Abstract
Osteoporosis is a common complication in patients with end-stage liver disease and after orthotopic liver transplantation (LT), with resulting increasing fracture rate. In this study, we investigated the role of treatment with pamidronate in preventing further bone loss after LT. Eighty-five patients with end-stage liver disease were included in the study. Pamidronate 30 mg was given intravenously every 3 months after LT for the duration of 1 year to 43 patients with osteopenia or osteoporosis prior LT. The remainders served as controls. All patients received a supplementation of calcium and vitamin D. Bone mineral density (BMD) at the lumbar spine and the femoral neck, and markers of bone metabolism were measured before and 12 months after LT. Sixty-two BMD were available at 12 months; only paired BMD were evaluated. A significant increase in lumbar spine BMD was observed in pamidronate treated patients. No change was evident in controls. Femoral neck BMD decreased in both treated and untreated patients. Osteocalcin serum levels and deoxypyridinoline urinary excretion were significantly reduced by treatment. Our study suggests that pamidronate decreases bone turnover and is effective in preventing the course of bone loss after LT, however the efficacy, at the dosage regimen employed and in a follow-up of 12 months, appears to be limited to trabecular bone, with no effect on the cortical structure of the femur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
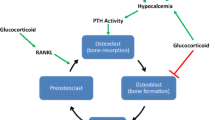
Organ transplantation is the treatment of choice for many patients with end-stage liver disease. Although life expectancy is markedly increased after transplantation, the quality of life of these patients is often impaired by the high occurrence of osteoporosis with resulting high fracture rate [1]. Moreover, osteoporosis is a common complication in individuals with end-stage liver disease, as many factors such as vitamin D deficiency, hypogonadism, immobility, and malnutrition contribute to increase bone loss and to lower bone mineral density (BMD) prior to orthotopic liver transplantation (LT) [2–5]. After LT, further deterioration of bone metabolism takes place as a consequence of immunosuppressive therapy. Glucocorticoids [6], tacrolimus (FK 506), and cyclosporine (Cs) [7] are responsible for accelerated bone turnover, particularly in the first 3–12 months after LT. Immobilization could also be a contributing factor [8]. The positive effect of bisphosphonates in prevention and treatment of corticoid-induced osteoporosis is well recognized [9, 10], however, although corticosteroids are frequently used as immunosuppressive drugs after LT, the use of bisphosphonates to prevent bone loss is not generally applied. Alendronate [11] and etidronate [12] have been used to prevent bone loss and osteoporotic fractures in liver transplant recipients, with positive effects or no effect at all, respectively. Pamidronate, a potent nitrogen containing bisphosphonate, has been employed in prospective randomized studies after renal [13], cardiac [14], and lung [4] transplantation. Although different therapeutic approaches have been used, pamidronate proved effective in preventing bone loss in the first year after transplantation. Literature data on the use of pamidronate in patients with LT are conflicting. Reeves et al. [15] reported that three-monthly infusion of pamidronate, starting before graft and continuing up to 9 months post-operatively, reduced vertebral fracture risk. On the other hand, Ninkovic et al. [16] reported no efficacy of a single intravenous infusion of pamidronate, given pre-operatively, in preventing bone loss and osteoporotic fractures during the first year after orthotopic LT.
The aim of this prospective study was to evaluate the efficacy of pamidronate to prevent further bone loss during the first year after LT. In addition, we measured bone metabolism parameters to evaluate any additive information to that derived from BMD measurements.
Patients and methods
Patients
Eighty-five patients with chronic liver diseases (58 men, 23 women, mean age 54.7 ± 10.0) having received orthotopic LT were studied. The study was approved by the local ethics committee and informed consent was obtained by all patients. The cause of liver disease was: cirrhosis of viral origin (n=46), alcoholic cirrhosis (n=18), sclerosing cholangitis (n=8), and others (n=9). None of the patients was receiving anti-osteoporosis treatment before transplantation. All women except three were post-menopausal but did not receive hormonal replacement therapy. Oral calcium (1 g/day) and vitamin D (800–1,000 IU/day) supplements were given to all patients from the time of transplantation. Forty-three patients (23 men, 20 women) received pamidronate 30 mg intravenously every 3 months. All patients were operated and followed during the same period of time.
