Abstract
Purpose
There is little information on tolerability to cisplatin-based chemotherapies in patients with a solitary kidney after nephroureterectomy. We evaluated the impact of having a solitary kidney on tolerability to gemcitabine plus cisplatin (GC) chemotherapy in urothelial carcinoma patients.
Methods
We retrospectively reviewed medical records of patients treated between August 2007 and November 2015. Eligible patients had received GC as first-line chemotherapy, including as neoadjuvant and adjuvant treatment. Patients who commenced GC chemotherapy after nephroureterectomy comprised the solitary kidney (SK) group; the remaining patients (i.e., those with both kidneys) comprised the BK group. Incidences of hematologic toxicities and renal insufficiency were examined and compared between two groups.
Results
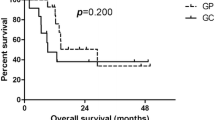
There were 16 patients in the SK group and 31 in the BK group. The incidence of hematologic toxicity (grade 3/4) was not significantly different between the two groups (neutropenia: 68.8 vs. 74.2%, respectively (P = 0.959); thrombocytopenia: 31.2 vs. 51.6%, respectively (P = 0.307); and anemia: 12.5 vs. 38.7%, respectively (P = 0.094)). Multivariate analysis revealed no statistically significant association between having a SK and severe hematologic toxicities. Moreover, no significant differences were observed in the incidence of acute kidney injury. The mean differences in serum creatinine and estimated glomerular filtration rate between baseline and each post-chemotherapy cycle were similar when comparing the SK and BK groups.
Conclusions
There is no evidence that tolerability to GC chemotherapy is inferior in patients with a solitary kidney. Therefore, there may be no need to avoid administering CDDP-based chemotherapy to such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract carcinoma may develop in any tissue where transitional epithelium is present, including in the renal pelvis, ureter, bladder, and proximal two-thirds of the urethra [1, 2]. Urothelial (transitional cell) carcinoma is the most common histologic subtype, accounting for more than 90% of urinary tract carcinoma [1]. More than 90% of urothelial carcinomas (UCs) originate in the bladder. Upper urinary tract urothelial carcinomas (UUTUCs), including those that originate in the renal pelvis or ureter, are relatively uncommon [3].
Radical nephroureterectomy is the standard treatment in UUTUC patients as well as those with bladder cancer that has invaded the ureter [2]. After nephroureterectomy, patients have an anatomic solitary renal unit, the so-called solitary kidney. However, UUTUC has a high local and systemic failure rate, even after radical surgery, and 5-year survival rates in patients with a pT3 or higher-stage lesion have been reported to be <50% [4]. Consequently, clinical guidelines recommend adjuvant systemic chemotherapy in UCs with a pathological stage of pT2/3 or greater and/or lymph node positivity; however, there is conflicting data regarding the efficacy of such treatments [2], as metastatic or recurrent disease following surgery may be managed with systemic chemotherapy as well [2, 5]. In each of these treatments strategies, cisplatin (CDDP)-based chemotherapy (CBCT) has been shown to be effective; the gemcitabine plus cisplatin (GC) regimen is commonly used in clinical practice [2, 5].
Hematologic toxicities such as neutropenia, thrombocytopenia, and anemia are the most frequent side effects in GC chemotherapy [5, 6]. Furthermore, nephrotoxicity is recognized as the dose-limiting adverse effect of CDDP [7, 8]. Hence, hematologic toxicities and renal insufficiency are the side effects in most strongly indicative of CDDP tolerability.
There is little information on the tolerability of patients with a solitary kidney to the administration of CDDP. Although a previous retrospective study investigated renal safety in patients with a solitary kidney who received long-term CBCT [9], no studies to compare tolerability between patients with a solitary kidney and control patients have been performed to our knowledge. Furthermore, the presence of a solitary kidney is a criterion for ineligibility for CDDP administration in some advanced UC clinical trials [10]; therefore, it has been difficult to obtain information regarding CDDP tolerability in patients with a solitary kidney. To that end, we conducted this retrospective study to compare the incidences of hematologic toxicities and renal insufficiency between UC patients with a solitary kidney and those who have both kidneys to evaluate the impact of having a solitary kidney on the tolerability to GC chemotherapy.
Patients and methods
Patients and controls
This study was approved by the ethical review board at Nagoya City University Graduate School of Medical Sciences.
We retrospectively reviewed the medical records of patients treated at Nagoya City University Hospital, Japan, between August 2007 and November 2015. Eligible patients had UC of the bladder, renal pelvis, or ureter; had received no chemotherapy prior to GC chemotherapy; and were administered GC chemotherapy at least once at Nagoya City University Hospital. Patients administered GC chemotherapy for advanced or metastatic disease were eligible regardless of intent (whether neoadjuvant, adjuvant, or palliative). We excluded patients who received prophylactic granulocyte colony-stimulating factor for neutropenia, magnesium injections for CDDP-induced renal insufficiency, or erythropoiesis-stimulating agents. We also excluded patients with diabetes mellitus, multiple primary cancers, nephrectomy of both kidneys, and those who underwent hemodialysis. Patients with a hydronephrotic kidney were also excluded, as such patients may have had a potentially non-functional kidney (effectively, a functional solitary kidney). However, patients who commenced GC chemotherapy after their hydronephrotic kidney was resolved by an indwelling ureteral stent or nephrostomy were included in the study. The eligible patients were divided into two groups: the solitary kidney (SK) group (i.e., those who commenced GC chemotherapy after nephroureterectomy) and the remaining patients with both kidneys (the BK group) who comprised the controls.
