Abstract
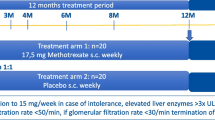
The objective of this study was to evaluate glucocorticoid (GC) use in patients with polymyalgia rheumatica (PMR), giant cell arteritis (GCA) or both diseases (PMR + GCA) under rheumatological care. Data from patients with PMR (n = 1420), GCA (n = 177) or PMR + GCA (n = 261) from the National Database of the German Collaborative Arthritis Centers were analyzed regarding GCs and related comorbidities (osteoporosis, diabetes and cardiovascular disease), stratified by disease duration (DD). Longitudinal data were analyzed for all patients with a DD ≤ 2 years at database entry (n = 1397). Three-year data were available for 256 patients. Predictors of GC use ≥ 3 years were examined by logistic regression analyses. A total of 76% received GCs, and 19% (PMR) to 40% (GCA) received methotrexate. Median GC doses were 12.5 mg (PMR), 11.3 mg (GCA), and 20.0 mg/day (PMR + GCA) in a 0–6-month DD. Median GC doses ≤ 5 mg/day were reached at a 13–18-month DD in PMR patients and at a 19–24-month DD in GCA or PMR + GCA patients. In the multivariate analysis, baseline methotrexate (OR 2.03, [95% CI 1.27–3.24]), GCs > 10 mg/day (OR 1.65, [1.07–2.55]), higher disease activity (OR 1.12, [1.02–1.23]) (median 0.6 years DD), and female sex (OR 1.63 [1.09–2.43]) were predictive for GC therapy at ≥ 3 years. Of the examined comorbidities, only osteoporosis prevalence increased within 3 years. GC use for ≥ 3 years was reported in one-fourth of all the patients. A difficult-to-control disease activity within the first year was a good predictor of long-term GC need.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polymyalgia rheumatica (PMR) and giant cell arteritis (GCA) are related inflammatory diseases that partially coexist [1]. Around one-fifth of patients with PMR have concomitant symptomatic GCA, while 40–60% of patients with GCA have features of PMR [2]. The treatment for both PMR and GCA is primarily based on glucocorticoids (GCs), which are initiated at different dosages and then (very) slowly tapered until cessation [1, 3, 4]. The European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) recommend GC treatment in PMR for a minimum of 12 months [3]. However, the available data from observational cohorts indicate that the mean duration of GC use in patients with PMR is approximately 2 years, with a wide range from 1 to more than 10 years [2, 5,6,7]. In GCA, higher starting doses are recommended, and the disease course is longer than in PMR, with a medium time between 2 and 3 years until permanent GC discontinuation [8, 9].
Long-term treatment with GCs is, however, associated with well-recognized adverse effects, such as GC-induced osteoporosis, metabolic and cardiovascular adverse effects and an increased risk for infection [2, 10]. Treatment with 10 mg/day of prednisone or equivalent for more than 3 months leads to a sevenfold increase in hip fractures and a 17-fold increase in vertebral fractures [11]. The risk ratio for glucocorticoid-induced diabetes is twofold in patients with older age, higher HbA1c level or lower glomerular filtration rates [12]. Overall, GC side effects occur in 50–65% of patients with PMR, thus representing a significant risk [3, 5].
The aim of the present study was to describe GC use and the related comorbidities in patients with PMR, GCA, and PMR + GCA in a large, nationwide German database, representing patients under routine rheumatologic care.
Patients and methods
Data source
The National Database of the German Collaborative Arthritis Centers is an ongoing prospective study that was established in 1993 as a long-term monitoring system for German Rheumatology. The database provides annually updated clinical data and rheumatologist- as well as patient-reported outcomes for unselected outpatients with inflammatory rheumatic diseases [13, 14]. Patients in routine rheumatological outpatient care from 15 participating arthritis centers are included, both from private practices and tertiary care centers. Patients treated entirely by general practitioners were not included.
The inclusion criteria for this study were rheumatologist-reported ICD-10 diagnoses of PMR (M35.3), GCA (M31.6), or PMR + GCA (M31.5/M35.3 + M31.6), and age ≥ 50 years at diagnosis. The exclusion criteria were suspected diagnoses or concomitant inflammatory diseases. Patients whose diagnosis changed to late-onset rheumatoid arthritis at a follow-up were also excluded from the study.
The database received study approval from the ethics committee of the Charité–University Medicine Berlin (EA1/196/06). Prior to enrolment, all the patients gave their informed consent.
