Abstract
The goal of this study was to determine whether hyaluronic acid (HA) or progressive knee exercises (PE) can improve functional parameters in patients with osteoarthritis (OA) of the knee. In a prospective clinical trial 200 knees (105 patients) with radiographic Kellgren Lawrence grade III OA were randomized and received either three intra-articular injections of hyaluronic acid (Hylan G-F 20) at one-week intervals or PE for 6 weeks. Patients were evaluated by use of the Hospital for Special Surgery (HSS) Knee Score and followed-up for 18 months. Total HSS score for HA and PE patients improved from 62.6±13.8 to 88.8±11.1 and from 65.4±12.3 to 88.3±9.1, respectively, at the end of the trial (P<0.01). There were no statistically significant differences between the groups. Twenty-one patients of the HA group were excluded from the study because they had received another form of therapy. All patients in the PE group completed the trial. The patients who dropped out had also significant improvement from 57.0±12.9 to 76.7±11.9 (P<0.01). This prospective randomized trial confirmed that both HA injections and PE result in functional improvement. HA injections also increase the levels of satisfaction of the OA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current therapeutic strategies in osteoarthritis (OA) of the knee are challenging. Although several options are available for symptomatic treatment of OA including simple, analgesics, non-steroidal anti-inflammatory drugs (NSAID), weight loss, exercise and physical therapy, intra-articular injection of corticosteroids and hyaluronic acid (HA) preparations, no medical intervention has been shown to halt disease progression or reverse joint damage [1–3].
Hyaluronic acid is an unbranched high-molecular-weight polysaccharide distributed throughout the body [4] and is an important component of synovial fluid and cartilage [5]. Randomized, controlled clinical trials of intra-articular injections of HA for knee OA have produced variable results [2, 4–18]. These trials have included patients of different age, disease severity, number of injections, and duration of follow-up. Although these trials have compared HA with placebo [4, 7, 8, 12, 15–18], NSAID [6, 19], corticosteroids [13, 14, 20, 21], or mucopolysaccharide polysulfuric acid ester [22], review of the literature revealed only one study comparing the effects of HA with those of physical therapy [23], even though the benefits of exercise therapy to OA patients are well known [24, 25].
The aim of this study was to compare the effects of HA injections with progressive knee exercise (PE) in a randomized clinical trial with long-term follow-up.
Materials and methods
The series consisted of 105 patients (200 knees) with primary OA of the knee as defined by the American College of Rheumatology criteria [26], and all were seeking treatment. All patients had Kellgren Lawrence grade III OA with narrowing of joint space and sclerosis of the subchondral bone [27]. Any patient with radiographic appearance of pseudocysts was defined as Kellgren Lawrence grade IV OA and excluded from the study. All radiographs (AP, lateral, Merchant) and were evaluated by two of us (VK, IG) and if consensus was not achieved the patient was not included in the study.
All patients were assessed with full medical examination and details of medication during the last year. Patients receiving NSAID were asked to discontinue them for the duration of the study, beginning from 15 days before the study. If this was not possible, because of other diseases, the patients were excluded from the study.
Exclusion criteria included previous fracture around the knee, inflammatory arthritis, previous intra-articular injections or any other invasive procedure in the knee, significant comorbidity (renal, hepatic, or heart disease), and chicken or egg allergy.
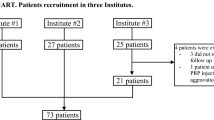
After written informed consent of the patients was received, patients with bilateral knee involvement (95 patients) were given a number and, by drawing lots with a computer program (Excel 2000), 48 of them were enrolled into the HA group and 47 into the PE group. The remaining ten patients with unilateral involvement were distributed into the groups, four for the HA group and six for the PE group, by the same method. As a result there were 100 knees in each group (52 patients in the HA group and 53 in the PE group).
