Abstract
Recent studies have focused on foodborne or commensal bacteria as vehicles of antibiotic resistance. However, the antibiotic resistance of milk bacteria from healthy donors is still vague in Taiwan. For this purpose, human milk samples were obtained from randomly recruited 19 healthy women between 3 and 360 days post-partum. Antibiotic susceptibility profile of bacteria from milk samples was determined. About 20 bacterial species were isolated from milk samples including Staphylococcus (6 species), Streptococcus (4 species), Enterococcus (2 species), Lactobacillus (1 species), and bacteria belonging to other genera (7 species). Some opportunistic or potentially pathogenic bacteria including Kluyvera ascorbata, Klebsiella oxytoca, Klebsiella pneumoniae, Acinetobacter baumannii, Actinomyces bovis, and Staphylococcus aureus were also isolated. Intriguingly, Staphylococcus isolates (22 strains) were resistant to 2–8 of 8 antibiotics, while Streptococcus isolates (3 strains) were resistant to 3–7 of 9 antibiotics, and members of the genus Enterococcus (5 strains) were resistant to 3–8 of 9 antibiotics. Notably, Staphylococcus lugdunensis, S. aureus, Streptococcus parasanguinis, Streptococcus pneumonia, and Enterococcus faecalis were resistant to vancomycin, which is considered as the last-resort antibiotic. Therefore, this study shows that most bacterial strains in human milk demonstrate mild to strong antibiotic resistance. Whether commensal bacteria in milk could serve as vehicles of antibiotic resistance should be further investigated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial antibiotic resistance has been well documented. For instance, an increase in the prevalence of antibiotic-resistant bacteria such as Staphylococcus aureus [6, 16], Acinetobacter baumannii [2, 19, 20], Klebsiella spp., and Enterobacter spp. has been frequently reported [4, 18, 26]. Previously, the selection and dissemination of antibiotic resistance was mainly studied in clinically relevant bacterial species. However, recent studies have suggested that foodborne or commensal bacteria may also function as reservoirs of antibiotic resistance genes, similar to those found in pathogens [8, 14, 25]. For example, human milk has been implicated as a reservoir for several antibiotic-resistant bacteria in that the strains of Staphylococcus epidermidis isolated from human milk (from healthy mothers) have shown resistance to gentamicin, tetracycline, erythromycin, clindamycin, or vancomycin, with several isolates demonstrating multi-drug resistance as well [3]. Moreover, S. epidermidis isolated from human milk of a healthy donor was also reported to exhibit multiple antibiotic resistances [7]. Additionally, Enterococcus spp. isolated from milk of healthy women, as well as that of porcine, canine, ovine, and feline origin, showed resistance to various clinically relevant antibiotics. Notably, two Enterococcus faecalis isolates from human milk displayed resistance to five of eight tested antibiotics, including gentamicin, streptomycin, quinupristin/dalfopristin, tetracycline, and chloramphenicol [11]. Since E. faecalis and E. faecium isolated from milk contained virulence genes and antibiotic resistance, they can serve as a reservoir of antibiotic resistance in infants or offspring [11]. Collectively, these reports indicate that some isolates of Staphylococcus or Enterococcus in milk (from healthy donors) exert resistance to various antibiotics. However, the antibiotic resistance profile of milk bacteria from local area in Taiwan is not clear. Therefore, human milk samples were collected from healthy women, and the bacterial antibiotic susceptibility profile of isolates from milk samples was determined.
Materials and Methods
Milk Samples
This study has been approved by the Institutional Review Board (IRB) at Saint Mary’s Hospital, Lundong (SMHIRB102007), and informed consent was obtained from all individual participants included in the study. Healthy, lactating mothers (n = 19) between 3 and 360 days post-partum who visited the Saint Mary’s Hospital, Lundong, were randomly recruited, and milk samples were collected as previously described [1]. For mothers who delivered by cesarean section, Keflex (cephalexin) had been treated as a prophylactic antibiotic. To collect milk sample, the breast was cleaned using sterile warm water or saline, and the first 0.5 mL of milk was discarded to avoid contamination from the skin. Then, 5–10 mL of milk was collected in sterile tubes by manual expression using sterile gloves. The samples were immediately processed in the laboratory and incubated in different culture media under both anaerobic and aerobic conditions.
