Abstract
Purpose
Paclitaxel injection concentrate for nano-dispersion (PICN) is a Cremophor-free, nanotechnology-driven paclitaxel formulation. This phase I study examined the safety, tolerability, pharmacokinetics and maximum tolerated dose (MTD) of PICN alone and in combination with carboplatin. Its early efficacy in unresectable biliary tract cancers (BTCs) was also evaluated.
Methods
This multi-center study comprised two parts. Part A contained a dose-escalation cohort following “3 + 3” design using PICN monotherapy in advanced solid tumors (Part A1); Part A2 dose-expansion cohort was then conducted in advanced BTCs due to observed efficacy in Part A1. Part B1 and B2 evaluated escalating dose of PICN with carboplatin in advanced solid tumors. PICN was administered as a 30 min-infusion every 3 weeks without pre-medications for hypersensitivity reactions.
Results
Thirty-six patients received PICN monotherapy in Part A and 21 received PICN plus carboplatin in Part B. The MTD of PICN was determined to be 295 mg/m2 both as a monotherapy and in combination with carboplatin at AUC 5. Dose-proportional exposure in paclitaxel Cmax and AUC was observed overdose range from 175 to 325 mg/m2 for PICN monotherapy and its combination with carboplatin. Carboplatin did not alter PICN exposure. Clinically significant toxicities mainly include neutropenia and peripheral neuropathy. PICN monotherapy yielded a response rate of 20% in unresectable BTCs.
Conclusion
This study demonstrated the safety and stable pharmacokinetics of PICN as a monotherapy and in combination with carboplatin. Single-agent PICN showed promising antitumor activity in advanced BTCs, warranting further studies to investigate its role in gastrointestinal cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paclitaxel is a chemotherapeutic agent with antitumor activity across a broad spectrum of tumors either as a monotherapy or in combination with other anti-cancer therapies [1, 2]. Mechanistically, paclitaxel promotes microtubule polymerization and induces mitotic arrest in cancer cells [3]. The development of paclitaxel as a therapeutic agent has been challenging due to its complex synthesis and aqueous insolubility [4]. Paclitaxel was initially formulated in the nonionic surfactant Cremophor EL (polyoxyethylated castor oil) and ethanol (Cre-paclitaxel) to enhance its solubility and permit its clinical applications. Use of Cremophor negatively impacts the efficacy and toxicity profile of paclitaxel and requires pre-medications with steroid and anti-histamines to mitigate the risks of Cremophor related infusion reactions, which are known to contribute to treatment-related morbidity and early discontinuation of therapies [5]. By eliminating the toxic organic base, solvent-free formulations have the potential to permit the delivery of a higher dose of paclitaxel to achieve better antitumor activity with an acceptable safety profile [6].
Paclitaxel injection concentrate for nano-dispersion (PICN)♣ is a novel, Cremophor-free paclitaxel formulation developed by Sun Pharma Advanced Research Company (SPARC Ltd.). It is a composite of self-assembled nano-particles of paclitaxel stabilized with polymer and lipid mixture and is given via intravenous administration [7, 8]. It does not leach plasticizers from infusion bags or tubings, permitting the use of conventional PVC infusion systems without in-line filtration. Its preparation does not need wait times and complex procedures such as lyophilized cake wetting or settling time. PICN due to synthetic chemical composition does not carry the potential risk for transmission of blood-borne illness. The net cumulative effect is decreased administrative burden on the hospital staff and reduced hospital stay for the patients [8]. Currently, PICN has been used as the non-proprietary name for the drug product under clinical development.
PICN dosage is determined by the paclitaxel content of this formulation, making a direct comparison with other commercially available formulations possible. The PICN formulation (PICN at 260 and 295 mg/m2 every 3 weeks, intravenous administration) was previously evaluated clinically in patients with metastatic breast cancer in India [7, 8]. The primary objective of this study (NCT01304303) was to evaluate the clinical safety and efficacy of PICN as a monotherapy and in combination with carboplatin in the treatment of advanced solid tumors in the North America population. PICN monotherapy was evaluated further in 20 patients with biliary tract cancers (BTCs) (dose expansion of Part A) after antitumor activity was observed in BTCs during dose escalation.
