Abstract
The purpose of this study was to identify a gene expression signature in osteoarthritis (OA) synovium and genomic pathways likely to be involved in the pathogenesis of OA. Four publicly accessible microarray studies from synovium of OA patients were integrated, and a transcriptomic and network-based meta-analysis was performed. Based on pathways according to the Kyoto Encyclopedia of Genes and Genomes, functional enrichment analysis was performed. Meta-analysis results of OA synovium were compared to two previously published studies of OA cartilage to determine the relative number of common and specific DEGs of the cartilage and synovium. According to our meta-analysis, a total of 1350 genes were found to be differentially expressed in the synovium of OA patients as compared to that of healthy controls. Pathway analysis found 41 significant pathways in the total DEGs, and 22 and 16 pathways in the upregulated and downregulated DEGs, respectively. Cell adhesion molecules and cytokine–cytokine receptor interaction were the most significant pathway in the upregulated and downregulated DEGs, respectively. Comparison of meta-analysis results of OA synovium with results of two previous studies of OA cartilage identified 85 common genes and 1632 cartilage-specific DEGs and 1265 synovium-specific DEGs in the first study; and 142 common genes, and 856 cartilage-specific DEGs and 1208 synovium-specific DEGs in the second study. Our results show a small overlap between the DEGs of the synovium compared to DEGs of the cartilage, suggesting different pathogenic mechanisms that are specific to the synovium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most common joint disease characterized by cartilage degradation, the formation of osteophytes, subchondral bone sclerosis and synovial inflammation, consequently resulting in joint pain, stiffness and functional disability [1, 2]. OA has been considered a disease of purely mechanical cartilage degeneration for a long time; therefore, research has mainly focused on the compositional and structural alterations of articular cartilage and the dysregulated functions of chondrocyte [3]. However, recent evidences support that OA affects not only articular cartilage, but also all of the joint structures, including synovium, bone, ligaments and meniscus, indicating that OA is a whole joint disease [4]. Furthermore, inflammation was regarded to play a critical role in the pathogenesis of OA, by contributing to cartilage degradation and synovial cell activation [5, 6]. Systemic and local production of inflammatory cytokines, activation of complement and innate immune response are involved in the inflammation of OA. There are increasing evidences that synovial inflammation is associated with greater symptoms such as pain and joint dysfunctions and structural progression of OA, indicating that synovitis is an integral component of OA pathogenesis [2, 4, 7]. Over the last decade, research focus has turned to the important role of synovitis in the pathogenesis of OA.
Gene expression profiling with microarrays has become a promising approach for identifying the changes underlying the initiation and progression of complex disease such as OA and discovering biomarkers for diagnosis, disease activity and response to treatment [8, 9]. A number of microarray studies have previously been undertaken in OA [10–19]. Although all these studies have successfully identified the differentially expressed genes (DEGs), the expression profiles identified in these studies were not consistent with each other, and DEGs reported in each study had little overlap. Furthermore, most of these studies focused on cartilage and peripheral blood of OA patients. Therefore, in this study, we integrated four publicly accessible microarray studies from synovium of OA patients and performed a transcriptomic and network-based meta-analysis to identify a gene expression signature and genomic pathways likely to be involved in the pathogenesis of OA.
Methods
Data collection
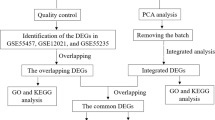
Microarray datasets were obtained from the Gene Expression Omnibus (GEO) at the National Center for Biotechnology Information (NCBI) by using the terms “osteoarthritis” on August 1, 2015. Studies were included in the analysis if they met the following criteria: (1) case–control studies, (2) studies containing gene expression data of synovium and (3) studies including patients diagnosed with OA. Ten microarray datasets, including GSE1919, GSE12021, GSE32317, GSE36700, GSE39340, GSE41038, GSE46750, GSE55235, GSE55457 and GSE55584, were identified by fulfilling the inclusion criteria (Fig. 1). GSE12021 was excluded because data in GSE12021 were overlapped with data in GSE55457. GSE32317, GSE36700, GSE39340, GSE46750 and GSE55584 were excluded due to the absence of healthy control in dataset. Finally, a total of four microarray studies that used synovium (GSE1919, GSE41038, GSE55235 and GSE55457) were considered for subsequent analysis.
