Teghini L, Pignone A, Generini S, Matucci-Cerinic M, Cagnoni M (2002) Renal functional reserve is impaired in patients with systemic sclerosis without clinical signs of kidney involvement. Ann Rheum Dis 61(8):682–686
Seiberlich B, Hunzelmann N, Krieg T, Weber M, Schulze-Lohoff E (2008) Intermediate molecular weight proteinuria and albuminuria identify scleroderma patients with increased morbidity. Clin Nephrol 70(2):110–117
Schuster J, Moinzadeh P, Kurschat C, Benzing T, Krieg T, Weber M et al (2013) Proteinuria in systemic sclerosis: reversal by ACE inhibition. Rheumatol Int 33(9):2225–2230
Daoussis D, Liossis S-N (2019) Treatment of systemic sclerosis associated fibrotic manifestations: current options and future directions. Mediterr J Rheumatol 30(1):33–37
Melissaropoulos K, Kraniotis P, Bogdanos D, Dimitroulas T, Sakkas L, Daoussis D (2019) Targeting very early systemic sclerosis: a case-based review. Rheumatol Int (Springer) 39:1961–1970
Trocchi P, Girndt M, Scheidt-Nave C, Markau S, Stang A (2017) Impact of the estimation equation for GFR on population-based prevalence estimates of kidney dysfunction. BMC Nephrol 18(1):341
Hickson LJ, Crowson CS, Gabriel SE, McCarthy JT, Matteson EL (2014) Development of reduced kidney function in rheumatoid arthritis. Am J Kidney Dis 63(2):206–213
Funding
No funding was provided.
Author information
Authors and Affiliations
Contributions
GI performed the literature search, statistical analysis and assisted in manuscript drafting. DD conceived the idea of the review, assisted in literature search and drafted the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
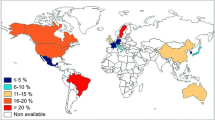
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iliopoulos, G., Daoussis, D. Renal dysfunction in systemic sclerosis beyond scleroderma renal crisis. Rheumatol Int 41, 1203–1208 (2021). https://doi.org/10.1007/s00296-021-04855-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-04855-x