Immunosuppressive therapy consisted of prednisone, Cs, and azathioprine. Maintenance treatment consisted of an association of Cs or tacrolimus with azathioprine and prednisone. A 500 mg pulse of intravenous methylprednisolone was given perioperatively. The median daily doses of prednisolone after orthotopic LT were 20 mg at first month with a progressive dose reduction until the 60-month post-transplantation. Thirty-two patients out of 81 received only 500 mg of prednisone IV in anhepatic phase and no steroids thereafter, in accord to a new protocol started in 2003. Acute rejections were treated with 1 g IV of methylprednisolone and/or antilymphocyte globulins (ATGAM; Pharmacia and Upjohn, USA, or ATG Fresenius Pharma AG, Switzerland). The work described in this article has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki).
Treatment
Patients with osteoporosis or osteopenia in either the lumbar spine or the femoral neck, a total of 47 patients, were assigned to treatment with pamidronate.
Four of them had severe complications in post-transplantation [cerebral haemorrhage (one) and acute renal failure (three)] and were then excluded before treatment with pamidronate was started. The remaining 43 (53%) patients were given pamidronate 30 mg intravenously every 3 months for 1 year. The remainders 38 patients (who had a baseline BMD T-score >−1 served as controls).
Bone mass measurements
Areal BMD was evaluated by DXA (dual-energy X-ray absorpiometry) using Hologic QDR-2000 bone densitometers (Hologic Inc., Waltham, MA, USA), at lumbar spine (L2–L4) and proximal femur (femoral neck). The precision of lumbar spine measurements in vivo was 1.0% for the lumbar spine and 1.6% for the hip. DXA measurements were performed at the time of inclusion on the list of transplant candidates and 12 months after transplantation. Median interval between pre-transplantation BMD measurement and LT was 6.2 months. BMD results (areal BMD in g/cm2) were transformed to T-scores (calculated as the difference between the actual measurement and the mean value of healthy gender-matched adult controls, divided by their standard deviation), from the data provided by the densitometers manufacturer. Osteoporosis was classified by a T-score of below −2.5 in either lumbar spine or femur, and osteopenia by a T-score between −2.5 and −1. BMD changes during follow-up are expressed as a percentage difference. Only clinical fractures were recorded.
Biochemistry
Plasma and urinary calcium, phosphate, and creatinine were measured. Plasma calcium was adjusted for protein levels [adjusted calcium = measured calcium/((protein/160) + 0.55)]. Osteocalcin was determined with an immunoradiometric assay (CIS-Bio, Gif-sur-Yvette, France, n.v.=23.0 ± 9.7 μg/l). Urinary deoxypyridinoline (D-Pyr), a marker of bone resorption, was measured by fluorescence emission after acid hydrolysis and high-performance liquid chromatography separation (Bio-Rad System, Munich, Germany), and is expressed as nmol/mmol of creatinine (n.v.=9.2 ± 4.6 nmol/mmol). Serum parathyroid hormone was measured using a two-site chemiluminescent immunometric assay (Immulite; Diagnostic Products Corp., Los Angeles, CA, USA; reference range, 1.06–6.9 pmol/l). Serum 25-hydroxyvitamin D3 (25OHD3) was measured by a chemiluminescence assay (Nichols Advantage, Nichols Institute, San Clemente, CA, USA; reference range, 25–120 nmol/l). Biochemistry was performed before transplantation and 12 months post-LT.