Material and methods
Study design and patient eligibility
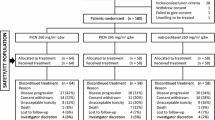
This study was reviewed and approved by the Institutional Review Boards of the respective centers, and written informed consent was mandatory. It was designed to determine the maximum tolerated dose (MTD) and toxicity profile of PICN alone (Part A: A1 and A2) and in combination with carboplatin (Part B: B1 and B2). The study began with dose escalation of PICN monotherapy (Part A1) and was expanded to enroll additional 20 patients with BTCs at the MTD (Part A2) when antitumor activity in BTCs was observed in Part A1. Upon determination of the MTD of PICN monotherapy in Part A, the study proceeded to determine the MTD of PICN in combination with carboplatin at AUC 6 (Part B1) and later at AUC 5 (Part B2) due to toxicity observed in B1.
Patients were eligible for the study if they were 18 years old and above, with histologically or cytologically confirmed diagnosis of advanced-stage solid tumors for which rational treatment options include taxane-based therapy in Part A1, and platinum plus taxane-based therapy in Part B. To be eligible for the A2 expansion cohort, patients were to have histologically or cytologically confirmed biliary tract carcinoma. Other inclusion criteria included Eastern Cooperative Oncology Group (ECOG) performance status 0–1, estimated life expectancy ≥ 12 weeks, measurable disease per the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, adequate bone marrow [absolute neutrophil count (ANC) ≥ 1.5 × 109/L, hemoglobin ≥ 9.0 g/dL, and platelet count ≥ 100 × 109/L], liver [total bilirubin ≤ 1.5 mg/dL (or ≤ 2 mg/dL for liver metastases), aspartate transaminase (AST) ≤ 2.5 × upper limit of normal (ULN; or ≤ 5 × ULN for liver metastases), alanine transaminase (ALT) ≤ 2.5 × ULN (or ≤ 5 × ULN for liver metastases), and alkaline phosphatase (ALP) ≤ 5 × ULN)], and renal functions [creatinine ≤ 2.0 mg/dL in Part A and ≤ 1.5 × ULN or creatinine clearance (CrCl) > 50 mL/min in Part B] within 2 weeks of initiation of treatment. Patients must have completed radiotherapy, chemotherapy and/or major surgery ≥ 4 weeks prior to study enrollment without residual toxicity with the exception of alopecia. Patients were excluded if they had known hypersensitivity to the study drug, active central nervous system metastases, pre-existing clinically significant peripheral neuropathy [grade ≥ 2 per Common Terminology Criteria of Adverse Events (CTCAE) version 4.0], severe concurrent disease per investigator assessment, and clinically significant pleural and/or ascitic fluid.
Dose escalation, dose-limiting toxicity (DLT), and maximum tolerated dose (MTD)
Adverse events were graded according to the National Cancer CTCAE version 4.0. DLT was defined as the occurrence of any of the following: grade 4 neutropenia for more than 7 days or febrile neutropenia requiring parenteral antibiotics, grade 3 thrombocytopenia for more than 7 days or requiring platelet transfusion, grade ≥ 2 hemorrhage, grade ≥ 3 non-hematologic PICN-related toxicities excluding alopecia, nausea, vomiting, nail disorders and diarrhea despite optimal medical management, or treatment delay for more than 7 days during the first cycle (Cycle 1) of treatment with PICN monotherapy or its combination with carboplatin. Adverse events attributed to carboplatin alone were not considered DLTs.
In Part A1, B1 and B2, patients were sequentially enrolled in a “3 + 3” dose-escalation scheme (Table 1). Three patients were treated at each dose level for 21-day cycles. If no DLT was observed with the starting dose, three patients would be treated at the next higher dose level. If one of three patients experienced a DLT at any dose level, three additional patients would be treated at this dose. If DLTs occurred in ≥ two patients at any dose level, dose escalation would be halted and three additional patients would be treated at the preceding lower dose level. MTD was defined as the dose level below the lowest dose that induced DLT in at least one-third of patients (of ≥ two of six patients) in Cycle 1 treatment. At least six patients would be treated at the MTD. Does escalation was not allowed in individual patients.