Before the treatment the knee function of all patients was evaluated using the Hospital for Special Surgery (HSS) Knee Score criteria that is based on a total of 100 points. The score is divided in to seven categories: pain, function, range of motion, muscle strength, flexion deformity, instability, and subtractions. Scores from 100 to 85 points are considered excellent; scores from 84 and 70 are good; scores from 69 to 60 are fair, and scores less than 60 are considered poor [28].
The HA group received three injections of hyaluronic acid (Synvisc; Hylan G-F 20, Wyeth, Turkey) separated by one-week intervals. In bilateral cases, both knees were injected.
The exercise program included a series of progressive, simple, range of motion and resistance exercises for six weeks. The exercise program was taught to the participants by two physical therapists (ZG and AS) and performed in home-based regimen, with the patients coming to the hospital at 1, 2, 3, and 6 weeks to learn the exercises. The details of PE program are displayed in Table 1.
All patients in both groups were evaluated at 1, 2, 3, 6 weeks and after 3, 6, 12, and 18 months by a physical therapist who was blind to the study.
intent-to-treat analyses
The results of treatment were assessed during each patient visit. In the intent-to-treat analysis the study was designed to have 80% power to detect a 1-unit difference between the two treatment groups with respect to the total HSS scores for each of the end points, with 5% Type I error in two-sided hypothesis tests. All patients who received at least one intra-articular HA injection were included in the intent-to-treat analyses. In addition to the analyses of the intent-to-treat population, analyses were done on patients who completed the study and had no major protocol violations. Progress of patients in both groups was analysed by the Kaplan–Meier method [29]. Change from baseline within treatment groups was assessed using Wilcoxon’s signed ranks test, whereas differences between treatment groups were assessed using Mann–Whitney U tests. χ2 tests were used to analyse categorical variables. Analysis of variance with repeated measures was applied to the efficacy data from the beginning of the study to 18 months of follow-up. A P value of <0.05 was considered significant. All data analysis was performed using SPSS for Windows, version 10.0.
Patients, who were dropped from the study for any reason were evaluated separately.
Results
intent-to-treat population
The 105 patients constituted the intent-to-treat population. The demographic data and the baseline disease characteristics at the start of the trial are displayed in Table 2. There were no statistically significant differences between demographic data or clinical data used in the study.
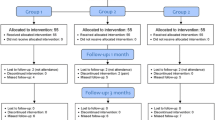
Discontinuation of treatment
In the intent-to-treat population, 31 patients in the HA group (59.6%) and 53 patients in the PE group (100%) completed the 18-month study. Progress of patients is displayed in Fig. 1. The causes of discontinuation are listed in Table 3.
Effectiveness population
The effectiveness population consisted of 84 patients (31 patients in the HA group and 53 patients in the PE group) who completed the 18-month study without major violations. The demographic data and the baseline disease characteristics at the start of the trial are listed in Table 2. There were no statistically significant differences among demographic or clinical data in the intent-to-treat population. After drop out of 21 patients, however, the PE group had more women.
Treatment outcomes, as the change from the baseline, are given in Table 4. Although there were improvements in all parameters used in the study for both HA and PE groups in the first 6 months, some differences between the groups were detected. At 1, 2, 3, and 6 weeks, the improvement in pain during transfer activity was statistically significant in favour of the PE group (P=0.042, 0.000, 0.010, and 0.024, respectively). After that time statistically significant differences were measured between the HA group and the PE group, for example pain during activity (6 weeks and 3 months), walking distance (3 months), and total HSS score at 3 months (P=0.039, 0.001, 0.012, 0.023, respectively). Although all patients improved when compared with baseline values, there were no statistically significant differences between the groups at six months (Table 4).
Table 4 shows the improvement that had occurred in each parameter at 12 and 18 months. Although all patients in the PE group completed the trial, 21 patients (42 knees) of the HA group were excluded from the study for various reasons. These patients were evaluated separately.
