Abstract
Ultrasonography (US) and power Doppler sonography (PDS) was used to investigate causes of new onset of shoulder pain and sites of shoulder inflammation in 157 shoulders of 99 patients with rheumatoid arthritis (RA). US detected effusion and/or synovitis in 92/157 glenohumeral joints, subdeltoid bursitis in 56/157 shoulders and tenosynovitis of biceps tendon in 55/157 shoulders. Bursitis and/or tenosynovitis were accompanied by glenohumeral synovitis in 68/90 shoulders. 68% of serologically active and 12% of serologically inactive patients had glenohumeral synovitis. PDS showed increased microvascular blood flow in 33 of the 44 investigated shoulders. Glenohumeral synovitis was correlated to elevated C-reactive protein levels (p = 0.0001) and microvascular blood flow assessed by PDS (p = 0.02). This study shows that rheumatoid shoulder pain is not caused by glenohumeral synovitis in 32% of patients, despite serologically active RA. US and PDS are mandatory to elucidate the origin of inflammatory and noninflammatory shoulder pain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The shoulder is involved in 70% of patients with rheumatoid arthritis (RA). In contrast to younger patients with RA, in late onset of rheumatoid arthritis shoulder pain is frequently the first symptom of the disease.
Shoulder pain and swelling are included in the disease activity scores such as DAS 28. However, the painful shoulder in rheumatoid arthritis patients may be caused not only by inflammation but also by noninflammatory diseases, such as degenerative disorders. Inflammatory changes in the rheumatoid shoulder includes synovitis of the glenohumeral joints, frequently associated with tenosynovitis of the bicipital tendon sheath and subdeltoid bursitis.
Clinical assessment shows low accuracy in the diagnosis of periarticular shoulder lesions compared with ultrasonography (US) [1]. In shoulder imaging, plain radiography has the disadvantage of being insensitive in arthritis of the glenohumeral joint. Magnetic resonance imaging (MRI) and musculoskeletal US are more sensitive methods than radiography in demonstrating erosions, pathologies of synovia, bursae, tendon sheaths and rotator cuff. The use of MRI is limited by its high costs. Musculoskeletal US has become an established adjunctive technique for the diagnosis of rheumatic diseases by its ability to detect minor synovitic lesions, tenosynovitis, bursitis and bone lesions. In RA and elderly-onset RA several studies have focused on the usefulness of US in the assessment of painful rheumatoid shoulders [2–4]. Glenohumeral synovitis, a peritendineous hypoechoic rim in bicipital tendon sheath and hypoechoic mass in the subdeltoid bursa are frequent US findings in patients with RA. A small study showed that isolated bicipital tenosynovitis and subdeltoid bursitis may occur in RA patients [2]. However, fluid in the biceps tendon sheath may caused by deteriorated bicipital gliding mechanism due to degenerative disorders or by exudative and proliferative synovitis. Strunk et al. recently showed that power Doppler sonography (PDS) helps to differentiate between degenerative shoulder disorders and rheumatoid shoulder as it demonstrates vascularity in the long bicipital tendon sheath only in patients with RA [5].
The aim of the study was to investigate the cause of new onset of shoulder pain in patients with RA in correlation to the systemic inflammatory activity assessed by CRP levels. We further analysed the value of PDS to estimate the inflammatory activity within different shoulder structures.
Methods
Patients
Ninety-nine consecutive patients with RA and shoulder pain were examined by musculoskeletal US. The group consisted of 67 women and 32 men (mean age 63 ± 13;range 23–85) with a disease duration of mean 8 ± 9 years (6 weeks–38 years). Nine patients had late onset of RA (age >60 years). Inclusion criteria were a history of new onset of shoulder pain and a painful shoulder on palpation or examination. In patients with bilateral shoulder pain both sites were included in the analysis. Overall, 157 glenohumeral joints were included in this study.
Out of 99 patients 80 (81%) had been treated with glucocorticoids and/or disease-modifying antirheumatic drugs. Nineteen patients (19%) had a new diagnosis of RA and were untreated.