Meta-analysis and network-based analysis
We followed the guideline provided by Ramasamy et al. [20] for meta-analysis of gene expression microarray. To integrate the results of individual studies and obtain a list of more robust DEGs in synovium between OA patients and healthy controls, we conducted a microarray meta-analysis using NetworkAnalyst, a web interface for the integrative analysis of gene expression data [21]. The optimum method for generating overlapping gene lists between heterogeneous studies has been suggested to use a ranked fold change (FC) analysis, which ignored the absolute degree of observed change; therefore, we used combing rank orders algorithm, with 20 times of permutation tests for meta-analysis [22]. The combining rank orders algorithm is a nonparametric approach based on ranks of FCs. In this approach, ratios of FCs are computed for all possible pairwise comparisons for each dataset and the resulting ranks are used to calculate the rank product for each gene. The entire process is repeated multiple times to derive a p value and false discovery rate for each gene [21]. After identification of DEGs, we performed network analysis using NetworkAnalyst. The DEGs identified from meta-analysis were presented within protein–protein interaction (PPI) networks to extract enriched functional pathways based on the Kyoto Encyclopedia of Genes and Genomes (KEGG) database. We used a PPI database based on InnateDB, which currently contains 14,755 proteins and 145,955 interactions for human [23]. The properties of nodes in network were displayed as hub degree and betweenness values. The degree centrality of hub is the number of connections that a node has to other nodes, whereas betweenness centrality represents to the number of shortest paths passing through the node [21].
Results
Study characteristics
This study includes four publicly accessible microarray datasets that examined synovium from OA patients. Detailed information of these four datasets is described in Table 1 [16, 24]. These datasets included a total of 28 patients with OA and 29 healthy controls. The demographic data of patients are summarized in Supplementary Table 1.
Analysis of gene expression profile in synovium of OA patients
To identify a common transcriptional signature in synovium of OA patients, four microarray datasets including GSE1919, GSE41038, GSE55235 and GSE55457 were analyzed using NetworkAnalyst. We selected the DEGs with p value <0.05. Meta-analysis using combing rank orders identified a total of 1350 genes to be differentially expressed between OA patients and healthy controls across microarray datasets. Among the 1350 DEGs, 693 genes were upregulated and 657 genes were downregulated in OA patients compared with healthy controls. The top 10 most significantly upregulated genes are SCRG1, IGJ, MMP1, CX3CR1, TAC1, NELL1, CSN1S1, LRRC15, GPR1 and MXRA5, and the top 10 most significantly downregulated genes are IL8, CYP4B1, DDIT4, CXCL2, DDX3Y, MAFF, RPS4Y1, FOSB, FKBP5 and APOD (Table 2). The complete list of DEGs is provided in Supplementary Table 2.
More recently, to examine whether genes identified by genome wide association study (GWAS) of OA patients are dysregulated in the cartilage of OA patients, differential expressions of these OA susceptibility genes were screened in a list of DEGs between the OA affected and preserved cartilage [15]. We also screened these genes in our list of DEGs in synovium of OA patients. Nine of 30 genes selected were differentially expressed in synovium between OA patients and healthy controls (Table 3). These nine OA susceptibility genes identified in synovium had little overlap with previous reported 8 genes different between OA and preserved cartilage.
Network analysis of DEGs in synovium of OA patients
To identify the overrepresented biological pathway dysregulated in synovium of OA patients, we conducted a network-based analysis of these 1350 significant OA genes using NetworkAnalyst. The resulting zero-order interaction network (composed only of the seed nodes and the edges that interconnect them) contained 640 nodes and 1379 edges. The complete list of nodes in the obtained network is provided in supplementary Table 3. HSP90AA1, EGR1, JUN, MYC, EGFR, CEBPB, PIK3R1, FOS, CDKN1A and ARRB2 were identified as potential hub genes in synovium of OA patients by hub explorer in NetworkAnalyst. Next, we identified enriched functional pathways within the obtained network by conducting pathway analysis based on KEGG database. We identified 41 significant pathways in the pathway analysis (Supplementary Table 4). For the upregulated DEGs, 16 significant functional pathways were identified to be enriched, and the most significant pathway was cell adhesion molecules (CAMs; Table 4 and Supplementary Table 5). For the downregulated DEGs, 22 significant functional pathways were identified to be enriched, and the most significant pathway was cytokine–cytokine receptor interaction (Table 4 and Supplementary Table 6).