Statistical analysis
All data are expressed as means ± SD. Statistical significance of differences was assessed by a two-tailed Student’s t-test or analysis of variance for intergroups comparison. A paired Student’s t-test was used to assess the statistical significance of changes in laboratory values at 12 months compared with baseline. A P value of less than 0.05 was considered significant. Multiple regression analysis was performed to evaluate the dependency of the % variation of bone loss on continue and discontinue variables. In order to evaluate probability of significant decrease in BMD at either site (lumbar spine and femoral neck) logistic regression analysis was performed based on age, sex, underlying liver disease, child class, and number of rejections, as variables.
Results
Patients’ baseline characteristics are reported in Table 1. They differed for the aetiology of underlying liver disease and for baseline lumbar and femoral BMD. Sixty-two BMD were available at 12 months (24 from the treated group and 38 from control group). Only paired BMD were evaluated. Prior to transplantation, osteoporosis at either L2–L4 or femoral neck was present in 54% of pamidronate group and in 23% of controls (P<0.01).
No significant bone loss in the spine was observed at 12 months after LT either in untreated or treated patients (−0.58 and −0.11% compared to baseline, P=0.30 and 0.48, respectively). However, when adjusted for age and sex, lumbar spine BMD in the pamidronate group significantly increased (P<0.003), whereas it remained unchanged in the controls (Table 2). Over 12 months, femoral neck BMD significantly decreased in both treated and untreated patients (−4.7 and −5.9%; P<0.001 vs. pre-transplant values, respectively). Similarly, total hip BMD decreased in both groups (−3.7 and −5.0%, P<0.002 and 0.001, in treated and untreated patients, respectively). In a model of multivariate and logistic analysis including age, sex, severity of disease (child class), and cumulative dose of steroids, there was no effect of the treatment on BMD at both femoral neck and total hip (data not shown). The prevalence of clinical fracture at baseline was of 13% in controls and 16% in the treated group (P=0.6). During the 12 months of follow-up, four patients experienced clinical fractures of radius, ankle, and ribs (one in the treated group and three in the controls) (Table 1).
Biochemical data are reported in Table 3. Serum total calcium, corrected serum calcium, and phosphate values were in the normal range and remained unchanged over 12 months Parathyroid hormone concentrations were increased at 12 months in both groups compared to the baseline values. At baseline, 25OHD3 mean levels were 25.3 ± 14.9 and 30.5 ± 16.7 nmol/l in treated and control group, respectively, and significantly increased in both groups at 12 months. Mean pre-transplantation osteocalcin serum levels were lower than in healthy controls, but significantly increased at 12 months in untreated patients. Urinary D-Pyr excretion was significantly reduced in pamidronate treated patients.
Discussion
Literature data show that the prevalence of bone disease in patients undergoing LT is high, however there is an impressive shortage of studies on treatment of osteoporosis carried out in liver transplant recipients. Published reports suggest that bisphosphonates are the most promising agents for the prevention and treatment of post-LT osteoporosis, although controversies still remain regarding dose regimen and duration of therapy. In this study, we report that pamidronate administered three-monthly during the first year after LT significantly increased lumbar spine BMD in treated patients compared to controls. Treatment had no protective effect on femoral bone loss, as femoral neck BMD fell comparably in treated and untreated patients. Pamidronate effects on BMD have been investigated after renal [13], cardiac [14], and lung [4] transplantation, with conflicting result: the beneficial effects of pamidronate therapy in spine BMD has been shown in cardiac, renal, and pulmonary transplanted patients using different regimens of pamidronate infusion which prevented bone loss compared with placebo-groups, or calcium and vitamin D alone therapy; in a recent randomized study, Ninkovic et al. [16] showed the lack of effect of a single pre-transplantation intravenous infusion (60 mg) of pamidronate on spine mineral density, while Dodidou et al. [17] demonstrated an increase in lumbar spine BMD over 12 months after LT in patients treated with pamidronate. The effects of antiresorptive therapy with pamidronate on femoral neck BMD are conflicting: Krieg et al. [18] reported the efficacy of cyclic pamidronate treatment in increasing not only lumbar spine but also femoral neck BMD in cardiac transplant recipients. However, data in LT are limited: Ninkovic et al. [16] demonstrated no