Ultrasound
A Logiq 200 Pro unit (Kranzbühler, Germany) or a Acuson Sequoia® US system (Mountainview, CA, USA) was used for US examinations using a 7.5 MHz linear transducer (Loqic Pro) or a 8 MHz linear transducer (Acuson Sequoia). US of the shoulder joint was performed with standard scans according the guidelines for musculoskeletal US in rheumatology [6]. The patient was sitting with 90° flexion of the elbow joint, the hand positioned in supination on top of the patient’s thigh. Standard scans were the posterior transverse and longitudinal scan, the lateral longitudinal and transverse scan in neutral position and maximal internal rotation, the anterior longitudinal scan in neutral position and in maximal internal rotation, the acriomiocalvicular joint scan and the axillary longitudinal scan with raised arm, the arm supported in 90 abduction and the longest distance beween the humeral head and the joint capsule was measured. All joints were examined dynamically in passive external and internal rotation of the humerus with 90° flexed elbow. All examinations were performed by a fully trained and experienced examiner (SMW). Representive images were digitally scanned and were read by two independent investigators (JS and SMW) who were banded to the patients’ clinical and laboratory findings.
Synovitis was defined by widened axillary recessus ≥3 mm and/or synovial proliferation in the posterior or anterior transverse scan. Bursitis was diagnosed when the maximum diameter of the subdeltoid bursa was more than 2 mm due to sonolucent fluid with or without additional echogenic material. Bicipital tenosynovitis was diagnosed by the presence of a hypoechoic rim with a maximum diameter of more than 2 mm.
PDS
Blood flow in the synovial membrane was visualised with PDS in 44 joints with signs of synovitis, effusion, tenosynovitis and/or bursitis using Acuson Sequoia®. The intensity of blood flow inside the joint capsule, subdeltoid bursa and long biceps tendon sheath was assessed semiquantitatively and divided into four grades (0–3), as suggested by Newman et al. [7]. Zero indicated normal or minimal tissue perfusion with either no signal or only a local dark red PDS US signal. One, mild hyperemia with dark red to red signal and/or single vessel signal. Two, moderate hyperemia with red-to-orange signal and confluent vessel signal. Three, marked hyperemia with orange-to-yellow signal and marked vessel signal with more than a half of the synovia or the tissue around the bursa. The power Doppler settings were the same for all joints and all patients, standardized with a B mode frequency of 7 MHz and a colour mode frequency of 7 MHz. The gain was set just below the noise levels and ranges between 41 and 51 dB. The images were evaluated by the consensus of two independent readers.
Power Doppler sonography was performed in posterior transverse, posterior longitudinal, anterior transverse and longitudinal scans and in the axillary longitudinal scan with raised arm to measure the intensity of blood flow inside the joint capsule, subdeltoid bursa and long biceps tendon sheath. Synovial fluid was aspired, whenever ultrasound demonstrates fluid within joint spaces or within the bursa subdeltoidea.
Statistical analysis
Statistical analysis was performed using Chi-square test or Fisher’s exact test and the Mann–Whitney rank sum test. P values <0.05 were considered as statistically significant.
Results
Ultrasound findings
Glenohumeral synovitis
The ultrasound findings are summarized in Table 1. The most common US finding was effusion or synovitis in 59% (n = 92) of 157 painful glenohumeral joints and 60% (n = 59) of 99 RA patients, respectively. Synovitis was detectable in the posterior scan in 80 of 92 shoulders (87%), in the anterior scan in 20/92 shoulders (22%), and in the axillary scan in 76 out of 84 shoulder (90%). Eight shoulders were not investigated with the axillary scan due to impaired elevation of the arm. Overall, in 8 shoulders synovitis was detected by posterior scan only, in 12 shoulders by axillary scan only. Synovitis in the anterior scan was always accompanied by synovitis in the axillary or posterior scan.
Bursitis and tenosynovitis
Subdeltoid bursitis and tenosynovitis of the biceps tendon was seen in 56 (35%) and 55 (35%) shoulders, respectively. In 22 shoulders (14%) we found isolated biceps tendon sheath effusion and/or isolated effusion in the subdeltoid bursa, whereas in 68 shoulders (43%) tenosynovitis and/or bursitis was accompanied by shoulder effusion and/or synovitis. Isolated effusion and/or synovitis of the shoulder joint space occurred in further 24 shoulders (14%). Isolated effusion in the biceps tendon sheath and/or subdeltoid bursa was accompanied by osteophytes or tears of the rotator cuff in 12 out of 22 patients (54%).
Erosions
US detected joint erosions on the humeral head in 92 joints (59%). The mean disease duration was significantly longer in patients with erosions (9.9 ± 9.4 years) versus patients without erosions (mean 5.7 ± 8.7 years), p value 0.024 (Mann Withney Rank sum test).
No significant correlation was found between the presence of erosions and glenohumeral synovitis: 59/92 joints with glenohumeral synovitis and/or effusion had erosions on the humeral head (64%) compared to 33 of 65 joints without synovitis (51%), p = n.s. Erosions were associated with the presence of osteophytes in 35 shoulders.