Comparison between the results of previous microarray studies in OA cartilage and our meta-analysis results in OA synovium
Our meta-analysis results in OA synovium were compared to the results of two previous microarray studies by Ramos et al. [15] and by Xu et al. [17] in OA cartilage in order to find commonly regulated as well as differentially regulated genes. First, comparison of the upregulated DEGs in the study by Ramos et al. revealed 705 genes in the OA cartilage versus 650 genes in the OA synovium; 43 genes were found to be in common. Comparison of the downregulated DEGs showed 927 genes in the OA cartilage versus 615 genes in the OA synovium; 42 genes were found to be in common. Second, comparison of the upregulated DEGs in the study by Xu et al. showed 419 genes in the OA cartilage versus 647 genes in the OA synovium; 46 genes were found to be in common. Comparison of the downregulated DEGs showed 437 genes in the OA cartilage versus 561 genes in the OA synovium; 96 genes were found to be in common. The list of commonly regulated genes is presented in Supplementary Figs. 1 and 2.
Discussion
Our study is the first meta-analysis to integrate previous microarray analyses comparing OA synovium to healthy synovium. Our meta-analysis found 1350 DEGs that were enriched in the OA synovium. Of these, 693 genes were upregulated and 657 genes were downregulated in the OA synovium compared to in the healthy synovium. When these DEGs were screened in a list of genes found in a recent GWAS study, identified 9 genes were found to be matched. Pathway analysis of total DEGs revealed 41 significant pathways and separate pathway analyses of upregulated and downregulated DEGs found 16 and 22 pathways, respectively. The most significant pathway enriched in upregulated DEGs was CAMs, whereas the most significant pathway enriched in downregulated DEGs was cytokine–cytokine receptor interactions.
CAMs are integral to the pathogenesis of inflammatory disorders such as rheumatoid arthritis (RA) and systemic lupus erythematosus, as they play important parts in innate and adaptive immune responses. Notably, VCAM-1, which is known to be expressed in inflamed blood vessel endothelium and whose ligand is expressed on effector T cells and monocytes, was enriched in the upregulated DEGs. Consistent with this result, a past study has shown the protein levels of VCAM-1 to be upregulated in the articular blood vessels of pathologic tissue as well as the synovium of OA patients compared to healthy controls [25]. Furthermore, increased levels of serum VCAM-1 have been found in patients with erosive hand OA and have also been found to be predictive of severe hip and knee joint OA. Together, these findings add further evidence that inflammation indeed plays an important role in OA pathogenesis [26, 27]. Moreover, our analysis has identified other CAMs such as ITGB2 (CD18), ITGAL (CD11a) and CD2 (LFA-2) which have yet to be studied in OA; therefore, our results warrant further research into the possible role of these molecules in the pathogenesis of OA.
Although cytokine–cytokine receptor interactions were enriched in both the upregulated and downregulated DEGs, what was striking was that when the nature of the cytokines in each fraction was considered, pro-inflammatory cytokines were mostly among the downregulated DEGs. IL-1β, TNF-α and IL-6 are thought to be the most important cytokines mediating synovitis in OA, with IL-15, IL-17, IL-18, IL-21, LIF also thought to be contributing [28]. However, according to our results, IL-1β and IL-6 were found to be downregulated in the OA synovium compared to in the healthy synovium. Cartilage, synovium and subchondral bone are all thought to contribute to inflammatory cytokine production but just how much each component contributes has been unclear. Our findings suggest that the synovium is not a major site of pro-inflammatory cytokine production in OA. Indeed, the concentration of cytokines such as IL-1α, IL-1β, TNF-α, IL-6, IFN-γ and OSM has been found to be markedly higher in the cartilage than in the synovial fluid [29].