protective effect of pamidronate (60 mg before transplantation) in femoral bone density. In the study by Dodidou et al. [17], an increase of the femoral neck BMD was not evident until 18–24 months of treatment, accounting for the fact that the efficacy of bisphosphonates could be related to the remodelling rate [19], which is higher in trabecular than in cortical bone. Giannini et al. [20] consistently reported that in a group of LT patients followed up to 2 years, the femoral bone density showed a tendency towards restoration 12–18 months after transplantation. In a histomorphometric study performed in LT patients, Vedi et al. [21] showed only a partial effect of a single infusion of 60 mg of pamidronate before transplantation in reducing erosion cavity size, suggesting that a higher dosage would be required for an effective reduction of bone turnover. We evaluated the prevalence and incidence of clinical fractures. At baseline, seven patients in treated and five patients in control group have had fractures. Twelve months after transplantation, three patients in the untreated group and one patient in the treated group reported fractures. The sample was however too small to reach statistical significance. Reeves et al. [15] reported that the administration of pamidronate 60 mg every 3 months reduced the risk of vertebral fracture in LT patients. Unfortunately, we were not able to evaluate prevalence and incidence of vertebral fractures in our patients.
Changes in bone turnover was studied by measuring biochemical parameter of bone formation and resorption before transplantation (median interval of 3 months) and at 12 months after transplantation. Pre-transplantation PTH serum levels were in the normal range and significantly increased after transplantation (P<0.001) in agreement with previous findings [22, 23]. An impairment of renal function caused by renal effects of immunosuppressive therapy may contribute to the development of secondary hyperparathyroidism, however, no correlation between PTH and creatinine values was found in LT patients [23]. In our patients, the mean of GFR in the two groups at 12 months was 58.11 ml/min and the correlation between PTH and GFR at 1 year did not reach statistical significance (P=0.15). We were unable to demonstrate any relationship between vitamin D, BMD, and PTH, corroborating the findings of other authors [24, 25].
Before transplantation, serum levels of osteocalcin (a marker of bone formation) were lower than in healthy controls, consistent with earlier observations in patients with chronic liver diseases [26], but were significantly increased in untreated patients 12 months after transplantation, accounting for the increase in bone turnover which takes place after LT [26–28]. The observed increase in D-Pyr urinary excretion (marker of bone resorption) in untreated LT recipients corroborates this evidence. Pamidronate, as expected, caused a decrease in bone turnover, with resulting decrease in both osteocalcin and D-Pyr concentrations.
In conclusion, our results suggest that pamidronate therapy started immediately after LT in patients with low bone mass is effective in increasing lumbar spine BMD, but has no effect in preventing further bone loss at the femoral neck and the total hip. We have no information on BMD in the first months after liver transplant, as biochemical and densitometric data were obtained before and 1 year after treatment, so it is not possible to check the influence of pamidronate during this period, in which most of the skeletal fractures are developed. However, the possibility that pamidronate causes an increase of femoral BMD in the first months, and a decrease thereafter seems highly hypothetical and, in fact, unlikely. The most likely explanation could be a relative insensitivity of cortical bone (which femoral neck is mainly made of) to respond to pamidronate within 1 year. A long-term study of bone mass changes could possibly produce more information.
One drawback of this study is that it is not a randomized investigation. It should be stressed that randomization is not strictly necessary because we treated all osteoporotic patients; moreover, pamidronate and other bisphosphonates have demonstrated their efficacy in the treatment of steroid-induced osteoporosis. The difference between treatment groups with respect to bone mass could not be an important limitation, since both groups continue to lose bone at femoral neck, regardless of treatment, allowing us to conclude that pamidronate was not effective at this skeletal site in our transplanted patients.
Despite data from clinical trials suggest that bisphosphonates are the safest and most promising agents for treatment of post-transplantation osteoporosis [29], the role of antiresorptive therapy in patients after LT has not yet been fully defined, and further randomized studies are needed.