Bacterial Isolation
Milk samples were immediately transferred to the laboratory, and the samples were centrifuged briefly at 6000 rpm for 10 min to collect all bacteria. Then, a certain amount of supernatant was discarded, and the centrifuged bacteria were re-suspended in the same milk. Bacteria were isolated by inoculating different culture plates with centrifuged samples. For instance, blood agar plate (BAP)/eosin-methylene blue (EMB) bi-plates and chocolate agar plates were incubated under aerobic conditions at 37 °C for 24 h. For anaerobic species, centrifuged samples were plated onto de Man, Rogosa and Sharpe (MRS), Bacteroides-bile-esculin (BBE), and kanamycin-vancomycin laked blood agar (KVLB) plates and incubated under anaerobic conditions at 37 °C for 48 h in a Bugbox anaerobic workstation (Ruskinn Technology, Ltd., Pencoed, UK; atmospheric composition: 80 % N2, 10 % CO2, and 10 % H2). The obtained bacterial colonies were further purified and examined using phenotypic identification. Pure colonies were identified using both phenotypic and genotypic identification methods as indicated below.
Identification of Bacterial Isolates
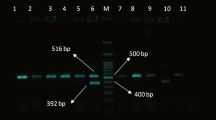
The bacterial isolates were identified by Gram staining and 16S rRNA sequence analysis. Morphological characteristics of the bacterial isolates were examined, followed by phenotypic and genotypic identification methods. Phenotype was characterized using the analytical profile index (API) [15, 17] and the Biolog Microstation system [12, 21]. For genotypic identification, chromosomal DNA of the isolates was extracted and used as a template in polymerase chain reactions (PCR) [23] as previously described, using primer sequences for the 16S rRNA gene [22, 24]. The PCR sequences were confirmed by BLAST searches against the GenBank database at the National Center for Biotechnology Information, USA (http://blast.ncbi.nlm.nih.gov/Blast.cgi).
PCR Amplification
PCR was carried out in a final volume of 50 μL containing 10 mM Tris–HCl (pH 9.0), 50 mM KCl, 1.5 mM MgCl2, 0.2 mM dNTP, 100 ng chromosomal DNA template, 20 pM primer, and 2 U Taq DNA polymerase (Promega, Madison, WI, USA). Thermal cycling was carried out as follows: initial denaturation at 94 °C for 30 s, followed by 30 cycles at 50 °C for 1 min, 72 °C for 1.5 min, and 94 °C for 1.5 min, and a final extension at 72 °C for 5 min in a PerkinElmer GeneAmp 9600 PCR system (Applied Biosystems, Foster City, CA, USA). Finally, the sequences were submitted to GenBank via Sequin software (http://www.ncbi.nlm.nih.gov/Sequin/index.html).