After 12 and 18 months all patients in both groups had improvement from baseline. When the groups were compared, however, the PE group was significantly better at performing transfer activity and had better total HSS score at 12 months. Results from evaluation of the patients at the beginning and at the end of the study are listed in Table 5. All patients in both groups had statistically significant improvement. Mean changes in each parameter during the study are displayed in Figs. 2 and 3.
In the HA group 21 patients with bilateral involvement were excluded from the study (six patients at 12 months and 15 patients at 18 months), because all had received another form of therapy (Table 3). When the mean baseline total HSS score (57.0±12.9) of these patients was compared with the last values (76.7±11.9), there was statistically significant improvement (P=0.0002).
Throughout the study no complications arising from HA injection, for example pain, effusion, synovitis, haemarthrosis, or septic arthritis, were recorded.
Discussion
For symptomatic treatment of OA of the knee, therapeutic options other than NSAID may benefit patients by reducing the morbidity associated with the latter [2]. Although HA preparations have been used to treat OA of the knee for more than 20 years, most experience has been much more recent [2, 6, 9–11, 18]. Review of the literature revealed several clinical trials comparing HA with placebo [4, 7, 8, 12, 15–18], NSAID [6, 19], corticosteroids [13, 14, 20, 21], and mucopolysaccharide polysulfuric acid ester [22]. The benefits of exercise programs for OA of the knee are also well-known [24, 25]. In the study of Petrella and Bartha [30] a simple 8-week home-based exercise program improved pain and functional performance over and above that seen with NSAID treatment alone. Puett and Griffen [31] reviewed 15 controlled trials of non-invasive therapy for OA from 1966 to 1993 and concluded that exercise reduced pain and improved function in patients with OA of the knee. Review of the literature revealed no report comparing results of exercise therapy with those from HA injections, however, so this study seems to be the first.
The results of this study indicate that patients with moderate OA of the knee (Kellgren Lawrence Grade III) benefit either from three injections of HA or 6 weeks of exercise therapy. In both groups the results after 18 months were statistically significantly different from the baseline values (Table 5). Although there were some differences between the groups, especially in the short term (Table 4), long-term results (18 months) showed improvement was almost equal (Figs. 2 and 3).
The drop out rate of the present study is relatively high (42 of 200 knees). Although higher rates have been reported in the literature [2, 12, 21], critical evaluation of these patients resulted in some important conclusions. First, detailed history is mandatory and should be recorded for all controls, especially in trials with long-term follow-up, for such an approach revealed various form of therapy received by the patients (Table 3). Interestingly, all patients excluded from the study were in HA group. Although these patients had statistically very significant improvement from the baseline (P=0.0002), the reason for seeking another form of therapy may be because of the increase in their satisfaction levels. It is well-known that any form of treatment has a placebo effect to some extent. During the study, we observed that the patients in the PE group continued to perform the exercises irregularly; treatment of the HA group, however, was stopped at three weeks. This is probably the reason why about 20% of the HA group sought another form of therapy, even though their scores were equal to those of the PE group.
As far as we know, our study has the longest follow-up of HA patients in the literature (1.5 years). In other series with long term follow-up trials had been ceased after one year [4, 8, 13, 15]. As discussed previously, the exclusion of the patients from our study happened after a year. So we believe clinical trials of HA injections should be with longer follow-up.
In this study, we tried to overcome several problems encountered in HA trials [12, 32]. All our patients had Kellgren Lawrence grade III osteoarthritis with inter-observer agreement, all patients in the HA group received same number of injections, relatively more patients were evaluated and with longer follow-up. However, there are still some weak points of the study. For example our study is not suitable for blind-type evaluation. The drop out rate after one year necessitates larger trials with longer follow-up.
Another unique feature of this study is that almost all of the patients (91%) had bilateral involvement and both knees were included in the study. Except for range of motion, it is not logical to include only one knee of bilateral involvement in measurement of the parameters of the rating systems when evaluating general performance, for example walking distance or climbing stairs, because the uninvolved healthy or diseased knee may affect the results either positively or negatively. This may explain why our results were superior to those of other series.