References
Leidig-Bruckner G, Hosch S, Dodidou P, Ritschel D, Conradt C, Klose C, Otto G, Lange R, Theilmann L, Zimmerman R, Pritsch M, Ziegler R (2001) Frequency and predictors of osteoporotic fractures after cardiac or liver transplantation: a follow-up study. Lancet 357:342–347
Monegal A, Navasa M, Guanabens N, Peris P, Pons F, Martinez de Osaba MJ, Rimola A, Rodes J, Munoz-Gomez J (1997) Osteoporosis and bone mineral metabolism disorders in cirrhotic patients referred for orthotopic liver transplantation. Calcif Tissue Int 60:148–154
Shane E, Mancini D, Aaronson K, Silverberg SJ, Seibel MJ, Addesso V, McMahon DJ (1997) Bone mass, vitamin D deficiency, and hyperparathyroidism in congestive heart failure. Am J Med 103:197–207
Trombetti A, Gerbase MW, Spiliopoulos A, Slosman DO, Nicod LP, Rizzoli R (2000) Bone mineral density in lung-transplant recipients before and after graft: prevention of lumbar spine post-transplantation-accelerated bone loss by pamidronate. J Heart Lung Transplant 19:736–743
Mikuls TR, Julian BA, Bartolucci A, Saag KG (2003) Bone mineral density changes within six months of renal transplantation. Transplantation 75:49–54
Kanis JA, Johansson H, Oden A, De Laet C, Johnell O, Eisman JA, Mc Closkey E, Mellstrom D, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19:893–899
Abdelhadi M, Ericzon BG, Hultenby K, Sjoden G, Reinholt FP, Nordenstrom J (2002) Structural skeletal impairment induced by immunosuppressive therapy in rats: cyclosporine A vs tacrolimus. Transpl Int 15:180–187
Bikle DD, Sakata T, Halloran BP (2003) The impact of skeletal unloading on bone formation. Gravit Space Biol Bull 16:45–54
Boutsen Y, Jamart J, Esselinckx W, Stoffel M, Devogelaer JP (1997) Primary prevention of glucocorticoid-induced osteoporosis with intermittent intravenous pamidronate: a randomized trial. Calcif Tissue Int 61:266–271
Saag KG, Emkey R, Schnitzer TJ, Brown JP, Hawkins F, Goemaere S, Thamsborg G, Liberman UA, Delmas PD, Malice MP, Czachur M, Daifotis AG (1998) Alendronate for the prevention and treatment of glucocorticoid-induced osteoporosis. Glucocorticoid-Induced Osteoporosis Intervention Study Group. N Engl J Med 339:292–299
Millonig G, Graziadei IW, Eichler D, Pfeiffer KP, Finkenstedt G, Muehllechner P, Koenigsrainer A, Margreiter R, Vogel W (2005) Alendronate in combination with calcium and vitamin D prevents bone loss after orthotopic liver transplantation: a prospective single-center study. Liver Transpl 11:960–966
Riemens SC, Oostdijk A, van Doormaal JJ, Thijn CJ, Drent G, Piers DA, Groen EW, Meerman L, Slooff MJ, Haagsma EB (1996) Bone loss after liver transplantation is not prevented by cyclical etidronate, calcium and alphacalcidol. The Liver Transplant Group, Groningen. Osteoporos Int 6:213–218
Fan SL, Almond MK, Ball E, Evans K, Cunningham J (2000) Pamidronate therapy as prevention of bone loss following renal transplantation. Kidney Int 57:684–690
Bianda T, Linka A, Junga G, Brunner H, Steinert H, Kiowski W, Schmid C (2000) Prevention of osteoporosis in heart transplant recipients: a comparison of calcitriol with calcitonin and pamidronate. Calcif Tissue Int 67:116–121
Reeves HL, Francis RM, Manas DM, Hudson M, Day CP (1998) Intravenous bisphosphonate prevents symptomatic osteoporotic vertebral collapse in patients after liver transplantation. Liver Transpl Surg 4:404–409
