Abstract
The relationship between synovial fluid (SF) cAMP level and IL-18 and PGE2 SF levels in rheumatoid arthritis (RA) and osteoarthritis (OA) patients, and between SF cAMP level and disease as well as inflammatory activity in RA were investigated in 17 RA and 19 OA patients. Erythrocyte sedimentation rate (ESR), serum (S) C-reactive protein (CRP) level and SF IL-18 level were higher in RA than in OA patients. SF PGE2 level was similar in both groups. SF cAMP level was higher in OA than in RA patients. In RA patients, SF cAMP level showed negative correlation with Disease Activity Score including a 28-joint count and S CRP, ESR and SF IL-18 level. The results suggest that cAMP promotes anti-inflammatory response in RA and OA patients, which is higher in the latter. Promotion of anti-inflammatory response by cAMP elevating agents might be useful in the treatment of RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A complex cytokine network produced by cells from inflamed synovia is involved in the pathogenesis of rheumatoid arthritis (RA). The network is composed of positive and negative feedback pathways regulating cytokine expression and action [1, 2].
Interleukin (IL)-18 is a proinflammatory cytokine with a prominent role in the pathogenesis of RA synovitis and tissue destruction in RA [3]. A number of proinflammatory cytokines [4, 5] including IL-18 [6, 7] can be detected in higher levels in synovial fluid (SF) of RA patients as compared with osteoarthritis (OA) patients.
Prostaglandin E2 (PGE2) contributes to a number of reactions involved in RA synovitis [8]. However, it has not been extensively studied in SF of RA patients. A higher level of SF PGE2 was found in RA than in OA patients, with no correlation with the levels of various cytokines [9]. The improvement of synovitis in RA patients by various drug treatments was accompanied by a decrease in the SF level of PGE2 [10–12].
Cyclic adenosine 5′-monophosphate (cAMP) mediates a number of various anti-inflammatory pathways resulting in inhibition of tumor necrosis factor alpha (TNFα) and IL-1, and stimulation of IL-10 production [13]. In vitro and in vivo studies demonstrated an inhibitory effect of cAMP on numerous and various reactions involved in immune and inflammatory responses, suggesting a central role of cAMP in anti-inflammatory mechanisms [14].
There are only a few studies exploring cAMP in SF of RA patients. There was no correlation between SF cAMP level and disease activity [15, 16], however, the treatment increasing the SF cAMP level ameliorated the symptoms of joint inflammation [16].
Considering the complex relationship of various participants involved in the pathogenesis of RA synovitis, we studied the relationship of SF cAMP primarily with two proinflammatory mediators, IL-18 and PGE2 in SF, and with the disease and systemic inflammatory activity in RA and OA patients.
Methods
The study included 17 RA and 19 OA consecutive patients with knee joint effusion and indication for arthrocentesis. RA patients (male/female 3/14, median age 53, range 39–66) met the American College of Rheumatology 1987 classification criteria [17]. All patients were treated continuously with some of the disease modifying anti-rheumatic drugs alone or in combination with other anti-rheumatic drugs: nonsteroidal anti-inflammatory drugs (NSAIDs) (n = 5), cyclo-oxygenase (COX)-2 inhibitors (n = 10) and methylprednisolone (n = 4).
In OA patients (male/female 10/9, median age 54, range 21–69), knee OA was diagnosed based on radiography and clinical findings. They were treated at the time of arthrocentesis with NSAIDs (n = 13) or COX-2 inhibitors (n = 4). The written informed consent was obtained from the patients involved in the study. The study was approved by Ethical Committee of the Dubrava University Hospital, Zagreb.
Disease activity in RA patients was evaluated by Disease Activity Score including a 28-joint count and S CRP level (DAS28-CRP) [18] using DAS28-CRP Calculator [19].
In both RA and OA patients SF was obtained by a therapeutic knee arthrocentesis in volume between 30 and 80 mL, depending on the volume of knee effusion. To reduce the viscosity of SF prior to analysis, SF samples were treated with hyluronidase (20 units/mL, at 37°C for 30 min) using Hylorunidase Sigma, type 1–2, H-3506 [20].
Erythrocyte sedimentation rate (ESR) was measured by a standard technique [21] and serum (S) C-reactive protein (CRP) was measured by an immunoturbidimetric assay [22] using Olympus autoanalyzer. SF IL-18, PGE2 and cAMP levels were measured by enzyme-linked immunosorbent assay (ELISA) using IL-18 kit from R&D (Cat. No. 7620), PGE2 Correlate-EIA (Cat. No. 900–001) and cAMP Correlate-EIA (Cat. No. 900-067) from Assay Designs, respectively. The manufacturer’s instructions were strictly followed [23–25] and plates were read on a Dynatech M5000 reader. Statistics was done using NCSS 2000 program attached to the book [26]. As higher values for proinflammatory variables and lower values for anti-inflammatory variables in RA then in OA group could be expected, the differences between mean in RA versus OA group were analyzed by one-tailed t test. The correlations between various parameters within groups were analyzed by Pearson correlation. P values less then 0.05 were considered significant.