In the A1 dose escalation cohort, PICN monotherapy started at 175 and progressed to 260, 295 and 325 mg/m2. Part A2 was conducted to determine the tolerability of the MTD determined in Part A1 and, furthermore, in BTC patients due to observed antitumor activity in Part A1. All patients in Part A2 received the same starting dose. In Part B, PICN dose escalation started at 220 and proceeded to 260 mg/m2 in combination with carboplatin at AUC 6 (Part B1) but the 260 mg/m2 dose level was determined intolerable. The protocol was then amended to explore a lower carboplatin dose (AUC 5) and PICN dose escalation re-started at 260 and proceeded to 295 and 325 mg/m2 (Part B2).
Treatment plan
PICN and carboplatin were supplied by Sun Pharma Advanced Research Co. Ltd., India. PICN was provided in single-use vials of liquid pre-concentrate to be diluted in 5% dextrose solution to obtain nano-dispersion for intravenous infusion. This was infused using conventional PVC infusion system without in-line filter. Carboplatin was provided as a sterile aqueous solution to be diluted per local institute standards prior to infusion. The maximum carboplatin dose used in the study was 900 mg per cycle for AUC 6 and 750 mg for AUC 5, using maximum CrCl 125 mL/min. In Part A, PICN was administered intravenously over 30 min every 3 weeks as a monotherapy. In Part B, PICN was administered intravenously over 30 min followed by carboplatin, which was administered intravenously over 30 min with an interval up to 3 h, on Day 1 of every 3-week cycle. Prophylactic anti-emetics including 5-HT3 antagonists were administered per local institutional standard. Prophylactic medications against hypersensitivity reactions were not required. Treatment was continued until patients developed unacceptable adverse events, had disease progression, withdrew consent, did not comply with treatment, or developed inter-current illness which prevented further treatment.
Study assessments
Following written, informed consent, patients underwent baseline assessments including a complete history and physical examination, evaluation of ECOG performance status, electrocardiograph, chest X-ray, radiographic staging of disease by either CT or MRI, complete blood count, serum chemistries, liver function test, coagulation profile, and urine pregnancy test if applicable. Interval examination, complete blood count, serum chemistries and liver function test were repeated weekly. Radiographic assessment was performed every two cycles based on RECIST version 1.1. Patients were followed for at least 3 weeks after study completion or discontinuation.
Pharmacokinetic (PK) studies
Plasma samples for PK evaluation were collected at pre-dose, 1, 2, 3, 4, 5, 6, 24, and 48 h following PICN infusion on the first day of Cycle 1 treatment. Blood samples were collected from a site other than the infusion site with a vacutainer containing ethylenediaminetetraacetic acid (EDTA). Plasma was separated within 1 h of collection by centrifugation at room temperature at 3000 rpm for 10 min and stored at or below − 20 °C within 1 h of separation. The plasma concentration of paclitaxel was measured using validated liquid chromatography-mass spectroscopy with solid-phase extraction over a concentration range of 0.005–25 μg/mL for paclitaxel [9].
Statistical analysis
As a phase I, dose-escalation and expansion study, analyses were descriptive and exploratory. Patients receiving at least one dose of study drug were included in safety analyses and those who completed at least one post-baseline efficacy assessment were evaluable for tumor response. Best overall response was the best response recorded from the start of the treatment until disease progression/recurrence or withdrawal from the study for any other reason. Patient characteristics, adverse events, and tumor response were summarized by descriptive statistics. Progression-free survival (PFS) was analyzed using the Kaplan–Meier method. PK parameters were analyzed using Phoenix® Win-Nonlin® (version 6.4) non-compartmental analyses. Statistical analyses were performed on individual PK parameters using the SAS® package (SAS® Institute Inc., USA, version 9.3).