Although several complications arising from HA injections have been reported [4–9, 12, 13, 19, 22, 33], we observed no complications either minor or major. To optimize efficacy and minimize adverse effects it is essential to bear in mind the importance of full aspiration of any synovial fluid present and of meticulous attention to needle placement [34].
As a result we conclude that hyaluronic acid or progressive knee exercise are effective in alleviating the symptoms of osteoarthritis, postponing total knee replacement for 18 months, and increasing the satisfaction levels of the patients. Additionally bilateral therapy seems more appropriate.
References
Adams M (1999) Viscosupplementation as an alternative to conventional treatment for the management of osteoarthritis of the knee. J Clin Rheum Suppl 5:18–23
Brandt KD, Block JA, Michalski JP et al (2001) Efficacy and safety of intraarticular sodium hyaluronate in knee osteoarthritis. ORTHOVISC Study Group. Clin Orthop 385:130–143
Waddell D, Rein A, Panarites C, Coleman PM, Weiss C (2001) Cost implications of introducing an alternative treatment for patients with osteoarthritis of the knee in a managed care setting. Am J Manag Care 7:981–991
Dougados M, Nguyen M, Listrat V, Amor B (1993) High molecular weight sodium hyaluronate (hyalectin) in osteoarthritis of the knee: a 1 year placebo- controlled trial. Osteoarthritis Cartilage 1:97–103
Namiki O, Toyoshima H, Morisaki N (1982) Therapeutic effect of intra-articular injection of high molecular weight hyaluronic acid on osteoarthritis of the knee. Int J Clin Pharmacol Ther Toxicol 20:501–507
Altman RD, Moskowitz R (1998) Intraarticular sodium hyaluronate (Hyalgan) in the treatment of patients with osteoarthritis of the knee: a randomized clinical trial. Hyalgan Study Group. J Rheumatol 25:2203–2212
Bragantini A, Cassini M, De Bastiani G, Perbellini A (1987) Controlled single-blind trial of intra-articularly injected hyaluronic acid (Hyalgan) in osteo-arthritis of the knee. Clin Trials J 24:333–340
Dixon AS, Jacoby RK, Berry H, Hamilton EB (1988) Clinical trial of intra-articular injection of sodium hyaluronate in patients with osteoarthritis of the knee. Curr Med Res Opin 11:205–213
Evanich JD, Evanich CJ, Wright MB, Rydlewicz JA (2001) Efficacy of intraarticular hyaluronic acid injections in knee osteoarthritis. Clin Orthop 390:173–181
Frizziero L, Govoni E, Bacchini P (1998) Intra-articular hyaluronic acid in the treatment of osteoarthritis of the knee: clinical and morphological study. Clin Exp Rheumatol 16:441–449
Goorman SD, Watanabe TK, Miller EH, Perry C (2000) Functional outcome in knee osteoarthritis after treatment with hylan G-F 20: a prospective study. Arch Phys Med Rehabil 81:479–483
Henderson EB, Smith EC, Pegley F, Blake DR (1994) Intra-articular injections of 750 kD hyaluronan in the treatment of osteoarthritis: a randomised single centre double-blind placebo-controlled trial of 91 patients demonstrating lack of efficacy. Ann Rheum Dis 53:529–534
Leardini G, Franceschini M, Mattara L, Bruno R, Perbellini A (1987) Intra-articular sodiom hyaluronate (Hyalgan) in gonarthrosis. A controlled study comparing methylprednisolone acetate. Clin Trials J 24:341–350
Leardini G, Mattara L, Franceschini M, Perbellini A (1991) Intra-articular treatment of knee osteoarthritis. A comparative study between hyaluronic acid and 6-methyl prednisolone acetate. Clin Exp Rheumatol 9:375–381
Listrat V, Ayral X, Patarnello F, et al (1997) Arthroscopic evaluation of potential structure modifying activity of hyaluronan (Hyalgan) in osteoarthritis of the knee. Osteoarthritis Cartilage 5:153–160