Although most pro-inflammatory cytokines were found to be downregulated in the OA synovium, a few were found to be upregulated such as IL-18. While IL-18 is expressed by cells of the immune system such as dendritic cells and monocytes, they are also expressed by non-immune cells such as synovial fibroblasts [30]. Furthermore, IL-18 receptor (IL-18R) is widely expressed on cells of the innate and adaptive immune systems [31]. Importantly, IL-18 has been shown to induce TNF-α and to a lesser extent, IL-6 in mononuclear cells, suggesting that it may be a candidate cytokine by which the synovium contributes to inflammation in the joint [32, 33]. In RA synovium, IL-18 has been shown to be involved in a positive feedback loop in which IL-18 induces pro-inflammatory cytokines such as TNF-α and IFN-γ that maintain synovial inflammation [31]. If IL-18 is driving inflammation in the OA synovium as in RA synovium, it is understandable why pharmacologic therapies targeting TNF-α showed results that were less effective than expected, as IL-18 may be acting upstream to maintain inflammation regardless of TNF-α blockage. IL-18 has also been shown to induce angiogenesis in RA synovium [34], suggesting it may be a candidate cytokine contributing to synovial angiogenesis in OA. However, further studies are required to demonstrate that the concentration of IL-18 in the OA synovium is sufficient to induce angiogenesis. Stimulation of human articular cartilage with culture containing IL-18 was shown to induce proteoglycan breakdown [35], suggesting that the synovium may be contributing to matrix breakdown in the cartilage via IL-18 production. Also, IL-18 levels in the plasma, cartilage and synovial fluid are correlated with radiographic severity in OA of the knee [36], suggesting that IL-18 indeed does contribute to OA pathology. Taking these results into account, IL-18 is a potential target for pharmacological treatment. Interestingly, IL-18-targeting therapies have shown successful results in animal models of chronic inflammatory disorders and have currently entered clinical trials for the treatment of psoriasis and RA. Therefore, IL-18 may provide a novel avenue of research in OA treatment.
Our study showed an interesting chemokine profile in the OA synovium compared to in the healthy synovium. Among the chemokines upregulated in the synovium were IP-10/CXCL10 and CCL5, while among those that were downregulated was IL-8/CXCL8. IFN-γ has been shown to upregulate IP-10/CXCL10 and CCL5 and downregulate IL-8/CXCL8 [37], suggesting that IFN-γ may be a key regulatory cytokine acting on the synovium. While IFN-γ has also been shown to upregulate CCL13, our results showed CCL13 was downregulated in the synovium [37]. However, IFN-γ induces CCL13 mainly in the cartilage, which suggests that the set of chemokines induced by IFN-γ may be tissue dependent. CXCL1, ENA-78/CXCL5 and IL-8/CXCL8 are thought to be the primary inflammatory chemokines in the RA synovium [37]. According to our study, however, CXCL1 and IL-8/CXCL8 were found to be downregulated in the OA synovium. These results elucidate a possible inflammatory chemokine signature in the OA synovium that is distinct from that in the RA synovium.
Studies have demonstrated angiogenesis to be increased in the OA synovium [38]. Angiogenesis is regulated by a balance between angiogenic and angiostatic factors. Importantly, among these regulatory factors, chemokines have shown angiogenic and angiostatic properties [37]. Among known angiogenic chemokines are CXCL-1, IL-8/CXCL8 and SDF-1/CXCL12, while among known angiostatic chemokines are IP-10/CXCL10 [37]. Interestingly, CXCL-1, IL-8/CXCL8 and CXCL2 were among the DEGs that were downregulated, and IP-10/CXCL10 and SDF-1/CXCL12 were among those that were upregulated. Considering that CXCL-1 and IL-8/CXCL8 are angiogenic chemokines and IP-10/CXCL10 is an angiostatic chemokine, they were ruled out as possible candidates involved in contributing to synovial angiogenesis. However, SDF-1/CXCL12 was found to be upregulated in the synovium, suggesting that SDF-1/CXCL12 may be a candidate chemokine involved in synovial angiogenesis. Furthermore, SDF-1/CXCL12 has been shown to induce apoptosis and induce matrix metalloproteinase-1 (MMP-1), MMP-3, MMP-9 and MMP-13 in chondrocytes [39]. However, while CXCR4, a receptor for SDF-1/CXCL12, is expressed in chondrocytes, SDF-1/CXCL12 is not produced by chondrocytes [39], suggesting that SDF-1/CXCL12 is produced in the synovium and acting on the cartilage, which in turn suggests that there is synovium–cartilage interaction which is exacerbating matrix breakdown in the cartilage. Notably, CXCR4 blocking therapies have been proposed as promising candidates for the treatment of rheumatic diseases such as RA and OA [39].
