Abstract
Behçet’s disease (BD) is a chronic disorder characterized by mucocutaneous and multisystem manifestations. Fibromyalgia (FM) is characterized by widespread musculoskeletal pain and may be present concomitantly with several rheumatic diseases. Our aims were to investigate the prevalence of FM in patients with BD and to evaluate the possible relation of FM presence with BD disease activity. A total of 104 Behcet patients were included in this study. Age, sex, disease durations and the BD Current Activity Form (BDCAF) scores as disease activity evaluation were recorded. Presence of FM and the Fibromyalgia Impact Questionnaire (FIQ) scores was investigated. Also, ESR and CRP concentrations were determined in all patients. Mann–Whitney U test and Pearson’s correlation tests were used for the statistical analysis. There were 60 female and 40 male patients with an age range of 19–51 years. Eighteen of 100 BD patients were diagnosed as FM. Although ages, disease duration and laboratory parameters did not differ between BD patients with and without FM, BD patients with FM were more frequently female (p < 0.000). The presence of FM did not differ significantly between patients with and without systemic manifestations. Also, oral–genital ulcers, erythema nodosum, thrombophlebitis, pustular lesions and doctor’s impression of disease activity scores were not found to be different in BD patients with or without FM. However, there were significant differences in fatigue, headache, arthralgia and patient impression of disease activity (today and last 28 days) between these groups (p < 0.000; p < 0.01; p < 0.01; p = 0.021 and p = 0.027, respectively). Also, there were significant correlations between BDCAF and FIQ items that refer pain and fatigue (p < 0.01). FM is a common and important clinical problem that may represent an additional factor that worsens pain and physical limitations in patients with BD. The higher prevalence of FM in patients with BD seems to be affected by BD itself, rather than its severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behçet’s disease (BD) is a chronic multisystem disorder characterized by oral and genital ulcers, cutaneous lesions, and ophthalmologic, neurologic, and gastrointestinal manifestations [1]. Besides several clinical manifestations in BD, 10 % of patients may also suffer from vague musculoskeletal pain [2]. Fibromyalgia (FM) is characterized by widespread musculoskeletal pain and the presence of certain tender points. It can affect about up to 7 % of the general population [3, 4], and concomitant FM has been reported in 14–35 % of the cases with several rheumatic diseases [3–7]. Although the relationship between fibromyalgia (FM) and rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) has been well studied, relationship between FM and BD is limited. Also, there are no published data on the influence of the disease activity when they are present concomitantly.
In this preliminary observation study, our primary aims were to investigate the prevalence of FM in patients with BD and to evaluate the possible relation of FM presence with BD disease activity.
Patients and methods
Patients
One hundred and four consecutive patients with BD who fulfilled the diagnosis criteria of the International Study Group for BD were included in this study after obtaining the informed consent from all participants [8]. Patients with thyroid function disorders, infections, psychosomatic or psychiatric disorders and any other chronic diseases were excluded from the study. Also, dependence on alcohol or other substances and any psychotropic drug usage were considered as exclusion criteria.
Clinical and laboratory assessments
For all of the patients with BD, demographic properties including age and sex and disease durations were recorded. The BD Current Activity Form (BDCAF), which scores the history of clinical features that have been present during the 4 weeks prior to the day of assessment, was used for the evaluation of disease activity [9]. With this activity form, fatigue, headache, oral–genital ulceration, skin lesions, joint involvement, gastrointestinal system involvement, central nervous system involvement, major vessel involvement, patient’s impression of disease activity (last 28 days and the same day) and doctor’s impression of disease activity were evaluated in our study. A Turkish version of BDCAF has been tested and validated for our population [10].
In all patients with BD, presence of FM was investigated as recommended by the American College of Rheumatology (ACR) classification criteria that include a history of widespread pain lasting more than 3 months and the presence of at least 11 of the 18 specified tender points described for FM [11]. Tender point examination was evaluated by the same clinician, and it involved applying a uniform manual finger pressure (ca. 4 kg), until the fingernail bed blanched, at each of the 9 paired referenced anatomical locations, and definite tenderness at any point was considered to be present. Also for the evaluation of patients with FM, we used the validated Turkish version of “The Fibromyalgia Impact Questionnaire (FIQ)” scoring system that evaluates the impact of FM on multidimensional aspects. FIQ was first published in 1991, translated into many languages including Turkish, and it has been one of the most used questionnaires in clinical practice and researches for the evaluation of the functional limitations and disability of FM [4, 12, 13].
As laboratory assessments, erythrocyte sedimentation rate (ESR) according to Westergren method and C-reactive protein (CRP) concentration by nephelometry (Beckman Array Protein System, USA) was determined in all patients.
Statistics
The results were analyzed by the SPSS package program version 18.0 (SPSS Inc., Chicago,IL, USA). Mann–Whitney U test was used to compare the data between groups of BD patients with and without FM, and Pearson’s correlation analysis was performed to determine the possible correlations between BD activity and FIQ scores. A p value of <0.05 was considered statistically significant.