Degenerative disorders
Overall, osteophytes were detected in 64 shoulders (41%), rotator cuff calcification in 29 shoulders (18%), and tears of the rotator cuff in 24 shoulders (15%). In 34 shoulders glenohumoral effusion or synovitis was associated with the presence of osteophytes on the humoral head. About 43 shoulder joints (27%) did not show signs of inflammation such as effusion in the glenohumeral joint, bicipital tendon sheath or subdeltoid bursa. These shoulders showed main degenerative disorders: osteophyes (n = 19), a complete or partial tear of the rotator cuff (n = 6) or calcific tendinitis (n = 15).
Correlation between ultrasound findings and CRP levels
C-reactive protein (CRP) levels were available in 95 out of 99 patients. The mean value was 3.88 mg/dL ± 5.49 (range 0.2–21 mg/dL). CRP levels were elevated (>0.2 mg/dL) in 79/95 patients (83%). A total of 16 patients (17%) were serologically inactive with CRP levels below 0.2 mg/dL. Synovial proliferation and/or effusion in at least one glenohumeral joint was found in 54/79 patients with elevated CRP levels (68%) in contrast to only 2/16 patients with normal CRP levels (12%) p = 0.0001. Thus, 32% of serologically active RA patients and 88% of inactive patients did not have glenohumeral synovitis as the cause of shoulder pain. Effusion of the biceps tendon sheath was found in 35 patients (out of 79) with elevated CRP levels in contrast to 2 (out of 16) patients with normal CRP levels (p = 0.036). Effusion in the subdeltoid bursa was present in 37 (out of 79) patients with elevated CRP levels in contrast to 1 (out of 16) patient with normal CRP levels (p = 0.006).
PDS findings
Power Doppler sonography was performed in 44 shoulders of 31 patients. The joint perfusion was within normal range in 11 joints. Increased microvascular blood flow was found in 33 shoulders (19 joints grade 1, 13 joints grade 2, 1 joints grade 3). Table 2 shows the frequency of hyperperfusion in different areas of the shoulder: The highest frequency of increased microvascular blood flow was detected within the anterior synovitis and tenosynovitis of the biceps tendon, the lowest in the widened axillary joint recessus (Table 2). In all patients with detectable hyperperfusion and bicipital tenosynovitis, increased blood flow was present inside and outside of the tendon sheath (Fig. 1c, d). In 21 joints hyperperfusion was detected in one joint area only, whereas in 11 joints multiple joint areas were involved (Table 3).
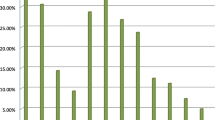
Correlation between PDS findings and CRP levels
C-reactive protein levels were significantly higher in patients with grades 1 (7.6 mg/dL ± 6.8), 2 (9.1 mg/dL ± 7.4) and 3 microvascular blood flow (23 mg/dL), compared to patients with grade 0 (2.4 mg/dL ± 1.7 mg/dL), p = 0.02. (Fig. 2).
Correlation between PDS findings and synovial fluid cell count
Synovial analysis was performed in 15 patients (punctio sicca in nine further patients). One patient with normal microvascular blood flow had a low cell count of 1,000 μL−1. In the 14 patients with increased microvascular blood flow an elevated cell count was present (median 26,000 μL−1, range 12,000–80,000). Joint infection was detected in one patient with a cell count of 80,000 μL−1 and a massive and global joint hyperperfusion grade 3 assessed by PDS (Fig. 1a).
Discussion
Clinical assessment shows low accuracy in the diagnosis of periarticular shoulder lesions compared with muskuloskeletal US [1]. US is helpful to distinguish between inflamed and degenerative lesions of the shoulder. Sonographic studies of shoulder involvement in RA showed that often both, articular and periarticular tissues, are affected [3]. In the present study we looked for different pathologies of the painful shoulder girdle in patients with serological active or inactive RA.
The frequency of synovitis in the glenohumeral joint (59%), subdeltoid bursitis (35%) and bicipital tenosynovits (35%) in our study match well with previous US studies on the rheumatoid shoulder, which found inflammation in the glenohumeral joint in 52–58%, subdeltoid bursitis in 18–69% and bicipital tenosynovitis in 32–57% [2, 3, 8].
Our study also confirms prior observations that the axillary scan is highly sensitive to detect synovitis in RA [9]. The combination of both, posterior and axillary scan lead to a 100% sensitivity for glenohumoral synovitis in our study.