Results
Patient characteristics
A total of 64 patients with advanced solid tumors were screened between October 2011 and December 2015 for this study; 57 of these patients were enrolled. Thirty-six patients were treated with PICN alone in Part A (A1 and A2) and 21 patients were treated with PICN plus carboplatin in Part B (B1 and B2). Nine patients received carboplatin at AUC 6 (B1) and 12 received carboplatin at AUC 5 (B2). Demographic and clinical characteristics of enrolled patients are summarized in Table 2. Most of the patients enrolled in the study had received ≥ one prior chemotherapy for their disease and had ≥ one metastatic site. Overall, 62.5 and 54.4% of patients had received ≥ two prior chemotherapies in Part A and B, respectively.
Dose-escalation and MTD
In Part A1 dose-escalation portion, cohorts of three patients were treated with PICN monotherapy successively from 175 to 295 mg/m2 with no DLTs. Four patients were treated at 325 mg/m2 and two events of grade ≥ 3 non-hematologic toxicity leading to dose-limiting toxicity (DLT) were reported. The two DLTs were pneumonia and sepsis. Therefore, a second cohort of three patients was treated at the preceding lower dose of 295 mg/m2 and no DLTs were observed. As a result, 295 mg/m2 was established as the MTD for PICN monotherapy. In Part A2 expansion cohort, all 20 patients with BTCs were treated at the MTD of 295 mg/m2. Overall PICN at the dose of 295 mg/m2 was well tolerated with one event of dose-limiting grade 4 neutropenia and one event of dose-limiting grade ≥ three non-hematologic toxicity reported.
In Part B1, three patients received the starting dose of PICN at 220 mg/m2 plus carboplatin at AUC 6 without DLTs. At the next higher dose level of PICN 260 mg/m2 plus carboplatin, two of three patients experienced dose-limiting thrombocytopenia and dose delay of ≥ 7 days for thrombocytopenia. This study was then amended to reduce the carboplatin dose to AUC 5 and dose escalation resumed with PICN at 260 mg/m2 with a fixed dose of carboplatin at AUC 5 in Part B2. Three patients were treated at this level and no DLTs were observed. Subsequently, in combination with carboplatin at AUC 5, one of six patients experienced DLT (grade 3 febrile neutropenia) at PICN 295 mg/m2 and two of three patients experienced DLTs (grade 3 sepsis with underlying neutropenia and grade 3 febrile neutropenia) at PICN 325 mg/m2. Thus, PICN295 mg/m2 was determined to be the MTD for PICN in a combination of carboplatin at AUC 5.
Treatment-related adverse events
In Part A1, safety was evaluated in 16 patients (Table 3) and the most common, treatment-related grade ≥ 2 adverse events were peripheral sensory neuropathy (31.25%), alopecia (31.25%), neutropenia (25%) and fatigue (25%). Five patients (31.25%) experienced grade ≥ 3 adverse events, of which two patients received PICN at 325 mg/m2 that is above the MTD. The most common grade ≥ 3 adverse event was neutropenia (18.75%). Other grade 3 adverse events included thrombocytopenia, leukopenia, peripheral sensory neuropathy, muscular weakness, pneumonia and fatigue. Five patients (31.3%) discontinued the study due to adverse events of which three patients received the dose of 325 mg/m2. In Part A2, safety was evaluated in 20 patients with heavily treated BTCs at MTD of 295 mg/m2. The most common grade ≥ 3 adverse events were neutropenia (20%) and peripheral sensory neuropathy (20%). Three patients (15%) discontinued the study due to adverse events and one patient died because of disease progression.
In Part B, safety was evaluated in 21 patients (Table 4). The most common, treatment-related grade ≥ 2 adverse events were neutropenia (76.2%), thrombocytopenia (47.6%), fatigue (47.6%), anemia (42.8%) and peripheral sensory neuropathy (38.1%). Grade ≥ 3 adverse events included anemia, neutropenia, febrile neutropenia, thrombocytopenia, fatigue, peripheral sensory neuropathy, muscular weakness, dehydration, and arthralgia. Six patients (28.5%) discontinued the study due to adverse events.