Cross-sectional data collected annually between the years 2007 and 2014 were analyzed with regard to GC treatment, comorbidities and concomitant treatment. The patients were followed up as long as they attended the same arthritis center and did not withdraw consent to participate. Therefore, the longitudinal data were only available for a subset of the continuously treated patients. The cross-sectional data were stratified by disease duration, which was defined from the initial symptoms until the visit dates (0–6, 7–12, 13–18, 19–24 months, > 2–5 years, and > 5 years). The patients were documented each year that they were seen in the enrolling clinic, and thus, a patient can possibly be included in the different disease duration strata. If data from more than 1 year were available for the same patient within one stratum, then only the last dataset was included.
The longitudinal data are described separately, as available. For this analysis, only patients with a disease duration ≤ 2 years at baseline were selected. To account for the drop-out in the database (information on the cause is not available), the numbers of patients available for each follow-up year (year 0, year 1, year 2, and year 3) are reported.
Outcome assessment
The primary outcome was GC use with daily GC doses (current dose and the mean over the past 6 months in mg of prednisone equivalent per day). The secondary outcomes included the use of additional immunosuppressive agents, remission according to the clinical judgment of the rheumatologist (yes/no, not necessarily drug-free), disease activity [on a numerical rating scale (NRS) 0–10], erythrocyte sedimentation rate (ESR in mm/h), C-reactive protein (CRP in mg/dl), the presence of GC-related comorbidities (osteoporosis, diabetes, hypertension, cardiac disease) and related treatment (calcium and vitamin D substitutes, bisphosphonates). ESR and CRP measurements were performed under therapy. The rheumatologist reported all the outcomes.
In addition, age, sex, disease duration, smoking status (current/former/never), level of education (≤ 9, 10–13, and ≥ 14 years) and body mass index (BMI in kg/m2) were assessed as covariates.
Statistical analyses
Descriptive statistics (the mean with the standard deviation (SD) or the median with the interquartile range (IQR), expressed as percentages) were used to summarize the characteristics. The baseline characteristics were compared for the PMR group versus the GCA and the PMR + GCA group with the t-, Mann–Whitney or Fisher exact test, depending on the parameters; the p values were adjusted for two parallel tests. Univariate and multivariate logistic regression analyses with backward elimination were used to examine the association between the clinical variables at year 0 and GC use at ≥ 3 years. For this analysis, only patients enrolled until 2011, thus with the potential to be reported 3 years later, were included. Since we aimed at estimating the minimum number of patients who remain on GC therapy after 3 years, we considered patients without information after 3 years as non-users. A p value lower than 0.05 was considered statistically significant. The data were analyzed using IBM SPSS Statistics, version 23.
Results
Cross-sectional data
The data from 1858 patients, documented at least once in the years 2007 to 2014, were available for analysis. A total of 1420 patients had a PMR diagnosis, 177 patients had a GCA diagnosis, and 261 patients had PMR and GCA diagnoses. The mean age (73 years), median disease duration (2.8 years) and mean BMI (26.4 kg/m2) were comparable between the groups. Compared to the PMR patients, the patients with GCA and PMR + GCA were more often female. In addition, the patients with PMR + GCA were most often current smokers (Table 1).
At the time of the cross-sectional analysis, n = 1237 patients (76%) were treated with GCs. The proportion was comparable between the patients with PMR, GCA and PMR + GCA. Since the patients in the cross-sectional data varied considerably regarding their disease duration, the patients were stratified by disease duration from symptom onset (Fig. 1).
The median GC doses were 12.5 mg/day (PMR), 11.3 mg/day (GCA), and 20.0 mg/day (PMR + GCA) in patients with a disease duration of 0–6 months. The patients with PMR + GCA had the highest variability within the GC doses (minimum 2.5 mg/day to maximum 100 mg/day). The median GC doses ≤ 5 mg were achieved at 13–18 months in the PMR patients and at 19–24 months in the GCA and PMR + GCA patients. In all the groups, more than 70% of the patients with a disease duration > 2–5 years and more than 60% of the patients with a disease duration > 5 years received GCs. Their median GC dosages were 4.0 (PMR), 5.0 (GCA) and 4.0 mg/day (PMR + GCA) at > 2–5 years and 5.0 (PMR), 5.0 (GCA) and 3.0 mg/day (PMR + GCA) > 5 years.