The tendon sheath is merely an extension of the synovial membrane of the joint. Therefore, a generalized joint effusion can certainly lead to fluid in the sheath [10]. However, Alasaarela et al. [2] detected bicipital tenosynovitis and subdeltoid bursitis in RA patients without concomitant glenohumoral synovitis frequently. Our study confirms the finding of isolated bicipital tenosynovitis and subdeltoid bursitis as a cause of shoulder pain in patients with RA, however, at a lower rate compared to the study of Alasaarela (6 and 9.5% vs. 17 and 23%, respectively) [2]. However, different sensitivities in the detection of glenohumoral synovitis may lead to this discrepancy.
Shoulder pain may occur in serologically active as well as inactive RA. A painful shoulder girdle on palpation or motion may not necessarily be caused by synovitis. Otherwise, glenohumeral synovitis may occur in serologically inactive RA. Thus, discrepancies between biomarkers of disease activity and the presence of shoulder synovitis may be frequent in patients with new onset of shoulder pain. Our study shows that only 68% of active RA patients and 12% of serologically inactive RA patients have glenohumeral synovitis as the cause of new onset of shoulder pain, underlining the need for musculoskeletal US in the evaluation of the shoulder in RA.
On gray-scale US the visualization of inflammation is restricted to the detection of synovial hypertrophy and fluid collection, enhanced by dynamic examination. The diagnostic accuracy of gray-scale US is hampered by low specificity, especially biceps tendon fluid and subdeltoid bursal fluid may be present in asymptomatic or degenerative shoulders [5, 11, 12]. Schmidt et al. [13] recently demonstrated a high frequency of small amounts of fluid in the subdeltoid bursae (85%), erosions >1 mm (23%), and fluid around long biceps tendon (27%) in healthy subjects. Moreover, Schmidt et al. [13] showed that the sagittal axillary recessus at the middle of the concavitiy of the humeral neck was found to be mean 2.2 mm, ranging between 0.4 and 6.2 mm. The broad range of standard reference values in US examination of the shoulder underlines the need for other methods to prevent misinterpretation of discrete fluid or irregularities of the bone surface as signs of arthritis, bursitis or tenosynovitis. PDS allows detection of flow in the examined tissues [14]. We used a semi-quantitative method of evaluation that is easily applicable in daily clinical practise. Analysis of interobserver variation for power Doppler signal shows good results [15]. Many research groups have reported promising results of studies analysing the use of PDS in RA [7, 16]. Only few studies focused on the shoulder [5]. The latter study of Strunk et al. [5] found PDS signals localized inside the tendon sheath in 91.7% of RA patients with shoulder pain in contrast to 0% of patients with degenerative shoulder disorders. The data of Strunk et al. [5] suggest that in RA the reason for fluid in the tendon sheath is exudative and proliferative synovitis within the peritendinous synovial membrane and not a generalized joint effusion within the glenohumeral joint. In accordance with findings of Strunk et al. our data show an increased PDS signal inside and outside the tendon sheath in 85% of shoulders with signs of tenosynovitis in B mode sonography.
Additionally, we searched for other sites of inflammation, especially the subdeltoid bursa and the glenohumoral joint space. We found that the probability to visualize angiogenesis differs within the sites of shoulder tissue, thus PDS signals were detected less frequently in synovial tissue of the axillary recessus than in the dorsal or ventral joint space or the subdeltoid bursa. The reason for this difference is unclear, mechanical stress is unlikely to be main cause of a different distribution of vessel profileration or vasodilatation. For instance, impingement or instability of degenerative shoulder joints does not show significant hyperperfusion detectable by PDS. Furthermore, our study shows that widening of the axillary joint recessus represents hypoechoic fluid and not synovialitis in most cases. In line with our interpretation, a simple intraarticular injection of physiological NaCl also leads to widening of the axillary joint recessus in the axillary scan [9].
The correlation between CRP levels, high synovial cell counts and the increased microvascular blood flow, suggests that an increased microvascular blood flow in the articular and periarticular shoulder tissue is associated with a high inflammatory activity. Since the shoulder is a major joint, it is reasonable to assume that inflammation in this joint necessarily will lead to elevated CRP levels. In contrast, previous studies on Doppler sonography of rheumatoid hands and knees have shown only weak correlation between CRP levels, erythrocyte sedimentation rate and local signs of disease activity in individual joints [17, 18]. In one case of the present study a very high synovial blood flow was associated with secondary shoulder infection. Thus further studies are necessary to clarify, whether PDS is a reliable tool for diagnosing bacterial joint infection.
In summary, our study shows that the site of inflammatory exudate varies considerably between individual RA patients with shoulder pain. Rheumatoid shoulder pain may not be caused by glenohumeral synovitis in 32% of patients, despite serologically active RA. Thus, the use of US and PDS is strongly recommended to elucidate the origin of inflammatory and noninflammatory shoulders and to determine the degree of inflammation in rheumatoid shoulder involvement.