Clinical efficacy
Thirty-three patients in Part A and 18 patients in Part B were evaluable for treatment response as follow-up imaging studies were not performed in six patients. In the Part A1 dose-escalation cohort with PICN monotherapy, four patients had partial response (PR) at doses ≥ 260 mg/m2. Two of these patients had advanced, refractory BTCs and they received 31 cycles and 17 cycles of treatment, respectively. Neither had received paclitaxel previously. These promising results prompted the Part A2 dose-expansion study in BTCs. The other two patients who attained PR had metastatic breast cancer and metastatic squamous cell carcinoma of the tongue refractory to two prior lines of chemotherapy. Both patients had previously received paclitaxel; one in the adjuvant setting and the other in the neoadjuvant setting. The patient with metastatic squamous cell carcinoma received 15 cycles of treatment.
In the Part A2 BTC expansion cohort, 4 (20%) patients had PR and 8 (40%) maintained stable disease (SD) at PICN dose of 295 mg/m2. Patients with PR received a median of 9 (range, 5–11) cycles of treatment. All four patients had not received paclitaxel previously. Overall, 20 patients received a mean of 4.15 cycles of treatment with a median PFS of 3.4 (95% confidence interval: 1.3–5.9) months (Fig. 1).
In Part B2, six patients were treated with PICN at 295 mg/m2 plus carboplatin at AUC 5 and three of them achieved PR. These three patients had squamous cell carcinoma (tonsil, esophagus and bladder, respectively) and two were refractory to ≥ 2 prior chemotherapy regimens including taxanes. Overall, these six patients received a median of eight cycles of PICN at MTD and achieved a median PFS of 8.2 (95% confidence interval: 4.1–9.8) months. Of three patients who received PICN dose of 260 mg/m2, one had PR while two had SD. At 325 mg/m2, two patients had SD and one patient withdrew from study prior to post-baseline assessment.
PK analysis
Forty-two patients contributed to PK analysis including 37 from dose-escalation cohorts (Part A1, B1 and B2) and 5 from the dose-expansion cohort (Part A2). PK parameters after a single dose of PICN in Cycle 1 derived by non-compartmental methods are presented in Tables 5, 6 and Fig. 2. The Cmax occurred towards the end of 30-min infusion. The slopes of dose-normalized Cmax and AUC vs. dose did not differ significantly from zero (P > 0.05) which demonstrates that Cmax and AUC increased linearly and in a proportional manner to the dose of PICN across all dose levels in Part A1 (175–325 mg/m2), B1 and B2 (220–325 mg/m2). The PK parameters did not differ significantly between the dose-escalation cohorts and the dose-expansion cohorts (Part A2). The paclitaxel exposure achieved at the evaluated PICN doses was comparable to published data on other formulations of paclitaxel [10].
Discussion
This study examined the safety, pharmacokinetics and preliminary efficacy of PICN, a novel Cremophor-free nanotechnology driven paclitaxel preparation as a monotherapy and in combination with carboplatin. Conventional solvent-containing formulations aggravate clinical toxicities associated with paclitaxel use including hypersensitivity reactions. Novel nanotechnology-driven formulations such as Abraxane® and PICN aim at improving the safety profile of paclitaxel, enabling delivery of higher doses to enhance its efficacy [11].