Out of all the patients who were not treated with GCs (n = 397), n = 91 (23%) were treated with a synthetic or biological immunosuppressive agent. In total, n = 306 (19%) remained without any GC or immunosuppressive agent. These patients had a mean ESR of 22.7 mm/h, and 71% of them were considered as being in remission by the rheumatologist. Thus, regarding the entire sample set, n = 60 patients (6%) did not receive any immunosuppressive therapy, although they were not reported to be in remission.
Methotrexate was concomitantly used in 19% (PMR, n = 215) to 41% (GCA, n = 57) of the patients. Azathioprine (9%, n = 12) and leflunomide (5%, n = 7) were also used for the treatment of GCA. Biologics were rarely used (PMR 0.3%, GCA 0.7%, PMR + GCA 2.3%).
Of n = 1237 patients receiving GCs, n = 860 (70%) had calcium and vitamin D and n = 192 (20%) had bone densitometry measurement during the past 12 months.
The presence of GC-related comorbidities was stratified by disease duration and was standardized for age differences in the strata (Fig. 2). The frequency of osteoporosis was higher in the groups with a longer disease duration, while the frequency of diabetes was higher only in the patients with longstanding PMR + GCA. The frequency of hypertension and cardiac disease was not increased in the patients with longstanding disease.
Longitudinal data
To further examine GC use during the follow-up, longitudinal data are reported (if available) from the database entry (year 0) up to 3 years (Table 2). For this analysis, only patients with a disease duration ≤ 2 years at the first documentation (PMR, n = 922; GCA, n = 116, PMR + GCA, n = 172) were selected. Complete 3-year data were available for n = 172 (PMR), n = 30 (GCA) and n = 54 (PMR + GCA) patients.
The median GC doses ≤ 5 mg were achieved at year 1 (PMR) and at year 2 (GCA, PMR + GCA), but remained between 4 and 5 mg at year 3.
The median ESR and CRP values were in the normal range under immunosuppressive therapy. Five hundred and fifty-five patients with PMR (n = 555; 48%), 66 patients with GCA (n = 66; 61%) and 112 patients with PMR + GCA (n = 112; 34%) were in clinical remission at the first documentation (year 0). During the follow-up, 20–44% from all the patients remaining in the database did not achieve clinical remission.
Osteoporosis was reported in n = 76 (10%) of the PMR and PMR + GCA patients and in n = 17 (17%) of patients with GCA at year 0. At year 3, n = 30 (19%, PMR), n = 10 (20%, PMR + GCA) and n = 8 (30%, GCA) of all the patients remaining in the database had osteoporosis. A small increase was also observed when only patients with complete follow-up data were included (+ 3.7% in PMR, + 9.4% in PMR + GCA, + 8.6% in GCA). The prevalence of diabetes was marginally higher at follow-up, and a higher prevalence of hypertension was only observed in patients with PMR + GCA (Table 2).
Predictors of ongoing GC therapy at ≥ 3 years disease duration
In the univariate regression analysis, PMR + GCA diagnosis (odds ratio: OR 2.07), GCs > 10 mg/day (OR 1.94), methotrexate therapy (OR 1.75), disease activity assessed by NRS (OR 1.11), all at the database entry time point, and female sex (OR 1.52) were associated with GC therapy at ≥ 3 years disease duration. Smoking, BMI, cardiovascular or diabetes comorbidities, age and disease duration were not significantly associated.
In the multivariate analysis, baseline MTX therapy (OR 2.03), GCs > 10 mg/day (OR 1.65), higher disease activity (OR 1.12) and female sex (OR 1.63) remained predictive for GC therapy at ≥ 3 years disease duration (Table 3).
Discussion
Due to the low prevalence of PMR, GCA and PMR + GCA, the data on the duration of GC use in these diseases are scarce. We took advantage of a large dataset of patients treated in routine rheumatological care that were observed in the National Database of the Collaborative Arthritis centers in Germany.
In women, PMR was two-to-three times and GCA was three times more frequent than in men. The average age at disease onset was 69 years. Of all the patients with PMR, 17% also had symptomatic GCA, while 61% of the patients with GCA had concomitant PMR. These figures are in line with the epidemiological data reported in the literature [2].