Results
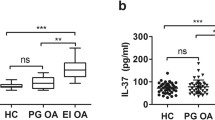
ESR, S CRP level and SF IL-18 level were higher in RA than in OA patients. SF PGE2 SF level was similar in both groups. SF cAMP level was higher in OA than in RA patients (Table 1).
In RA patients, SF cAMP level showed negative correlation with DAS28-CRP, ESR and SF IL-18 level (Fig. 1a–c). The correlation coefficients are shown on Table 2. There were no statistically significant correlation coefficients between SF cAMP level and S CRP level in RA patients and between SF cAMP and S CRP, ERS, SF IL-18 and SF PgE2 in OA patients.
Relationship between synovial fluid cyclic adenosine 5′-monophosphate (cAMP) level and (a) Disease Activity Score including a 28-joint count and serum C-reactive protein level (DAS28-CRP). b Erythrocyte sedimentation rate (ESR), and (c) synovial fluid interleukin-18 (IL-18) level in rheumatoid arthritis patients (n = 17). For correlation coefficients, see Table 2
Discussion
Differences between the RA and OA groups of patients (higher ESR, S CRP level, SF IL-18 level and lower SF cAMP level in RA than in OA patients) reflected a higher inflammatory activity in RA than in OA. These results are in concordance with the higher SF levels of various proinflammatory cytokines found in RA as compared with OA patients [3–6].
Similar SF PGE2 levels in RA and OA patients could be explained by medication with drugs lowering PGE2 synthesis, administered to patients of both groups, and by the anti-inflammatory effects of PGE2. Generally, PGE2 is considered as a proinflammatory mediator [8] but in fact, it exerts dual pro- and anti-inflammatory effects depending on target cells, receptor subtype and context of activation [27–30]. PGE2 contributes to switching on the resolution of inflammation [31], so PGE2 need not correlate with chronic inflammatory response.
In contrast to previous studies [15, 16], we found negative correlation between SF cAMP level and disease activity as assessed by DAS28-CRP and ESR.
The lack of correlation between SF cAMP and S CRP levels could be explained by dual opposite effects of cAMP in the regulation of IL-6 expression, which is a major stimulator of CRP synthesis [32]. The expression of IL-6 is enhanced by TNFα, IL-1β and PGE2. The latter acts through cAMP signaling [33, 34]. On the other hand, an increase in cAMP suppresses the expression of TNFα [35–37] and could be assumed that the net effect of cAMP on IL-6 synthesis and consequently CRP synthesis depends on balance of these two processes.
Relationship between cAMP and PGE2 and IL-18 SF levels was not investigated. The majority of PGE2 effects are mediated by cAMP signaling [27] and positive correlation between cAMP and PGE2 may be expected. The lack of correlation between cAMP and PGE2 SF levels might be due to the PGE2 lowering medication administered to all patients, variability in PGE2 signaling depending on target cells, receptor subtype and co-stimulation [27], and effects of a number of G-protein coupled receptor ligands other than PGE2 that also act through cAMP signaling and contribute to the RA pathogenesis [38].
IL-18 is a proinflammatory cytokine with a powerful Th1 promoting activity [39]. The negative correlation between cAMP and IL-18 SDF levels might be explained by the immunomodulatory function of cAMP. Suppressing T-cell activation, cAMP prevents inappropriate immune response and autoimmunity [40]. Elevation of cAMP differently affects cytokine production in effector T cells, suppressing it in Th1 cells and increasing it in Th2 cells [41]. cAMP elevating agents including PGE2 drive Th1/Th2 balance toward Th2 response [38, 42]. PGE2 participates in negative feedback loops regulating cytokine expression. TNFα and IL-1β increase COX-2 expression and PGE2 synthesis [8]. PGE2, in turn, down-regulates TNFα and IL-1β expression [42, 43]. In contrast to IL-1β, IL-18 does not increase COX-2 expression and PGE2 synthesis [44]. Consequently, a negative correlation between cAMP and IL-18 might be expected.
In conclusion, assuming that essential molecular mechanisms regulating immune and inflammatory responses are common to all relevant cell types, the data derived from experimental settings (cell culture, experimental animals) can be translated to clinical setting (our study). Taking together, cAMP appears as a pivot mediator of anti-inflammatory response. Elevation of SF cAMP level accompanied by lower DAS28-CRP score, lower ESR and lower SF IL-18 level in RA, and a higher SF cAMP level in OA than in RA suggest that cAMP promotes anti-inflammatory response in both RA and OA patients, which is higher in the latter. Promotion of anti-inflammatory response by agents elevating cAMP might be useful in the treatment of RA.