Our results show that Wnt1-inducible signaling pathway protein 3 (WISP-3) was upregulated in the OA synovium as compared to in the healthy synovium. The Wnt/β-catenin signaling pathway was shown to be upregulated in experimental OA models of mice, and stimulation of cultured macrophages and chondrocytes with recombinant WISP-1 has been shown to induce several MMPs and aggrecanase in an IL-1-independent manner [40]. Interestingly, WISP-3 has been shown to induce MMP1 and MMP10 [41]. Taking into account that MMP1, MMP3, MMP9 and MMP13 were upregulated in the synovium, WISP3 may be targeted to potentially reduce matrix degradation in OA.
Interestingly, TNFSF11B and TNFRSF11B were upregulated in the OA synovium. While both are involved in the differentiation of osteoclasts, one’s function opposes the other [42]. In particular, increased TNFRSF11B activity has been shown to lead to OA development.
DEGs identified in the OA synovium in our study were directly compared in the list of genes dysregulated in OA cartilage [15, 17]. We reasoned the overlapping genes may be involved in a pathogenic mechanism common to both tissues, while non-overlapping genes may be involved in pathogenic mechanisms specific to each tissue. Our analysis revealed that non-overlapping genes clearly outnumbered overlapping genes, suggesting different pathogenic mechanisms are at play in the synovium as opposed to in the cartilage. For example, in OA cartilage, MMP13 and ADAMTS5 are important matrix metalloproteinases involved in matrix degradation in the cartilage, in which the main component is type II collagen. However, ADAMTS5 and type II collagen (COL2A1) were not among the DEGs in OA synovium, suggesting that this key pathogenic mechanism in the cartilage does not play an important role in the synovium. Although low in number, overlapping genes revealed certain pathogenic mechanisms that may be common in the cartilage and the synovium. Superoxide dismutase-2 (SOD2) was found to be a gene downregulated in common in the OA synovium and in the OA cartilage. Downregulation of SOD2 leads to a decrease in oxidoreductase activity, which in turn leads to an increased ROS burden in the synovium, which has been demonstrated in OA [17]. Similar to the downregulation of AKT3 in OA cartilage, AKT2 was downregulated in OA synovium. The decrease in AKT2 may have protective effects in the synovium as depletion of AKT3 in chondrocytes has been shown to result in reduction of MMP13 expression [43]. MYC expression, which leads to chondrocyte apoptosis, is downregulated in OA cartilage as well as in OA synovium. ATF3 was also found to be downregulated in both the OA cartilage and OA synovium. In cartilage, reduced ATF3 expression is thought to decrease responsiveness of chondrocytes to stimuli but its role in the synovium has yet to be elucidated.
The strength of our study lies in that we find evidence for distinct pathogenic mechanisms within the OA synovium as opposed to within the OA cartilage for example. Notably, our results suggest that the synovium is probably not a main producer of pro-inflammatory cytokines as previously thought. Furthermore, we suggest novel molecular targets such as WISP3 that may have potential therapeutic benefit. On the other hand, our study was limited by the number of studies and the number of total specimens. Moreover, our study is limited by the potential heterogeneity in the synovial samples of the OA patients. A previous study has shown that there is significant difference in the gene expression profile of inflamed areas of the synovial lining compared to normal or reactive areas of the lining in the same OA patient [13]. However, despite this heterogeneity, our analysis discovered CAMs to be enriched in the upregulated DEGs and cytokines such as IL-1 and IL-6 to be enriched in the downregulated DEGs. Future gene expression studies in OA synovium should validate the results of our studies.
In conclusion, our study shows a distinct gene expression profile in OA synovium compared to in healthy synovium and demonstrates distinct genes and pathways enriched in OA synovium versus OA cartilage.