Results
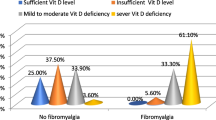
After exclusion of four patients due to thyroid dysfunction and antidepressant usage, one hundred patients with BD were evaluated in this study. There were 60 female and 40 male patients with an age range of 19–51 (35.1 ± 7.9 year ± SD) years. The disease duration of the patients was 84.9 ± 48.5 months. Eighteen of 100 BD patients (18 %) were diagnosed as FM according to ACR criteria. Age, gender ratio, disease durations and ESR and CRP levels of BD patients with or without FM were shown in Table 1. Although ages, disease duration and laboratory parameters of groups did not differ between BD patients with and without FM, BD patients with FM were more frequently female (p < 0.000).
The presence of FM did not differ significantly between BD patients with and without severe manifestations such as uveitis, central nervous system, gastrointestinal system or major vessel involvement (since there were only two patients with major vessel involvement, they were not included in the analysis). Also, oral–genital ulcers, erythema nodosum, superficial thrombophlebitis, pustular lesions and doctor’s impression of disease activity scores were not found to be different in BD patients with or without FM. However, there were significant differences in fatigue, headache, arthralgia and patient impression of disease activity (today and last 28 days) between these groups (p < 0.000; p < 0.01; p < 0.01; p = 0.021 and p = 0.027, respectively) (Table 2).
Also, we investigated the possible correlations between BD activity and FIQ scores. Although we determined no correlation between other parameters of BDCAF and FIQ scores, there were significant correlations between BDCAF and FIQ items that refer pain (headache, arthralgia) and fatigue (p < 0.01).
Discussion
FM is estimated to affect 2–7 % of the general population [3, 4]. FM is also a well-documented secondary feature of many rheumatic diseases, including RA and SLE [5, 14, 15]. Also, its frequency was reported in up to 24 % of patients with psoriatic arthritis, in 49 % of patients with Crohn’s disease and 50 % of women with AS [16–18]. However, the investigations about the relationship between FM and BD are limited. FM is a potentially debilitating disorder that can have a devastating effect on quality of life, impairing the patient’s abilities and can result with economic and social burdens [19]. Since BD can also cause vague musculoskeletal pain, to differentiate the concomitant FM is particularly important. Previous studies reported considerably different FM prevalence in the patients with BD with a range of 8.9 and 37.1 % [20–22]. In our study, 18 % of the cases with BD were found to have concomitant FM. Our FM prevalence was found to be higher than the previous Turkish investigation. This might be due to the female predominance of our study cohort. As in several previous studies, FM was found to be more frequent in female cases with BD in our study. Female predominance is a well-known feature of FM with several explanations such as hormone-related mechanisms or gender-related response to the tender point requirement in the diagnosis [19, 23].
Since it may be thought that BD duration might contribute the presence of FM in patients with BD, disease duration was also investigated as a possible factor related to FM and BD. Similar to previous studies we found no difference in disease duration between BD patients with or without FM [21, 22]. Also, laboratory investigations as acute phase response showed no difference between BD patients with or without FM, as it can be expected.
Since FM may be affected by the involvements of BD, our study investigated the relation between clinical manifestations and FM presence. It was found that the presence of FM did not differ significantly between BD patients with or without objective manifestations. This result is consistent with previous studies that investigated FM and BD relation [21, 22]. Disease activity of BD was also questioned as a possible factor related to FM in these studies, and they revealed no association between BD activity and FM presence. However, in previous studies, disease activity was evaluated clinically by summing the manifestations. In our study, we used a standardized scale, BDCAF, which was developed and validated due to the absence of reliable clinical and laboratory indices that are useful in reflecting overall disease activity for BD. The heterogeneous nature of the disease expression of BD makes it difficult to achieve a single score for disease activity. Because BDCAF does not have an overall activity score, that is, a composite index, deduced from the individual scores for different systems, we evaluated the possible relations with FM for each parameter of the scale. In our study, we found no difference in objective disease activity parameters in BDCAF in BD patients with or without FM. Despite the methodological differences in the evaluation of disease activity in BD, this result is consistent with previous studies [21, 22]. These results suggest that higher prevalence of FM in BD is affected by BD itself, rather than its severity. On the other hand, in our study, in spite of the similar results in objective BD manifestations in patients with or without FM, there were significantly higher scores in fatigue, headache and arthralgia and patient impression of disease activity parameters of the BDCAF scale in BD patients with FM than the others. Although it was not statistically significant, doctor’s impression of disease activity parameter also showed a mild higher score in BD patients with FM. Supporting these data, in our previous study investigating relation between disease activity and depression in patients with BD, patient’s impression of disease activity and joint involvement in patients with BD were found as related factors to the depression scores [24].
In our study, we also investigated the possible correlations of BD disease activity and impact of FM on the patient with a scoring system (FIQ). Although we determined no correlation between other parameters of BDCAF and FIQ scores, there was a significant correlation between BDCAF and FIQ items that refer pain (headache and arthralgia) and fatigue. These results can suggest that since it requires different approaches in the managements of the diseases, to differentiate the clear source of these subjective complaints as BD or FM is particularly important.
Being the first study, investigating the interactions between disease activities of BD and FM may increase the importance of our study. The main weakness of our study was the inabilities of researching the relation between FM and relatively rare and severe involvements of BD due to the limited number of patients.