References
Weyand CM, Goronzy JJ (2006) Pathomechanisms in rheumatoid arthritis—time for a string theory? J Clin Invest 116:869–871. doi:10.1172/JCI28300
Choy EH, Panayi GS (2001) Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med 344:907–916. doi:10.1056/NEJM200103223441207
Dayer JM (1999) Interleukin-18, rheumatoid arthritis, and tissue destruction. J Clin Invest 104:1337–1339. doi:10.1172/JCI8731
Steiner G, Tohidast-Akrad M, Witzmann G et al (1999) Cytokine production by synovial T cells in rheumatoid arthritis. Rheumatology (Oxford) 38:202–213. doi:10.1093/rheumatology/38.3.202
Manicourt DH, Poilvache P, Van Egeren A et al (2000) Synovial fluid levels of tumor necrosis factor alpha and oncostatin M correlate with levels of markers of the degradation of crosslinked collagen and cartilage aggrecan in rheumatoid arthritis but not in osteoarthritis. Arthritis Rheum 43:281–288. doi 10.1002/1529-0131(200002)43:2<281::AID-ANR7>3.0.CO;2-7
Yamamura M, Kawashima M, Taniai M et al (2001) Interferon-gamma-inducing activity of interleukin-18 in the joint with rheumatoid arthritis. Arthritis Rheum 44:275–285. doi 0.1002/1529-0131(200102)44:2<275::AID-ANR44>3.0.CO;2-B
Petrovic-Rackov L, Pejnovic N (2006) Clinical significance of IL-18, IL-15, IL-12 and TNF-alpha measurement in rheumatoid arthritis. Clin Rheumatol 25:448–452. doi:10.1007/s10067-005-0106-0
Martel-Pelletier J, Pelletier JP, Fahmi H (2003) Cyclooxygenase-2 and prostaglandins in articular tissues. Semin Arthritis Rheum 33:155–167. doi:10.1016/S0049-0172(03)00134-3
Hishinuma T, Nakamura H, Sawai T et al (1999) Microdetermination of prostaglandin E2 in joint fluid in rheumatoid arthritis patients using gas chromatography/selected ion monitoring. Prostaglandins Other Lipid Mediat 58:179–186. doi:10.1016/S0090-6980(99)00028-3
Goto M, Hanyu T, Yoshio T et al (2001) Intra-articular injection of hyaluronate (SI-6601D) improves joint pain and synovial fluid prostaglandin E2 levels in rheumatoid arthritis: a multicenter clinical trial. Clin Exp Rheumatol 19:377–383
Bertin P, Lapicque F, Payan E et al (1994) Sodium naproxen: concentration and effect on inflammatory response mediators in human rheumatoid synovial fluid. Eur J Clin Pharmacol 46:3–7. doi:10.1007/BF00195907
Seppälä E, Nissilä M, Isomäki H et al (1985) Comparison of the effects of different anti-inflammatory drugs on synovial fluid prostanoid concentrations in patients with rheumatoid arthritis. Clin Rheumatol 4:315–320. doi:10.1007/BF02031615
Elenkov IJ, Wilder RL, Chrousos GP et al (2000) The sympathetic nerve—an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev 52:595–638
Moore AR, Willoughby DA (1995) The role of cAMP regulation in controlling inflammation. Clin Exp Immunol 101:387–389
Wadskov S, Donde R, Sylvest J (1979) Plasma and synovial fluid cAMP in patients with rheumatoid arthritis. Scand J Rheumatol 8:136–138. doi:10.3109/03009747909114444
Trang LE, Lövgren O, Roch-Norlund AE et al (1979) Cyclic nucleotides in joint fluid in rheumatoid arthritis and in Reiter’s syndrome. Scand J Rheumatol 8:91–96. doi:10.3109/03009747909105343
Arnett FC, Edworthy SM, Bloch DA et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324. doi:10.1002/art.1780310302
http://www.das-score.nl/www.das-score.nl/index.html. Accessed 8 Sept 2007
http://www.das-score.nl/www.das-score.nl/dasculators.html. Accessed 8 Sept 2007
Ziolkowska M, Kurowska M, Radzikowska A et al (2002) High levels of osteoprotegerin and soluble receptor activator of nuclear factor kappa B ligand in serum of rheumatoid arthritis patients and their normalization after anti-tumor necrosis factor alpha treatment. Arthritis Rheum 46:1744–1753. doi:10.1002/art.10388
Fischbach F (1988) Laboratory diagnostic tests, 3rd edn. Lippincott, Philadelphia, pp 57–59
http://www.olympus-diagnostica.com/diagnostica/3112_marketinginformation.cfm. Accessed 8 Sept 2007
http://www.rndsystems.com/pdf/7620.pdf. Accessed 8 Sept 2007