Antimicrobial Susceptibility Testing by Disk Diffusion Assay
Antibiotic susceptibility of isolates was determined using Kirby–Bauer’s disk diffusion method. The results were analyzed and interpreted according to CLSI guidelines using the disk diffusion technique (NCCLS 2012). All antimicrobial disks were purchased from Oxoid Ltd (Oxoid, Basingstoke, UK). Antibiotics, such as oxacillin (1 μg), ampicillin (10 μg), amoxicillin (25 μg), cefazolin (30 μg), cephalothin (30 μg), vancomycin (30 μg), sulfamethoxazole–trimethoprim (25 μg), and ampicillin/sulbactam (20 μg), were selected to test the resistance of Staphylococcus spp. to these antibiotics. Moreover, antibiotics such as ampicillin (10 μg), cefazolin (30 μg), gentamicin (10 μg), erythromycin (15 μg), clindamycin (2 μg), oxacillin (1 μg), ampicillin/sulbactam (20 μg), sulfamethoxazole–trimethoprim (25 μg), and vancomycin (30 μg) were used to test resistance of Enterococcus and Streptococcus spp. Similarly, amikacin (30 μg), ampicillin (10 μg), cefotaxime (30 μg), cefazolin (30 μg), gentamicin (10 μg), ampicillin/sulbactam (20 μg), trimethoprim/sulfamethoxazole (25 μg), ciprofloxacin (5 μg), imipenem (10 μg), and meropenem (10 μg) were used for Kluyvera spp. As for A. baumannii, amikacin (30 μg), ertapenem (10 μg), ceftriaxone (30 μg), ciprofloxacin (5 μg), imipenem (10 μg), meropenem (10 μg), ampicillin/sulbactam (20 μg), cefotaxime (30 μg), ampicillin (10 μg), and cefazolin (30 μg) were used. Otherwise, tetracycline (30 μg), ampicillin (10 μg), amoxicillin (25 μg), chloramphenicol (30 μg), and erythromycin (15 μg) were used for Lactobacillus gasseri.
Moreover, the same assay was routinely conducted using the quality control organisms recommended by NCCLS, including E. coli ATCC 25922, S. aureus ATCC 25923, Pseudomonas aeruginosa ATCC 27853, Haemophilus influenzae ATCC 49766, and Streptococcus pneumoniae ATCC49619, to validate the disk diffusion assay and the effectiveness of antibiotic disks.
Results and Discussion
Distribution of Bacteria in Human Breast Milk
The presence of bacteria in human milk has been acknowledged since the 1970s, with studies focusing on pathogens [10]. In this study, we evaluated the antibiotic susceptibility of bacteria isolated from milk of healthy mothers. In Table 1, approximately four groups of bacterial species were isolated from milk samples, including Staphylococcus (6 species), Streptococcus (4 species), Enterococcus (2 species), Lactobacillus (1 species), and bacteria belonging to other genera (7 species). As described in the paragraph “Identification of Bacterial Isolates,” the bacterial isolates were identified by phenotypic (Gram staining, API, and Biolog Microstation system) and genotypic identification methods (16S rRNA sequence analysis). Staphylococcal and streptococcal cells were the most common, wherein S. epidermidis (in 9 samples) and Staphylococcus lugdunensis (in 6 samples) were frequently isolated (Table 1).
The bacterial species, supplements, and duration of lactation are shown in Table 2. These data indicate that each milk sample had a distinct and heterogeneous bacterial profile. These bacterial strains could be roughly classified into four groups according to their pathogenicity or basic characterizations: commensals (or low-pathogenic), opportunistic pathogens, pathogens, and Lactobacillus species. In summary, commensal bacteria were found in 78 % (15 out of 19) of samples, and opportunistic bacteria were found in 37 % (7 out of 19) of samples. Furthermore, Lactobacillus spp. or potential lactic acid species (such as E. faecalis) were found in 31 % (5) of samples. Thus, most milk-derived isolates were found to be mildly pathogenic or non-pathogenic bacteria, comprising about 94 % of isolates.
Antibiotic Sensitivity Testing for Bacterial Isolates from Human Milk
As indicated in the introduction section, some isolates of Staphylococcus or Enterococcus in milk from healthy donors exert resistance to various antibiotics [3, 7, 11]. In this study, a total of 22 bacterial isolates of Staphylococcus spp. (Table 3) were also evaluated for their susceptibility to several antibiotics. Similar to previous reports, most of these bacteria showed resistance to multiple antibiotics, and these bacteria were found to be resistant to two to eight out of eight antibiotics tested, while two isolates, S. lugdunensis (M3) and S. aureus (M4), were resistant to vancomycin. The resistance rates were also calculated, and a high resistance rate, including intermediate resistance, was observed against oxacillin (82 %) and ampicillin (100 %). Resistance rates of these bacteria to other antibiotics tested were below 17 %.