Ninkovic M, Love S, Tom BD, Bearcroft PW, Alexander GJ, Compston JE (2002) Lack of effect of intravenous pamidronate on fracture incidence and bone mineral density after orthotopic liver transplantation. J Hepatol 37:93–100
Dodidou P, Bruckner T, Hosch S, Haass M, Klar E, Sauer P, Ziegler R, Leidig-Bruckner G (2003) Better late than never? Experience with intravenous pamidronate treatment in patients with low bone mass or fractures following cardiac or liver transplantation. Osteoporos Int 14:82–89
Krieg MA, Seydoux C, Sandini L, Goy JJ, Berguer DG, Thiebaud D, Burckhardt P (2001) Intravenous pamidronate as treatment for osteoporosis after heart transplantation: a prospective study. Osteoporos Int 12:112–116
Fromm GA, Vega E, Plantalech L, Galich AM, Mautalen CA (1991) Differential action of pamidronate on trabecular and cortical bone in women with involutional osteoporosis. Osteoporos Int 1:129–133
Giannini S, Nobile M, Ciuffreda M, Iemmolo RM, Dalle Carbonare L, Minicuci N, Casagrande F, Destro C, Gerunda GE, Sartori L, Crepaldi G (2000) Long-term persistence of low bone density in orthotopic liver transplantation. Osteoporos Int 11:417–424
Vedi S, Ninkovic M, Garrahan NJ, Alexander GJ, Compston JE (2002) Effects of a single infusion of pamidronate prior to liver transplantation: a bone histomorphometric study. Transpl Int 15:290–295
Compston JE, Greer S, Skingle SJ, Stirling DM, Price C, Friend PJ, Alexander G (1996) Early increase in plasma parathyroid hormone levels following liver transplantation. J Hepatol 25:715–718
Floreani A, Fries W, Luisetto G, Burra P, Fagiuoli S, Boccagni P, Della Rovere GR, Plebani M, Piccoli A, Naccarato R (1998) Bone metabolism in orthotopic liver transplantation: a prospective study. Liver Transpl Surg 4:311–319
Hay JE, Dickson ER, Weisner RH, Kron RAF (1990) Long-term effect of orthotopic liver transplantation on the osteopenia of primary biliary cirrhosis (abstract). Hepatology 12:838
Valero MA, Loinaz C, Larrodera L, Leon M, Moreno E, Hawkins F (1995) Calcitonin and bisphosphonates treatment in bone loss after liver transplantation. Calcif Tissue Int 57:15–19
Watson RG, Coulton L, Kanis JA, et al (1990) Circulating osteocalcin in primary biliary cirrhosis following liver transplantation and during treatment with ciclosporin. J Hepatol 11:354–358
Diamond T, Stiel D, Lunzer M, Wilkinson M, Roche J, Posen S (1990) Osteoporosis and skeletal fractures in chronic liver disease. Gut 31:82–87
McDonald JA, Dunstan CR, Dilworth P, Sherbon K, Sheil AG, Evans RA, McCaughan GW (1991) Bone loss after liver transplantation. Hepatology 14:613–619
Cohen A, Ebeling P, Sprague S, Shane E (2003) Transplantation osteoporosis. In: Favus MJ (eds) Primer on the metabolic bone diseases and disorders of mineral metabolism. American Society for Bone and Mineral Research, Washington, pp 370–379
Acknowledgements
We thank the team of the service of nuclear medicine for the BMD measurements, and the whole group of solid organ transplantation for patients care.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pennisi, P., Trombetti, A., Giostra, E. et al. Pamidronate and osteoporosis prevention in liver transplant recipients. Rheumatol Int 27, 251–256 (2007). https://doi.org/10.1007/s00296-006-0196-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-006-0196-2