References
Naredo E, Aguado P, De Miguel E, Uson J, Mayordomo L, Gijon-Banos J, Martin-Mola E (2002) Painful shoulder: comparison of physical examination and ultrasonographic findings. Ann Rheum Dis 61:132–136
Alasaarela EM, Alasaarela EL (1994) Ultrasound evaluation of painful rheumatoid shoulders. J Rheumatol 21:1642–1648
Coari G, Paoletti F, Iagnocco A (1999) Shoulder involvement in rheumatic diseases. Sonographic findings. J Rheumatol 26:668–673
Lange U, Piegsa M, Teichmann J, Neeck G (2000) Ultrasonography of the glenohumeral joints—a helpful instrument in differentiation in elderly onset rheumatoid arthritis and polymyalgia rheumatica. Rheumatol Int 19:185–189
Strunk J, Lange U, Kurten B, Schmidt KL, Neeck G (2003) Doppler sonographic findings in the long bicipital tendon sheath in patients with rheumatoid arthritis as compared with patients with degenerative diseases of the shoulder. Arthritis Rheum 48:1828–1832
Backhaus M, Burmester GR, Gerber T, Grassi W, Machold KP, Swen WA, Wakefield RJ, Manger B (2001) Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis 60:641–649
Newman JS, Laing TJ, McCarthy CJ, Adler RS (1996) Power Doppler sonography of synovitis: assessment of therapeutic response—preliminary observations. Radiology 198:582–584
Cantini F, Salvarani C, Olivieri I, Niccoli L, Padula A, Macchioni L, Boiardi L, Ciancio G, Mastrorosato M, Rubini F, Bozza A, Zanfranceschi G (2001) Shoulder ultrasonography in the diagnosis of polymyalgia rheumatica: a case-control study. J Rheumatol 28:1049–1055
Koski JM (1989) Axillar ultrasound of the glenohumeral joint. J Rheumatol 16:664–667
Middleton WD, Reinus WR, Totty WG, Melson GL, Murphy WA (1985) US of the biceps tendon apparatus. Radiology 157:211–215
Arslan G, Apaydin A, Kabaalioglu A, Sindel T, Luleci E (1999) Sonographically detected subacromial/subdeltoid bursal effusion and biceps tendon sheath fluid: reliable signs of rotator cuff tear? J Clin Ultrasound 27:335–339
Neumann CH, Holt RG, Steinbach LS, Jahnke AH Jr, Petersen SA (1992) MR imaging of the shoulder: appearance of the supraspinatus tendon in asymptomatic volunteers. AJR Am J Roentgenol 158:1281–1287
Schmidt WA, Schmidt H, Schicke B, Gromnica-Ihle E (2004) Standard reference values for musculoskeletal ultrasonography. Ann Rheum Dis 63:988–994
Schmidt WA, Volker L, Zacher J, Schlafke M, Ruhnke M, Gromnica-Ihle E (2000) Colour Doppler ultrasonography to detect pannus in knee joint synovitis. Clin Exp Rheumatol 18:439–444
Szkudlarek M, Court-Payen M, Jacobsen S, Klarlund M, Thomsen HS, Ostergaard M (2003) Interobserver agreement in ultrasonography of the finger and toe joints in rheumatoid arthritis. Arthritis Rheum 48:955–962
D’Agostino MA, Said-Nahal R, Hacquard-Bouder C, Brasseur JL, Dougados M, Breban M (2003) Assessment of peripheral enthesitis in the spondylarthropathies by ultrasonography combined with power Doppler: a cross-sectional study. Arthritis Rheum 48:523–533
Terslev L, Torp-Pedersen S, Savnik A, von der Recke P, Qvistgaard E, Danneskiold-Samsoe B, Bliddal H (2003) Doppler ultrasound and magnetic resonance imaging of synovial inflammation of the hand in rheumatoid arthritis: a comparative study. Arthritis Rheum 48:2434–2441
Carotti M, Salaffi F, Manganelli P, Salera D, Simonetti B, Grassi W (2002) Power Doppler sonography in the assessment of synovial tissue of the knee joint in rheumatoid arthritis: a preliminary experience. Ann Rheum Dis 61:877–882
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stegbauer, J., Rump, L.C. & Weiner, S.M. Sites of inflammation in painful rheumatoid shoulder assessed by musculoskeletal ultrasound and power Doppler sonography. Rheumatol Int 28, 459–465 (2008). https://doi.org/10.1007/s00296-007-0465-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-007-0465-8