Antibiotic resistance of Staphylococcus strains from milk samples of healthy donors has been occasionally reported [3, 5]. For instance, the disk diffusion assay found a high rate of antibiotic resistance of S. epidermidis, S. warneri, S. haemolyticus, and S. aureus isolated from milk to penicillin (87 %) and erythromycin (59.3 %) [5]. Notably, two S. haemolyticus isolates from the same study were considered to be intermediately resistant to vancomycin based on the minimum inhibitory concentration assay [5]. That was the first report to indicate that Staphylococcus strains from human milk express reduced susceptibility to vancomycin [5]. More recently, S. epidermidis strains from the milk of healthy mothers have shown resistance to tetracycline, erythromycin, clindamycin, and vancomycin as well [3]. Interestingly, our study is the first to report antibiotic resistance of S. lugdunensis and Sporosarcina pasteurii from milk samples. Collectively, data from previous (from different countries) and the present study indicate that several Staphylococcus spp. isolated from milk from healthy mothers show multiple antibiotic resistances, including that against vancomycin. These data imply that more milk samples from healthy donors should be studied for their antibiotic susceptibility.
Both Enterococcus and Streptococcus spp. show resistance against the selected antibiotics (Table 4). For example, the majority of E. faecalis strains displayed resistance (including intermediate resistance) against three to eight of the nine antibiotics tested, while most Streptococcus-related strains also displayed resistance or intermediate resistance against three to seven out of nine antibiotics tested. Importantly, one Streptococcus parasanguinis strain (M18) was resistant to vancomycin, while another four strains including E. faecalis and S. pneumoniae (samples M2, M5, M12, and M14) also displayed intermediate resistance to vancomycin. The antibiotic resistance rates were also evaluated for these strains. Higher resistance rates for Enterococcus-related strains (total of six strains; Table 3), including intermediate resistance, were observed against cefazolin (66.6 %), gentamicin (83.3 %), erythromycin (100 %), clindamycin (100 %), and oxacillin (100 %). Moreover, all Streptococcus-related strains were resistant to oxacillin and sulfamethoxazole–trimethoprim. In comparison to a previous report, Enterococcus spp. isolated from milk of healthy women, including that of porcine, canine, ovine, and feline origin, have been observed to display resistance against various clinically relevant antibiotics [11]. Of note, two E. faecalis isolates from human milk displayed resistance to five of the eight antibiotics tested, including gentamicin, streptomycin, quinupristin/dalfopristin, tetracycline, and chloramphenicol [11]. Altogether, the present and previous data indicate that Enterococcus or Streptococcus strains isolated from milk show wide-spectrum antibiotic resistance.
Kluyvera and Klebsiella (from M8, M12, or M13) strains were resistant to one to three of 10 antibiotics tested (Table 5). Notably, all strains were resistant to ampicillin. In contrast, A. baumannii (two strains) was resistant to five of 11 antibiotics tested, including ertapenem, ceftriaxone, cefotaxime, ampicillin, and cefazolin. Thus, compared to Kluyvera and Klebsiella, an increased antibiotic resistance was noted for A. baumannii. Conversely, L. gasseri was sensitive to all antibiotics tested and resistant to erythromycin.
Taken together, our data provide evidence that most isolates obtained from the milk of healthy donors showed resistance to various antibiotics. Notably, resistance of bacteria to a given antibiotic can be intrinsic or acquired. However, we did not screen for virulence determinants or antibiotic resistance genes in this study; this will be further evaluated in a subsequent study.
The Role of Commensal Bacteria in Human Milk
The mothers recruited in this study continuously breast-fed their babies for the duration of the study. Although our data show that most bacterial isolates possessed resistance to multiple antibiotics, we believe that these milk-borne bacteria may not pose a risk to the breast-fed infants. Our and previous data only indicate that milk-borne bacteria could be a reservoir or a vehicle for the dissemination of antibiotic resistance [3, 5]. Moreover, the possible threat associated with these bacteria is that they may transfer resistance genes to pathogenic bacteria.