GCs were used in more than 70% of all the patients with a disease duration above two years, and this was irrespective of having PMR, GCA or both diseases. This was confirmed by longitudinal data from all the patients who were followed for at least 3 years. We assumed that those patients who remained in rheumatological care still were in need of treatment, whereas a majority of those who were lost to follow up may have achieved GC-free remission after 3 years. If we estimate that all the patients who left the database had drug-free remission, we can calculate that at least 25% of all the patients observed at baseline used GCs after 3 years and 40% of those with both diseases. Considering the generally accepted treatment goals, the number of patients who failed to achieve GC-free remission was high. Chandran et al. reported that patients with GCA received GCs twice as long in the recent years (medium 2.6 years) compared to earlier decades (1.5 years). They assumed that low daily GC doses, at approximately 5 mg, were used for a longer time because of the awareness that the disease requires continuous treatment [8]. Cimmino et al. reported that one-third of patients with PMR had GCs for more than 6 years [7]. In the present study, the serological markers were in the normal range under immunosuppressive therapy, and thus, it remains unclear whether GCs were indeed necessary over the entire period.
Currently, there are no defined remission criteria for PMR and GCA. ESR remission and clinical remission, as reported by the rheumatologist, were not reached by all the patients. Even among the patients with a disease duration beyond 5 years, only half were reported to be in clinical remission. This percentage is high, given that the remission should be aimed for and that all patients were under ongoing rheumatologic care. The majority of the patients not in remission were actively treated.
Signs of a difficult-to-control disease activity within the first year (reflected by methotrexate use, failing to achieve low-dose GCs and remaining disease activity as reported by the rheumatologist) were associated with a higher risk to remain on GCs for 3 years and above. This observation underlines the need for alternative effective treatment modalities for this subset of patients. A recent cohort study of 131 patients with GCA showed comparable results, demonstrating that patients with long-term remission reached low-dose GCs faster than patients who were not in remission [15]. In a second report of the same cohort, the features of a high disease activity and higher cumulative GC doses were predictive of flaring in GCA patients [16].
Limited evidence supports the use of GC-sparing agents, such as methotrexate, for either PMR or GCA. Currently, only methotrexate is recommended in patients with early PMR in addition to GCs, particularly for those at high risk of relapse and/or prolonged therapy and during the follow-up of patients with a relapse, without a significant response to GC or those experiencing GC-related adverse events [3]. In the present study, methotrexate was only used in 19% of the patients with PMR and in 26% of those with PMR + GCA; other agents were rarely used. GCA patients without PMR were more frequently treated with methotrexate and other immunosuppressive agents. Methotrexate was associated with a higher probability of GC use in ≥ 3 years, indicating the need for intensive therapy in these patients. In the case series by Cimmino et al., which was also in patients on methotrexate therapy, almost one-third remained on GCs for more than 6 years [7].
TNF-alpha blocking agents have been shown to be ineffective for the treatment of PMR and/or GCA, but results from recent trials indicate that tocilizumab is an effective treatment in PMR and abatacept is effective for GCA therapy [17,18,19]. In the present study, abatacept was not used, and only two patients were on off-label tocilizumab.
NSAIDs are not recommended for PMR or GCA treatment apart from the possible short-term use of NSAIDs and/or analgesics in PMR patients with pain related to other conditions [3]. The reason for the concomitant NSAID use in PMR patients and for the frequent use of analgesics in GCA patients was not documented. Additionally, the use of aspirin was not documented specifically.
Cardiac comorbidity and diabetes showed no relevant increase during the follow-up, even in patients with more active disease. Since the GCs were tapered to ≤ 5 mg/day after 12 months in the patients with PMR and after 18 months in the patients with GCA or both diseases, this result supports the current practice of using GCs as a long-term immunosuppressive agent, provided that low-dose GC therapy is always the target to be achieved as soon as possible. This also conforms to a recent population-based cohort report that the presence of PMR and/or GCA was not associated with an increased risk of cardiovascular disease [20]. Cardiac disease and diabetes were reported in all the groups at similar frequencies, while hypertension was more frequently reported in the patients with PMR + GCA.
The prevalence of osteoporosis increased within 3 years, irrespective of having PMR and/or GCA. This increase was observed continuously from year 0 to year 3. Whether the GC therapy, a persisting disease activity or both, in addition to age, are primarily responsible for this remains unclear. In a large GCA cohort from a UK database, cumulative GC doses were associated with an osteoporosis comorbidity in GCA, supporting that GC use as risk factor for osteoporosis [21]. In the present cohort, prevention of GC-related osteoporosis by calcium and vitamin D supplementation was performed in the majority of patients but regular bone density measurements were performed only in one-fifth of patients with GC use. However, these data also show that causality cannot be demonstrated, and the distinction between GC use and GCA-related disease activity remains the major challenge. These results underline the need to explore novel therapeutic agents for effective PMR and GCA therapy in order to save on GCs and effectively suppress disease activity.