Lohmander LS, Dalen N, Englund G, et al (1996) Intra-articular hyaluronan injections in the treatment of osteoarthritis of the knee: a randomised, double blind, placebo controlled multicentre trial. Hyaluronan Multicentre Trial Group. Ann Rheum Dis 55:424–431
Scale D, Wobig M, Wolpert W (1996) Viscosupplementation of osteoarthritic knees with hylan: a treatment schedule study. Cur Therap Res 55:643–647
Wobig M, Dickhut A, Maier R, Vetter G (1998) Viscosupplementation with hylan G-F 20: a 26-week controlled trial of efficacy and safety in the osteoarthritic knee. Clin Ther 20:410–423
Adams ME, Atkinson MH, Lussier AJ et al (1995) The role of viscosupplementation with hylan G-F 20 (Synvisc) in the treatment of osteoarthritis of the knee: a Canadian multicenter trial comparing hylan G-F 20 alone, hylan G-F 20 with non-steroidal anti-inflammatory drugs (NSAIDs) and NSAIDs alone. Osteoarthritis Cartilage 3:213–225
Grecomoro G, Piccione F, Letizia G (1992) Therapeutic synergism between hyaluronic acid and dexamethasone in the intra-articular treatment of osteoarthritis of the knee: a preliminary open study. Curr Med Res Opin 13:49–55
Jones AC, Pattrick M, Doherty S, Doherty M (1995) Intra-articular hyaluronic acid compared to intra-articular triamcinolone hexacetonide in inflammatory knee osteoarthritis. Osteoarthritis Cartilage 3:269–273
Graf J, Neusel E, Schneider E, Niethard FU (1993) Intra-articular treatment with hyaluronic acid in osteoarthritis of the knee joint: a controlled clinical trial versus mucopolysaccharide polysulfuric acid ester. Clin Exp Rheumatol 11:367–372
Lucangeli A, Gugelmetto M, Primon D (2001) Terapia fisica e acido ialuronico per via intra-articolare nel trattamento della gonartrosi. Riv It Biol Med 21:5–10
Deyle GD, Henderson NE, Matekel RL et al (2000) Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med 132:173–181
Rogind H, Bibow-Nielsen B, Jensen B et al (1998) The effects of a physical training program on patients with osteoarthritis of the knees. Arch Phys Med Rehabil 79:1421–1427
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheumatol Dis 16:494–503
Alicea J (2001) Scoring systems and their validation for the arthritic knee. In: Insall JN, Scott WN (eds) Surgery of the knee. Churchill Livingstone, Philadelphia, pp 1507–1515
Kaplan E, Meier P (1958) Non parametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Puett DW, Griffin MR (1994) Published trials of nonmedicinal and noninvasive therapies for hip and knee osteoarthritis. Ann Intern Med 121:133–140
Petrella RJ, Bartha C (2000) Home based exercise therapy for older patients with knee osteoarthritis: a randomized clinical trial. J Rheumatol 27:2215–2221
Wen DY (2000) Intra-articular hyaluronic acid injections for knee osteoarthritis. Am Fam Physician 62:565–572
Marshall KW (2000) Intra-articular hyaluronan therapy. Curr Opin Rheumatol 12:468–474
Adams ME, Lussier AJ, Peyron JG (2000) A risk-benefit assessment of injections of hyaluronan and its derivatives in the treatment of osteoarthritis of the knee. Drug Saf 23:115–130
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karatosun, V., Unver, B., Gocen, Z. et al. Intra-articular hyaluranic acid compared with progressive knee exercises in osteoarthritis of the knee: a prospective randomized trial with long-term follow-up. Rheumatol Int 26, 277–284 (2006). https://doi.org/10.1007/s00296-005-0592-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-005-0592-z