Previous findings have reported the presence of various Lactobacillus or Bifidobacterium species within human milk [9, 10, 13]. Similar to previous studies, one milk sample in our study was colonized with L. gasseri. However, no Bifidobacterium species were isolated from our milk samples. The lack of Bifidobacterium species may be due to the lesser number of milk samples harvested in the present study. Therefore, more milk samples from healthy donors will be studied in our next study. In contrast, the supernatants produced by selected milk isolates, L. gasseri and E. faecalis, exhibited anti-bacterial activity against foodborne pathogens including Escherichia coli HER 1255, Salmonella enterica ATCC 19430, and Staphylococcus aureus ATCC 25923 (data not shown). These data may partially explain the roles of Lactobacillus or potential lactic acid bacteria within human milk.
In conclusion, this study demonstrates that human milk from healthy donors contains various antibiotic-resistant bacteria and that several opportunistic pathogens can colonize the milk as well.
References
Albesharat R, Ehrmann MA, Korakli M, Yazaji S, Vogel RF (2011) Phenotypic and genotypic analyses of lactic acid bacteria in local fermented food, breast milk and faeces of mothers and their babies. Syst Appl Microbiol 34(2):148–155. doi:10.1016/j.syapm.2010.12.001
Antunes LC, Visca P, Towner KJ (2013) Acinetobacter baumannii: evolution of a global pathogen. Pathog Dis. doi:10.1111/2049-632X.12125
Begovic J, Jovcic B, Papic-Obradovic M, Veljovic K, Lukic J, Kojic M, Topisirovic L (2013) Genotypic diversity and virulent factors of Staphylococcus epidermidis isolated from human breast milk. Microbiol Res 168(2):77–83. doi:10.1016/j.micres.2012.09.004
Bouza E, Cercenado E (2002) Klebsiella and enterobacter: antibiotic resistance and treatment implications. Semin Respir Infect 17(3):215–230
Carneiro LA, Queiroz ML, Merquior VL (2004) Antimicrobial-resistance and enterotoxin-encoding genes among staphylococci isolated from expressed human breast milk. J Med Microbiol 53(Pt 8):761–768
Casey JA, Cosgrove SE, Stewart WF, Pollak J, Schwartz BS (2012) A population-based study of the epidemiology and clinical features of methicillin-resistant Staphylococcus aureus infection in Pennsylvania, 2001–2010. Epidemiol Infect 141:1–14
Delgado S, Arroyo R, Jimenez E, Marin ML, del Campo R, Fernandez L, Rodriguez JM (2009) Staphylococcus epidermidis strains isolated from breast milk of women suffering infectious mastitis: potential virulence traits and resistance to antibiotics. BMC Microbiol 9:82. doi:10.1186/1471-2180-9-82
Devirgiliis C, Zinno P, Perozzi G (2013) Update on antibiotic resistance in foodborne Lactobacillus and Lactococcus species. Front Microbiol 4:301. doi:10.3389/fmicb.2013.00301
Heikkila MP, Saris PE (2003) Inhibition of Staphylococcus aureus by the commensal bacteria of human milk. J Appl Microbiol 95(3):471–478
Jeurink PV, van Bergenhenegouwen J, Jimenez E, Knippels LM, Fernandez L, Garssen J, Knol J, Rodriguez JM, Martin R (2013) Human milk: a source of more life than we imagine. Benef Microbes 4(1):17–30. doi:10.3920/BM2012.0040
Jimenez E, Ladero V, Chico I, Maldonado-Barragan A, Lopez M, Martin V, Fernandez L, Fernandez M, Alvarez MA, Torres C, Rodriguez JM (2013) Antibiotic resistance, virulence determinants and production of biogenic amines among enterococci from ovine, feline, canine, porcine and human milk. BMC Microbiol 13:288. doi:10.1186/1471-2180-13-288