Limitations and strengths
Clinical diagnoses by the rheumatologists, reported as ICD-10 diagnoses, were used for the differentiation between PMR, GCA, and PMR + GCA. We cannot verify whether the diagnosis was based on the classification criteria, biopsies or imaging. The strength of the dataset is the large number of patients in a database, which has established a continuous comprehensive documentation for many years. Patients from private practices and tertiary care centers are included, representing real-life data from PMR/GCA provision in Germany. No significant differences were found regarding GC treatment and osteoporosis prophylaxis in secondary or tertiary care.
A selection bias is probable regarding the need of GCs. Patients who reach remission and who are able to terminate GCs are no longer in need of rheumatologic care and drop out of our observation. We addressed this issue by considering the dropout patients as GC non-users for the regression analysis, which resulted in the lowest possible estimate of continuous GC use. Further, we cannot account for patients who dropout due to serious events or death. Thus, the overall prevalence of GC use in the PMR patients can only be roughly estimated from our data. In addition, no data were reported regarding the initial inflammatory activity and the time interval between the onset of the symptoms, the initiation of the GC therapy and the GC starting doses. We also have no data on the cumulative GC doses, but other cohorts already addressed this topic [16, 21,22,23]. Infections are not reported in the NDB, therefore, they were not analysed although they belong to GC-related comorbidity.
Conclusion
In this cohort, GC use was frequent among patients with PMR, GCA and PMR + GCA with a disease duration above 2 years. It remains unknown whether PMR and/or GCA developed into a chronic stage in a subset of patients or whether GC therapy was continued at a low dose without definite clinical need. The predictors of long-term GC use rather support the need for more intensive and longer-lasting immunosuppressive therapies in these patients.
References
Buttgereit F, Dejaco C, Matteson EL, Dasgupta B (2016) Polymyalgia rheumatica and giant cell arteritis: a systematic review. JAMA 315:2442–2458
Matteson EL, Buttgereit F, Dejaco C, Dasgupta B (2016) Glucocorticoids for management of polymyalgia rheumatica and giant cell arteritis. Rheum Dis Clin North Am 42:75–90
Dejaco C, Singh YP, Perel P et al (2015) 2015 Recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Ann Rheum Dis 74:1799–1807
Dasgupta B, Borg FA, Hassan N et al (2010) BSR and BHPR guidelines for the management of giant cell arteritis. Rheumatology (Oxford) 49:1594–1597
Gabriel SE, Sunku J, Salvarani C, O’Fallon WM, Hunder GG (1997) Adverse outcomes of antiinflammatory therapy among patients with polymyalgia rheumatica. Arthritis Rheum 40:1873–1878
Narvaez J, Nolla-Sole JM, Clavaguera MT, Valverde-Garcia J, Roig-Escofet D (1999) Longterm therapy in polymyalgia rheumatica: effect of coexistent temporal arteritis. J Rheumatol 26:1945–1952
Cimmino MA, Salvarani C, Macchioni P et al (2008) Long-term follow-up of polymyalgia rheumatica patients treated with methotrexate and steroids. Clin Exp Rheumatol 26:395–400
Chandran A, Udayakumar PD, Kermani TA, Warrington KJ, Crowson CS, Matteson EL (2015) Glucocorticoid usage in giant cell arteritis over six decades (1950 to 2009). Clin Exp Rheumatol 33(2 Suppl 89):S-102
Proven A, Gabriel SE, Orces C, O’Fallon WM, Hunder GG (2003) Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Rheum 49:703–708
Van der Goes MC, Jacobs JW, Boers M et al (2010) Patient and rheumatologist perspectives on glucocorticoids: an exercise to improve the implementation of the European League Against Rheumatism (EULAR) recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis 69:1015–1021
Mazzantini M, Di Munno O (2014) Glucocorticoid-induced osteoporosis: 2013 update. Reumatismo 66:144–152
Katsuyama T, Sada KE, Namba S et al (2015) Risk factors for the development of glucocorticoid-induced diabetes mellitus. Diabetes Res Clin Pract 108:273–279
Albrecht K, Huscher D, Richter J, Backhaus M, Bischoff S, Kotter I et al (2014) Change in referral, treatment and outcomes in patients with systemic lupus erythematosus in Germany in the 1990s and the 2000s. Lupus Sci Med 1:e000059