References
Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, Carr AJ (2015) Osteoarthritis. Lancet 386(9991):376–387. doi:10.1016/S0140-6736(14)60802-3
Sellam J, Berenbaum F (2010) The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol 6(11):625–635. doi:10.1038/nrrheum.2010.159
Goldring MB, Goldring SR (2010) Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis. Ann NY Acad Sci 1192:230–237. doi:10.1111/j.1749-6632.2009.05240.x
Scanzello CR, Goldring SR (2012) The role of synovitis in osteoarthritis pathogenesis. Bone 51(2):249–257. doi:10.1016/j.bone.2012.02.012
Berenbaum F (2013) Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthritis Cartilage 21(1):16–21. doi:10.1016/j.joca.2012.11.012
Pap T, Korb-Pap A (2015) Cartilage damage in osteoarthritis and rheumatoid arthritis-two unequal siblings. Nat Rev Rheumatol. doi:10.1038/nrrheum.2015.95
Attur M, Samuels J, Krasnokutsky S, Abramson SB (2010) Targeting the synovial tissue for treating osteoarthritis (OA): where is the evidence? Best Practice Res Clin Rheumatol 24(1):71–79. doi:10.1016/j.berh.2009.08.011
Bauer JW, Bilgic H, Baechler EC (2009) Gene-expression profiling in rheumatic disease: tools and therapeutic potential. Nat Rev Rheumatol 5(5):257–265. doi:10.1038/nrrheum.2009.50
Haupl T, Stuhlmuller B, Grutzkau A, Radbruch A, Burmester GR (2010) Does gene expression analysis inform us in rheumatoid arthritis? Ann Rheum Dis 69(Suppl 1):i37–i42. doi:10.1136/ard.2009.119487
Attur M, Belitskaya-Levy I, Oh C, Krasnokutsky S, Greenberg J, Samuels J, Smiles S, Lee S, Patel J, Al-Mussawir H, McDaniel G, Kraus VB, Abramson SB (2011) Increased interleukin-1beta gene expression in peripheral blood leukocytes is associated with increased pain and predicts risk for progression of symptomatic knee osteoarthritis. Arthritis Rheum 63(7):1908–1917. doi:10.1002/art.30360
Geyer M, Grassel S, Straub RH, Schett G, Dinser R, Grifka J, Gay S, Neumann E, Muller-Ladner U (2009) Differential transcriptome analysis of intraarticular lesional vs intact cartilage reveals new candidate genes in osteoarthritis pathophysiology. Osteoarthritis Cartilage 17(3):328–335. doi:10.1016/j.joca.2008.07.010
Karlsson C, Dehne T, Lindahl A, Brittberg M, Pruss A, Sittinger M, Ringe J (2010) Genome-wide expression profiling reveals new candidate genes associated with osteoarthritis. Osteoarthritis Cartilage 18(4):581–592. doi:10.1016/j.joca.2009.12.002
Lambert C, Dubuc JE, Montell E, Verges J, Munaut C, Noel A, Henrotin Y (2014) Gene expression pattern of cells from inflamed and normal areas of osteoarthritis synovial membrane. Arthritis Rheumatol 66(4):960–968. doi:10.1002/art.38315
Ramos YF, Bos SD, Lakenberg N, Bohringer S, den Hollander WJ, Kloppenburg M, Slagboom PE, Meulenbelt I (2014) Genes expressed in blood link osteoarthritis with apoptotic pathways. Ann Rheum Dis 73(10):1844–1853. doi:10.1136/annrheumdis-2013-203405
Ramos YF, den Hollander W, Bovee JV, Bomer N, van der Breggen R, Lakenberg N, Keurentjes JC, Goeman JJ, Slagboom PE, Nelissen RG, Bos SD, Meulenbelt I (2014) Genes involved in the osteoarthritis process identified through genome wide expression analysis in articular cartilage; the RAAK study. PLoS One 9(7):e103056. doi:10.1371/journal.pone.0103056
Woetzel D, Huber R, Kupfer P, Pohlers D, Pfaff M, Driesch D, Haupl T, Koczan D, Stiehl P, Guthke R, Kinne RW (2014) Identification of rheumatoid arthritis and osteoarthritis patients by transcriptome-based rule set generation. Arthritis Res. Ther 16(2):R84. doi:10.1186/ar4526