The MTD of PICN monotherapy was established at 295 mg/m2 every 3 weeks in this study. Clinically significant adverse effects observed with PICN monotherapy across all dose levels tested (175–325 mg/m2) were peripheral sensory neuropathy and neutropenia; 13.9 and 19.4% of patients had grade ≥ 3 peripheral sensory neuropathy and neutropenia, respectively. At the MTD of 295 mg/m2 every 3-week, 15.4 and 3.8% of patients had grade 3 peripheral sensory and motor neuropathy, respectively, and 19.2% of patients had grade 3–4 febrile neutropenia. This compared favorably to Cre-paclitaxel at 175 mg/m2 every 3-week (FDA-approved dosing schedule), which causes peripheral neuropathy in 42–70% of patients (≤ 7% with grade 3–4 toxicity) and neutropenia in 78–98% patients (14–75% with grade 4 toxicity) [12]. The incidence of grade 4 neutropenia was also comparable between albumin-bound paclitaxel (Abraxane®) at 260 mg/m2 every 3-week and PICN at 295 mg/m2 every 3-week (9 and 7.7% of patients had grade 4 neutropenia, respectively) [13]. These toxicities are known with the use of paclitaxel. Ocular or vision disturbances were not reported in patients who received PICN at doses evaluated.
When combined with carboplatin, increased incidence of myelosupression was observed. Most of the adverse events in the study were indicative of the nature of the patient population or expected from the study drug. Compared to platinum-containing regimens with Cre-paclitaxel, the extent and incidence of myelosuppression and peripheral neuropathy were limited with the use of PICN formulation which enabled the delivery of a higher dose of paclitaxel [14,15,16,17,18,19,20]. None of the enrolled patients experienced hypersensitivity reactions. Pre-medication with steroid was not required for PICN monotherapy and only 5.5% of patients (two out of 36 in Part A) required anti-emetics.
The PK analysis of PICN demonstrated a dose linear and proportional increase in Cmax and AUC0-inf across all paclitaxel dose levels. Dose linear behaviour of PICN contrasts with the non-linear pharmacokinetics associated with Cre-paclitaxel formulation and is similar to Abraxane®. PICN at 260 and 295 mg/m2 demonstrated Cmax (16.54 and 12.01 μg/mL) and AUC0-inf (18.72 and 20.40 μg*h/mL) similar to that observed with Abraxane® 260 mg/m2 as a 30-min infusion (Cmax 19.5 μg/mL and AUC0-inf 20.3 μg*h/mL). Cre-paclitaxel administered at 175 mg/m2 as a 3-h infusion attains Cmax of 3.6 μg/mL and AUC0-inf 15.0 μg*h/mL [8]. The significant increase in the paclitaxel exposure from PICN could contribute to improved antitumor efficacy compared with solvent-based paclitaxel. PICN in combination with carboplatin also demonstrated dose-proportional pharmacokinetics. Carboplatin did not impact the pharmacokinetics of PICN in the study. The pharmacokinetics between Indian and North American population was similar and MTD was established at 295 mg/m2 for both populations.
This study also showed promising antitumor activity of PICN monotherapy in patients with advanced BTCs. As the standard of care, gemcitabine plus cisplatin is the first-line therapy for metastatic BTCs based on two landmark studies [21, 22], which reported a median overall survival of about 11 months and a response rate of 19.5%. There is insufficient data to recommend a specific chemotherapy in the second-line setting [23]. In the A2 expansion cohort, 20 patients with gallbladder carcinoma, intra-hepatic and extra-hepatic cholangiocarcinoma received PICN monotherapy at 295 mg/m2 every 3 weeks. Fourteen patients received it as a second-line agent and five patients as third line and beyond. Overall, PICN monotherapy yielded an overall response rate of 20% and a median PFS of 3.4 months in unresectable BTC patients. Its role as a combination regimen is currently under investigation (SWOG S1815).
In conclusion, this phase I study established the MTD of PICN as a monotherapy and in combination with carboplatin. With its well-tolerated safety profile, PICN demonstrated encouraging single-agent activity in BTCs with response rates comparable to the standard first-line combination therapy for this disease. The role of paclitaxel in BTCs should be explored further either as a single agent or part of a combination therapy. This study demonstrated that nano-dispersion technology could deliver higher paclitaxel dose with good tolerance in North American patient population and offers an alternative Cremophor-free paclitaxel formulation.