In conclusion, FM is a common and important clinical problem that may represent an additional factor that worsens pain and physical limitations in patients with BD. The higher prevalence of FM in patients with BD seems to be affected by BD itself, rather than its severity. Subjective complains overlapping in FM and BD need to be differentiated clearly regarding management differences in these diseases. An increased awareness of the possible FM coexistence with BD may contribute more accurate management of BD.
References
Sakene T, Takeno M, Suzuki N, Inaba G (1999) Behçet’s disease. N Engl J Med 341:1284–1291
Yurdakul S, Yazici H, Tüzün Y, Pazarli H, Yalçin B, Altaç M, Ozyazgan Y, Tüzüner N, Müftüoğlu A (1983) The arthritis of Behçet’s disease: a prospective study. Ann Rheum Dis 42:505–515
Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L (1995) The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 38:19–28
Ediz L, Hiz O, Toprak M, Tekeoglu I, Ercan S (2011) The validity and reliability of the Turkish version of the Revised Fibromyalgia Impact Questionnaire. Clin Rheumatol 30:339–346
Wolfe F, Michaud K (2004) Severe rheumatoid arthritis (RA), worse outcomes, comorbid illness, and sociodemographic disadvantage characterize ra patients with fibromyalgia. J Rheumatol 31:695–700
Naranjo A, Ojeda S, Francisco F, Erausquin C, Rúa-Figueroa I, Rodríguez-Lozano C (2002) Fibromyalgia in patients with rheumatoid arthritis is associated with higher scores of disability. Ann Rheum Dis 61:660–661
Torrente-Segarra V, Carbonell-Abelló J, Castro-Oreiro S, Manresa Domínguez JM (2010) Association between fibromyalgia and psychiatric disorders in systemic lupus erythematosus. Clin Exp Rheumatol 28:S22–S26
International Study Group for Behcet’s Disease (1990) Criteria for the diagnosis of Behcet’s Disease. Lancet 335:1078–1080
Bhakta BB, Brennan P, James TE, Chamberlain MA et al (1999) Behçet’s disease: evaluation of a new instrument to measure clinical activity. Rheumatology 38:728–733
Hamuryudan V, Fresko İ, Direskeneli H, Tennant MJ et al (1999) Evaluation of the Turkish translation of a disease activity form for Behçet’s syndrome. Rheumatology 38:734–736
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL et al (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the Multicenter Criteria Committee. Arthritis Rheum 33:160–172
Sarmer S, Ergin S, Yavuzer G (2000) The validity and reliability of the Turkish version of the Fibromyalgia Impact Questionnaire. Rheumatol Int 20:9–12
Burckhardt CS, Clark SR, Bennett RM (1991) The fibromyalgia impact questionnaire: development and validation. J Rheumatol 18:728–733
Middleton GD, McFarlin JE, Lipsky PE (1994) The prevalence and clinical impact of Fibromyalgia in systemic lupus erythematosus. Arthritis Rheum 37:1181–1188
Buskila D, Press J, Abu-Shakra M (2003) Fibromyalgia in systemic lupus erythematosus: prevalence and clinical implications. Clin Rev Allergy Immunol 25:25–28
Buskila D, Langevitz P, Gladman DD, Urowitz S, Smythe HA (1992) Patients with rheumatoid arthritis are tenderer than those with psoriatic arthritis. J Rheumatol 19:1115–1119
Buskila D, Odes LR, Neumann L, Odes HS (1999) Fibromyalgia in Inflammatory bowel disease. J Rheumatol 26:1167–1171
Aloush V, Ablin JN, Reitblat T, Caspi D, Elkayam O (2007) Fibromyalgia in women with ankylosing spondylitis. Rheumatol Int 27:865–868
Arnold LM, Clauw DJ, McCarberg BH (2011) Improving the recognition and diagnosis of fibromyalgia. Mayo Clin Proc 86:457–464
Al-Izzi MK, Jabber AS (2004) Fibromyalgia in Iraqi patients with Behcet’s disease. J Med Liban 52:86–90
Lee SS, Yoon HJ, Chang HK, Park KS (2005) Fibromyalgia in Behçet’s disease is associated with anxiety and depression, and not with disease activity. Clin Exp Rheumatol 23:15–19
Yavuz S, Fresko I, Hamuryudan V, Yurdakul S, Yazici H (1998) Fibromyalgia in Behçet’s syndrome. J Rheumatol 25:2219–2220
Akkuş S, Senol A, Ayvacioglu NB, Tunc E, Eren I, Isler M (2004) Is female predominance in irritable bowel syndrome related to fibromyalgia? Rheumatol Int 24:106–109
Melikoglu MA, Melikoglu M (2010) The relationship between disease activity and depression in patients with Behcet disease and rheumatoid arthritis. Rheumatol Int 30:941–946
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Melikoglu, M., Melikoglu, M.A. The prevalence of fibromyalgia in patients with Behçet’s disease and its relation with disease activity. Rheumatol Int 33, 1219–1222 (2013). https://doi.org/10.1007/s00296-012-2530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2530-1