Xu Y, Barter MJ, Swan DC, Rankin KS, Rowan AD, Santibanez-Koref M, Loughlin J, Young DA (2012) Identification of the pathogenic pathways in osteoarthritic hip cartilage: commonality and discord between hip and knee OA. Osteoarthritis Cartilage 20(9):1029–1038. doi:10.1016/j.joca.2012.05.006
Wang Q, Rozelle AL, Lepus CM, Scanzello CR, Song JJ, Larsen DM, Crish JF, Bebek G, Ritter SY, Lindstrom TM, Hwang I, Wong HH, Punzi L, Encarnacion A, Shamloo M, Goodman SB, Wyss-Coray T, Goldring SR, Banda NK, Thurman JM, Gobezie R, Crow MK, Holers VM, Lee DM, Robinson WH (2011) Identification of a central role for complement in osteoarthritis. Nat Med 17(12):1674–1679. doi:10.1038/nm.2543
Aigner T, Fundel K, Saas J, Gebhard PM, Haag J, Weiss T, Zien A, Obermayr F, Zimmer R, Bartnik E, Bartnik E (2006) Large-scale gene expression profiling reveals major pathogenetic pathways of cartilage degeneration in osteoarthritis. Arthritis Rheum 54(11):3533–3544. doi:10.1002/art.22174
Ramasamy A, Mondry A, Holmes CC, Altman DG (2008) Key issues in conducting a meta-analysis of gene expression microarray datasets. PLoS Med 5(9):e184. doi:10.1371/journal.pmed.0050184
Xia J, Gill EE, Hancock RE (2015) NetworkAnalyst for statistical, visual and network-based meta-analysis of gene expression data. Nat Protoc 10(6):823–844. doi:10.1038/nprot.2015.052
Roberts PC (2008) Gene expression microarray data analysis demystified. Biotechnol Annu Rev 14:29–61. doi:10.1016/S1387-2656(08)00002-1
Breuer K, Foroushani AK, Laird MR, Chen C, Sribnaia A, Lo R, Winsor GL, Hancock RE, Brinkman FS, Lynn DJ (2013) InnateDB: systems biology of innate immunity and beyond–recent updates and continuing curation. Nucleic Acids Res 41(Database issue):D1228–D1233. doi:10.1093/nar/gks1147
Ungethuem U, Haeupl T, Witt H, Koczan D, Krenn V, Huber H, von Helversen TM, Drungowski M, Seyfert C, Zacher J, Pruss A, Neidel J, Lehrach H, Thiesen HJ, Ruiz P, Blass S (2010) Molecular signatures and new candidates to target the pathogenesis of rheumatoid arthritis. Physiol Genom 42A(4):267–282. doi:10.1152/physiolgenomics.00004.2010
Morales-Ducret J, Wayner E, Elices MJ, Alvaro-Gracia JM, Zvaifler NJ, Firestein GS (1992) Alpha 4/beta 1 integrin (VLA-4) ligands in arthritis. Vascular cell adhesion molecule-1 expression in synovium and on fibroblast-like synoviocytes. J Immunol 149(4):1424–1431
Pulsatelli L, Assirelli E, Dolzani P, Addimanda O, Mancarella L, Pavloska B, Facchini A, Meliconi R (2013) Increased serum vascular cell adhesion molecule (VCAM)-1 levels in patients with erosive hand osteoarthritis. Rheumatology 52(2):400–402. doi:10.1093/rheumatology/kes309
Schett G, Kiechl S, Bonora E, Zwerina J, Mayr A, Axmann R, Weger S, Oberhollenzer F, Lorenzini R, Willeit J (2009) Vascular cell adhesion molecule 1 as a predictor of severe osteoarthritis of the hip and knee joints. Arthritis Rheum 60(8):2381–2389. doi:10.1002/art.24757
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H (2011) Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 7(1):33–42. doi:10.1038/nrrheum.2010.196
Tsuchida AI, Beekhuizen M, ’t Hart MC, Radstake TR, Dhert WJ, Saris DB, van Osch GJ, Creemers LB (2014) Cytokine profiles in the joint depend on pathology, but are different between synovial fluid, cartilage tissue and cultured chondrocytes. Arthritis Res Ther 16(5):441. doi:10.1186/s13075-014-0441-0
Moller B, Kukoc-Zivojnov N, Kessler U, Rehart S, Kaltwasser JP, Hoelzer D, Kalina U, Ottmann OG (2001) Expression of interleukin-18 and its monokine-directed function in rheumatoid arthritis. Rheumatology 40(3):302–309