Data availability
The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
References
Rowinsky EK (1997) The development and clinical utility of the taxane class of antimicrotubule chemotherapy agents. Annu Rev Med 48:353–374. https://doi.org/10.1146/annurev.med.48.1.353
Crown J, O’Leary M (2000) The taxanes: an update. Lancet 355(9210):1176–1178. https://doi.org/10.1016/s0140-6736(00)02074-2
Schiff PB, Fant J, Horwitz SB (1979) Promotion of microtubule assembly in vitro by taxol. Nature 277(5698):665–667
Weaver BA (2014) How taxol/paclitaxel kills cancer cells. Mol Biol Cell 25(18):2677–2681. https://doi.org/10.1091/mbc.E14-04-0916
Hennenfent KL, Govindan R (2006) Novel formulations of taxanes: a review Old wine in a new bottle? Ann Oncol 17(5):735–749. https://doi.org/10.1093/annonc/mdj100
Ma WW, Hidalgo M (2013) The winning formulation: the development of paclitaxel in pancreatic cancer. Clin Cancer Res 19(20):5572–5579. https://doi.org/10.1158/1078-0432.ccr-13-1356
Jain MM, Gupte SU, Patil SG, Pathak AB, Deshmukh CD, Bhatt N, Haritha C, Govind Babu K, Bondarde SA, Digumarti R, Bajpai J, Kumar R, Bakshi AV, Bhattacharya GS, Patil P, Subramanian S, Vaid AK, Desai CJ, Khopade A, Chimote G, Bapsy PP, Bhowmik S (2016) Paclitaxel injection concentrate for nanodispersion versus nab-paclitaxel in women with metastatic breast cancer: a multicenter, randomized, comparative phase II/III study. Breast Cancer Res Treat 156(1):125–134. https://doi.org/10.1007/s10549-016-3736-9
Taclantis® (PICS) (2020). https://www.sparc.life/research-programs/taclantis-picn. Accessed 16 Nov 2020
Gardner ER, Dahut W, Figg WD (2008) Quantitative determination of total and unbound paclitaxel in human plasma following Abraxane treatment. J Chromatogr B Analyt Technol Biomed Life Sci 862(1–2):213–218
Gardner ER, Dahut WL, Scripture CD, Jones J, Aragon-Ching JB, Desai N, Hawkins MJ, Sparreboom A, Figg WD (2008) Randomized crossover pharmacokinetic study of solvent-based paclitaxel and nab-paclitaxel. Clin Cancer Res 14(13):4200–4205. https://doi.org/10.1158/1078-0432.ccr-07-4592
Foote M (2007) Using nanotechnology to improve the characteristics of antineoplastic drugs: improved characteristics of nab-paclitaxel compared with solvent-based paclitaxel. Biotechnol Annu Rev 13:345–357. https://doi.org/10.1016/s1387-2656(07)13012-x
Lexicomp, Inc. Paclitaxel (conventional): drug information. In: UpToDate, UpToDate, Waltham, MA. https://www.uptodate.com/contents/paclitaxel-conventional-drug-information/print?search=paclitaxel-conventional-drug-&source. Accessed 16 Feb 2021
Hecht JR, Trarbach T, Hainsworth JD, Major P, Jäger E, Wolff RA, Lloyd-Salvant K, Bodoky G, Pendergrass K, Berg W, Chen B-L, Jalava T, Meinhardt G, Laurent D, Lebwohl D, Kerr D (2011) Randomized, placebo-controlled, phase III study of first-line oxaliplatin-based chemotherapy plus PTK787/ZK 222584, an oral vascular endothelial growth factor receptor inhibitor, in patients with metastatic colorectal adenocarcinoma. J Clin Oncol 29(15):1997–2003. https://doi.org/10.1200/jco.2010.29.4496
Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S, Copeland LJ, Walker JL, Burger RA (2006) Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med 354(1):34–43. https://doi.org/10.1056/NEJMoa052985
Bermejo C, Busby JE, Spiess PE, Heller L, Pagliaro LC, Pettaway CA (2007) Neoadjuvant chemotherapy followed by aggressive surgical consolidation for metastatic penile squamous cell carcinoma. J Urol 177(4):1335–1338. https://doi.org/10.1016/j.juro.2006.11.038