Huscher D, Thiele K, Rudwaleit M, Albrecht KC, Bischoff S, Krause A et al (2015) Trends in treatment and outcomes of ankylosing spondylitis in outpatient rheumatological care in Germany between 2000 and 2012. RMD Open 1:e000033
Restuccia G, Boiardi L, Cavazza A et al (2017) Long-term remission in biopsy proven giant cell arteritis: a retrospective cohort study. J Autoimmun 77:39–44
Restuccia G, Boiardi L, Cavazza A et al (2016) Flares in biopsy-proven giant cell arteritis in Northern Italy: characteristics and predictors in a long-term follow-up study. Medicine (Baltimore) 95:e3524
Lally L, Forbess L, Hatzis C, Spiera R (2016) Brief report: a prospective open-label phase IIa trial of tocilizumab in the treatment of polymyalgia rheumatica. Arthritis Rheumatol 68:2550–2554
Devauchelle-Pensec V, Berthelot JM, Cornec D et al (2016) Efficacy of first-line tocilizumab therapy in early polymyalgia rheumatica: a prospective longitudinal study. Ann Rheum Dis 75:1506–1510
Langford CA, Cuthbertson D, Ytterberg SR et al (2017) A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of giant cell arteritis. Arthritis Rheumatol 69:837–845
Pujades-Rodriguez M, Duyx B, Thomas SL, Stogiannis D, Smeeth L, Hemingway H (2016) Associations between polymyalgia rheumatica and giant cell arteritis and 12 cardiovascular diseases. Heart 102:83–89
Petri H, Nevitt A, Sarsour K, Napalkov P, Collinson N (2015) Incidence of giant cell arteritis and characteristics of patients: data-driven analysis of comorbidities. Arthritis Care Res (Hoboken) 67:390–395
Kremers HM, Reinalda MS, Crowson CS, Zinsmeister AR, Hunder GG, Gabriel SE (2005) Relapse in a population based cohort of patients with polymyalgia rheumatica. J Rheumatol 32:65–73
Hernandez-Rodriguez J, Cid MC, Lopez-Soto A, Espigol-Frigole G, Bosch X (2009) Treatment of polymyalgia rheumatica: a systematic review. Arch Intern Med 169:1839–1850
Acknowledgements
The authors gratefully acknowledge the contributions and the enthusiasm of all the participating patients and consultant rheumatologists who contributed data to the National Database. The authors would like to acknowledge the significant contributions of R. Alten (Berlin), M. Backhaus (Berlin), H. Burkhardt (Frankfurt/Main), S. Kleinert and J. Wendler (Erlangen), T. Eidner (Jena), K. Fischer (Greifswald), J. Henes (Tübingen), U. von Hinüber (Hildesheim), K. Karberg (Berlin), I. Kötter (Hamburg), A. Krause (Berlin), S. Späthling-Mestekemper (München), J. Richter (Düsseldorf), S. Wassenberg and R. Weier (Ratingen).
Author information
Authors and Affiliations
Contributions
DH had full access to all data of this study and take responsibility for data integrity and accuracy of the analysis. KA, DH, FB and AZ: study concept and design. MA, GH, WO and KT: acquisition of the data. KA, DH, FB, MA and AZ: analysis and interpretation of the data. KA and DH: drafting the manuscript. All authors critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Funding
The database is funded by unconditional grants from the German Collaborative Arthritis Centers and from a consortium of 11 pharmaceutical companies to the German Academy for Continuing Medical Education in Rheumatology. The principal investigators and their team had full academic freedom in the study design and conduct, data analysis and publication of the results.
Conflict of interest
M.A. is an investigator in a tocilizumab trial of GCA. F.B. reported receiving consultancy fees, honoraria and travel expenses from Horizon Pharma (formerly Nitec Pharma) and Mundipharma Int Ltd and grant support from Horizon Pharma. In addition, he serves as co-principal investigator and site investigator in a Mundipharma sponsored trial in PMR investigating the effects of MR prednisone. None of the other authors have conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Katinka Albrecht and Dörte Huscher contributed equally to this work.
Rights and permissions
About this article
Cite this article
Albrecht, K., Huscher, D., Buttgereit, F. et al. Long-term glucocorticoid treatment in patients with polymyalgia rheumatica, giant cell arteritis, or both diseases: results from a national rheumatology database. Rheumatol Int 38, 569–577 (2018). https://doi.org/10.1007/s00296-017-3874-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3874-3