Bombardieri M, McInnes IB, Pitzalis C (2007) Interleukin-18 as a potential therapeutic target in chronic autoimmune/inflammatory conditions. Expert Opinion Biol Ther 7(1):31–40. doi:10.1517/14712598.7.1.31
Gracie JA, Forsey RJ, Chan WL, Gilmour A, Leung BP, Greer MR, Kennedy K, Carter R, Wei XQ, Xu D, Field M, Foulis A, Liew FY, McInnes IB (1999) A proinflammatory role for IL-18 in rheumatoid arthritis. J Clin Investig 104(10):1393–1401. doi:10.1172/JCI7317
Yamamura M, Kawashima M, Taniai M, Yamauchi H, Tanimoto T, Kurimoto M, Morita Y, Ohmoto Y, Makino H (2001) Interferon-gamma-inducing activity of interleukin-18 in the joint with rheumatoid arthritis. Arthritis Rheum 44(2):275–285. doi:10.1002/1529-0131(200102)44:2<275:AID-ANR44>3.0.CO;2-B
Park CC, Morel JC, Amin MA, Connors MA, Harlow LA, Koch AE (2001) Evidence of IL-18 as a novel angiogenic mediator. J Immunol 167(3):1644–1653
Olee T, Hashimoto S, Quach J, Lotz M (1999) IL-18 is produced by articular chondrocytes and induces proinflammatory and catabolic responses. J Immunol 162(2):1096–1100
Wang Y, Xu D, Long L, Deng X, Tao R, Huang G (2014) Correlation between plasma, synovial fluid and articular cartilage Interleukin-18 with radiographic severity in 33 patients with osteoarthritis of the knee. Clin Exp Med 14(3):297–304. doi:10.1007/s10238-013-0251-8
Szekanecz Z, Vegvari A, Szabo Z, Koch AE (2010) Chemokines and chemokine receptors in arthritis. Front Biosci 2:153–167
Mapp PI, Walsh DA (2012) Mechanisms and targets of angiogenesis and nerve growth in osteoarthritis. Nat Rev Rheumatol 8(7):390–398. doi:10.1038/nrrheum.2012.80
Villalvilla A, Gomez R, Roman-Blas JA, Largo R, Herrero-Beaumont G (2014) SDF-1 signaling: a promising target in rheumatic diseases. Expert Opinion Ther Targets 18(9):1077–1087. doi:10.1517/14728222.2014.930440
Blom AB, Brockbank SM, van Lent PL, van Beuningen HM, Geurts J, Takahashi N, van der Kraan PM, van de Loo FA, Schreurs BW, Clements K, Newham P, van den Berg WB (2009) Involvement of the Wnt signaling pathway in experimental and human osteoarthritis: prominent role of Wnt-induced signaling protein 1. Arthritis Rheum 60(2):501–512. doi:10.1002/art.24247
Baker N, Sharpe P, Culley K, Otero M, Bevan D, Newham P, Barker W, Clements KM, Langham CJ, Goldring MB, Gavrilovic J (2012) Dual regulation of metalloproteinase expression in chondrocytes by Wnt-1-inducible signaling pathway protein 3/CCN6. Arthritis Rheum 64(7):2289–2299. doi:10.1002/art.34411
Ramos YF, Bos SD, van der Breggen R, Kloppenburg M, Ye K, Lameijer EW, Nelissen RG, Slagboom PE, Meulenbelt I (2015) A gain of function mutation in TNFRSF11B encoding osteoprotegerin causes osteoarthritis with chondrocalcinosis. Ann Rheum Dis 74(9):1756–1762. doi:10.1136/annrheumdis-2013-205149
Litherland GJ, Dixon C, Lakey RL, Robson T, Jones D, Young DA, Cawston TE, Rowan AD (2008) Synergistic collagenase expression and cartilage collagenolysis are phosphatidylinositol 3-kinase/Akt signaling-dependent. J Biol Chem 283(21):14221–14229. doi:10.1074/jbc.M710136200
Funding
This study was funded by Basic Science Research Pro-gram through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2014R1A1A2001950).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Robin Park and Jong Dae Ji declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, R., Ji, J.D. Unique gene expression profile in osteoarthritis synovium compared with cartilage: analysis of publicly accessible microarray datasets. Rheumatol Int 36, 819–827 (2016). https://doi.org/10.1007/s00296-016-3451-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-016-3451-1