Perez EA, Hillman DW, Stella PJ, Krook JE, Hartmann LC, Fitch TR, Hatfield AK, Mailliard JA, Nair S, Kardinal CG, Ingle JN (2000) A phase II study of paclitaxel plus carboplatin as first-line chemotherapy for women with metastatic breast carcinoma. Cancer 88(1):124–131
Stathopoulos GP, Rigatos S, Papakostas P, Fountzilas G (1997) Effectiveness of paclitaxel and carboplatin combination in heavily pretreated patients with head and neck cancers. Eur J Cancer 33(11):1780–1783
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, Richel DJ, Nieuwenhuijzen GA, Hospers GA, Bonenkamp JJ, Cuesta MA, Blaisse RJ, Busch OR, ten Kate FJ, Creemers GJ, Punt CJ, Plukker JT, Verheul HM, Spillenaar Bilgen EJ, van Dekken H, van der Sangen MJ, Rozema T, Biermann K, Beukema JC, Piet AH, van Rij CM, Reinders JG, Tilanus HW, van der Gaast A (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366(22):2074–2084. https://doi.org/10.1056/NEJMoa1112088
Vaughn DJ, Malkowicz SB, Zoltick B, Mick R, Ramchandani P, Holroyde C, Armstead B, Fox K, Wein A (1998) Paclitaxel plus carboplatin in advanced carcinoma of the urothelium: an active and tolerable outpatient regimen. J Clin Oncol 16(1):255–260. https://doi.org/10.1200/jco.1998.16.1.255
Von Hoff DD, Ramanathan RK, Borad MJ, Laheru DA, Smith LS, Wood TE, Korn RL, Desai N, Trieu V, Iglesias JL, Zhang H, Soon-Shiong P, Shi T, Rajeshkumar NV, Maitra A, Hidalgo M (2011) Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J Clin Oncol 29(34):4548–4554. https://doi.org/10.1200/jco.2011.36.5742
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira SP, Roughton M, Bridgewater J (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 362(14):1273–1281. https://doi.org/10.1056/NEJMoa0908721
Okusaka T, Nakachi K, Fukutomi A, Mizuno N, Ohkawa S, Funakoshi A, Nagino M, Kondo S, Nagaoka S, Funai J, Koshiji M, Nambu Y, Furuse J, Miyazaki M, Nimura Y (2010) Gemcitabine alone or in combination with cisplatin in patients with biliary tract cancer: a comparative multicentre study in Japan. Br J Cancer 103(4):469–474. https://doi.org/10.1038/sj.bjc.6605779
Lamarca A, Hubner RA, David Ryder W, Valle JW (2014) Second-line chemotherapy in advanced biliary cancer: a systematic review. Ann Oncol 25(12):2328–2338. https://doi.org/10.1093/annonc/mdu162
Acknowledgements
We thank the patients, their families and all investigators who participated in this clinical trial. We also thank Pradeep Shahi from the Pharmacokinetics Department, Sun Pharmaceutical Industries Ltd for proof-reading the manuscript.
Funding
This study was supported by Sun Pharma Advanced Research Co. Ltd. Medical editorial assistance was also provided by Sun Pharma Advanced Research Co. Ltd.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
EL, JD and AJ declare no conflict of interest specifically related to this project. Their respective institutions received research support to conduct this study from the sponsor.
Ethical approval
This study was approved by the institutional review board of respective institutions and was performed in line with the principles of the Declaration of Helsinki.
Consent to participate
Written informed consent to participate in the study was obtained from all participants included in the study.
Consent for publication
Written informed consent for publication of clinical data was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, W.W., Zhu, M., Lam, E.T. et al. A phase I pharmacokinetic and safety study of Paclitaxel Injection Concentrate for Nano-dispersion (PICN) alone and in combination with carboplatin in patients with advanced solid malignancies and biliary tract cancers. Cancer Chemother Pharmacol 87, 779–788 (2021). https://doi.org/10.1007/s00280-021-04235-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-021-04235-z