Klingler JM, Stowe RP, Obenhuber DC, Groves TO, Mishra SK, Pierson DL (1992) Evaluation of the Biolog automated microbial identification system. Appl Environ Microbiol 58(6):2089–2092
Martin R, Langa S, Reviriego C, Jiminez E, Marin ML, Xaus J, Fernandez L, Rodriguez JM (2003) Human milk is a source of lactic acid bacteria for the infant gut. J Pediatr 143(6):754–758. doi:10.1016/j.jpeds.2003.09.028
Mathur S, Singh R (2005) Antibiotic resistance in food lactic acid bacteria: a review. Int J Food Microbiol 105(3):281–295. doi:10.1016/j.ijfoodmicro.2005.03.008
O’Hara CM, Rhoden DL, Miller JM (1992) Reevaluation of the API 20E identification system versus conventional biochemicals for identification of members of the family Enterobacteriaceae: a new look at an old product. J Clin Microbiol 30(1):123–125
Onanuga A, Awhowho GO (2012) Antimicrobial resistance of Staphylococcus aureus strains from patients with urinary tract infections in Yenagoa, Nigeria. J Pharm Bioallied Sci 4(3):226–230. doi:10.4103/0975-7406.99058
Overman TL, Plumley D, Overman SB, Goodman NL (1985) Comparison of the API rapid E four-hour system with the API 20E overnight system for the identification of routine clinical isolates of the family Enterobacteriaceae. J Clin Microbiol 21(4):542–545
Paterson DL (2006) Resistance in gram-negative bacteria: enterobacteriaceae. Am J Med 119(6 Suppl 1):S20–S28. doi:10.1016/j.amjmed.2006.03.013 (discussion S62–70)
Peleg AY, Seifert H, Paterson DL (2008) Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev 21(3):538–582. doi:10.1128/CMR.00058-07
Rit K, Saha R (2012) Multidrug-resistant acinetobacter infection and their susceptibility patterns in a tertiary care hospital. Niger Med J 53(3):126–128. doi:10.4103/0300-1652.104379
Stager CE, Davis JR (1992) Automated systems for identification of microorganisms. Clin Microbiol Rev 5(3):302–327
Temmerman R, Huys G, Swings J (2004) Identification of lactic acid bacteria: culture-dependent and culture-independent methods. Trends Food Sci Technol 15:348–359
Wang CM, Shyu CL, Ho SP, Chiou SH (2008) Characterization of a novel thermophilic, cellulose-degrading bacterium Paenibacillus sp. strain B39. Lett Appl Microbiol 47(1):46–53. doi:10.1111/j.1472-765X.2008.02385.x
Wang CM, Shyu CL, Ho SP, Chiou SH (2007) Species diversity and substrate utilization patterns of thermophilic bacterial communities in hot aerobic poultry and cattle manure composts. Microb Ecol 54(1):1–9. doi:10.1007/s00248-006-9139-4
White DG, Zhao S, Simjee S, Wagner DD, McDermott PF (2002) Antimicrobial resistance of foodborne pathogens. Microbes Infect 4(4):405–412
Yu WL, Chuang YC, Walther-Rasmussen J (2006) Extended-spectrum beta-lactamases in Taiwan: epidemiology, detection, treatment and infection control. J Microbiol Immunol Infect 39(4):264–277
Acknowledgments
This work was supported by grants from St. Mary’s Junior College of Medicine, Nursing and Management, and St. Mary’s Hospital, Luodong (SMC104-I-01, SMHRH-102003, and SMHRF-103001), and partially supported by a Grant from the Ministry of Science and Technology (MOST 103-2320-B-562 -001-MY3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Chen, PW., Tseng, SY. & Huang, MS. Antibiotic Susceptibility of Commensal Bacteria from Human Milk. Curr Microbiol 72, 113–119 (2016). https://doi.org/10.1007/s00284-015-0925-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-015-0925-4