http://www.assaydesigns.com/objects/catalog//product/extras/900-001.pdf. Accessed 8 Sept 2007
http://www.assaydesigns.com/objects/catalog//product/extras/900-067.pdf. Accessed 8 Sept 2007
Dawson B, Trapp RG (2001) Basic and clinical biostatistics, 3rd edn. Lange, New York
Hata AN, Breyer RM (2004) Pharmacology and signaling of prostaglandin receptors: multiple roles in inflammation and immune modulation. Pharmacol Ther 103:147–166. doi:10.1016/j.pharmthera.2004.06.003
Akaogi J, Nozaki T, Satoh M et al (2006) Role of PGE2 and EP receptors in the pathogenesis of rheumatoid arthritis and as a novel therapeutic strategy. Endocr Metab Immune Disord Drug Targets 6:383–394
Min SY, Kim WU, Cho ML et al (2002) Prostaglandin E2 suppresses nuclear factor-kappaB mediated interleukin 15 production in rheumatoid synoviocytes. J Rheumatol 29:1366–1376
Gomez PF, Pillinger MH, Attur M et al (2005) Resolution of inflammation: prostaglandin E2 dissociates nuclear trafficking ofindividual NF-kappaB subunits (p65, p50) in stimulated rheumatoid synovial fibroblasts. J Immunol 175:6924–6930
Yacoubian S, Serhan CN (2007) New endogenous anti-inflammatory and proresolving lipid mediators: implications for rheumatic diseases. Nat Clin Pract Rheumatol 3:570–579. doi:10.1038/ncprheum0616
Gabay C (2006) Interleukin-6 and chronic inflammation. Arthritis Res Ther 8 (Suppl 2):S3. doi:10.1186/ar1917
Baumann H, Kushner I (1998) Production of interleukin-6 by synovial fibroblasts in rheumatoid arthritis. Am J Pathol 152:641–644
Dendorfer U, Oettgen P, Libermann TA (1994) Multiple regulatory elements in the interleukin-6 gene mediate induction by prostaglandins, cyclic AMP, and lipopolysaccharide. Mol Cell Biol 14:4443–4454
Eigler A, Siegmund B, Emmerich U et al (1998) Anti-inflammatory activities of cAMP-elevating agents: enhancement of IL-10 synthesis and concurrent suppression of TNF production. J Leukoc Biol 63:101–107
Kasyapa CS, Stentz CL, Davey MP et al (1999) Regulation of IL-15-stimulated TNF-alpha production by rolipram. J Immunol 163:2836–2843
Souness JE, Griffin M, Maslen C et al (1996) Evidence that cyclic AMP phosphodiesterase inhibitors suppress TNF alpha generation from human monocytes by interacting with a ‘low-affinity’ phosphodiesterase 4 conformer. Br J Pharmacol 118:649–658
Schillace RV, Carr DW (2006) The role of protein kinase A and A-kinase anchoring proteins in modulating T-cell activation: progress and future directions. Crit Rev Immunol 26:113–131
Gracie JA, Forsey RJ, Chan WL et al (1999) A proinflammatory role for IL-18 in rheumatoid arthritis. J Clin Invest 104:1393–1401. doi:10.1172/JCI7317
Taskén K, Aandahl EM (2004) Localized effects of cAMP mediated by distinct routes of protein kinase A. Physiol Rev 84:137–167. doi:10.1152/physrev.00021.2003
Harris SG, Padilla J, Koumas L et al (2002) Prostaglandins as modulators of immunity. Trends Immunol 23:144–150. doi:10.1016/S1471-4906(01)02154-8
Chen CH, Zhang DH, LaPorte JM et al (2000) Cyclic AMP activates p38 mitogen-activated protein kinase in Th2 cells: phosphorylation of GATA-3 and stimulation of Th2 cytokine gene expression. J Immunol 165:5597–5605
Harizi H, Gualde N (2006) Pivotal role of PGE2 and IL-10 in the cross-regulation of dendritic cell-derived inflammatory mediators. Cell Mol Immunol 3:271–277
Lee JK, Kim SH et al (2004) Differences in signaling pathways by IL-1beta and IL-18. Proc Natl Acad Sci USA 101:8815–8820. doi:10.1073/pnas.0402800101
Acknowledgments
The authors thank Mirko Škoro, MD, PhD, for participation in patient examination. The study was supported by a grant to JMV from the Croatian Ministry of Science, Education and Sports (No. 198-1081874-0183).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morovic-Vergles, J., Culo, M.I., Gamulin, S. et al. Cyclic adenosine 5′-monophosphate in synovial fluid of rheumatoid arthritis and osteoarthritis patients. Rheumatol Int 29, 167–171 (2008). https://doi.org/10.1007/s00296-008-0663-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0663-z