Treatment protocol
Gemcitabine (GEM) 1,000 mg/m2 was administered by intravenous infusion for 30 min on days 1, 8, and 15 of a 28-day cycle. CDDP 70 mg/m2 was administered by intravenous infusion in 500 mL of normal saline over 180 min on day 2 of each cycle. Intravenous hydration (2000 mL per day) was provided on days 1, 2, and 3.
Observational period in each patient
The observational period in each patient was from day 1 of the 1st cycle to the end of the final cycle of GC chemotherapy or until November 2015, whichever was earlier; data from all completed cycles during this period were used. If a subsequent cycle did not commence within 28 days after completion of the previous cycle, that previous cycle was considered as the final cycle.
Evaluation of hematologic toxicities and renal safety
We evaluated hematologic toxicities and renal safety to compare the tolerability of GC chemotherapy between two groups. Neutropenia, thrombocytopenia, and anemia were used as indicators of hematologic toxicities and were evaluated according to the National Cancer Institute Common Toxicity Criteria for Adverse Events version 4.0. The incidences of grade 3/4 hematologic toxicities that developed during the chemotherapy cycles were compared between the groups. Renal safety was evaluated by noting the incidences of acute kidney injury (AKI) and any changes in renal function with the completion of GC chemotherapy cycles. The development of AKI was evaluated according to the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline criteria [11], and involved assessment by changes in serum creatinine (SCre) levels within 7 days after administration of CDDP. Differences in SCre and estimated glomerular filtration rate (e-GFR) between baseline and post-completion of each chemotherapy cycle were compared between the SK and BK groups.
Clinical data acquisition
All clinical variables were collected from patients’ medical records held by the Nagoya City University Hospital. Data on age, sex, SCre, e-GFR, serum albumin, Union for International Cancer Control TNM cancer staging, number of chemotherapy cycles, and doses of anti-cancer agents delivered were compared to background values in the SK and BK groups, and were also used to evaluate the association between the presence of a solitary kidney and hematologic toxicities. Actual doses of anti-cancer agents were calculated as the proportions of delivered dose to planned dose.
Statistical analysis
Differences between the SK and BK groups in terms of incidence of hematologic toxicities or AKI, as well as background clinical variables, such as sex, pre-existing cytopenia, and cancer stage, were compared by Fisher’s exact test or the chi-squared test. Age, SCre, e-GFR, and serum albumin were compared by Student’s t test. The differences between baseline and post-chemotherapy SCre and e-GFR after completion of each chemotherapy cycle were compared using Student’s t test. Multivariate analyses were performed using three types of logistic regression models: the unadjusted (crude) model; Model 1, which adjusted for age and sex; and Model 2, which adjusted for the variables in Model 1 plus established risk factors of chemotherapy-induced hematologic toxicities [2, 12, 13]. The established risk factors in Model 2 included the presence of a solitary kidney, the number of GC chemotherapy cycles, pre-existing cytopenia (of each and any type), serum albumin, and TNM stage IV. Each of these variables was excluded as an explanatory variable if used as an objective variable in any particular analysis. P < 0.05 was considered as statistically significant in this study; all statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [14].
Results
Characteristics of patients
Forty-seven patients were included in this study, the baseline characteristics of whom are summarized in Table 1. There were 16 patients in the SK group and 31 in the BK group. The ratios between the sexes were similar in both groups. Baseline renal function was significantly lower in the SK group than in the BK group (mean SCre levels were 1.17 ± 0.23 and 0.82 ± 0.25 mg/dL, while mean e-GFRs were 49.1 ± 10.6 mL/min/1.73 m2 and 70.4 ± 21.9 mL/min/1.73 m2, respectively). On the other hand, patients in the BK group tended to exhibit lower serum albumin and were more likely to have TNM stage IV tumors, although the differences were not significant. Baseline neutrophil count, platelet count, and hemoglobin levels were similar between the groups. The proportions of SK and BK patients who received adjuvant therapy were 81.2 and 32.3%, respectively; 18.8 and 48.4% received palliative therapy, respectively. No serious adverse events, including hand-foot syndrome, occurred in either group; only hematologic toxicities and renal insufficiency were observed.
Administration of anti-cancer agents
The anti-cancer agents were administered as summarized in Table 2. The median number of administered cycles was two in both groups, and the proportion of patients who received four or more cycles tended to be higher in the BK group than in the SK group (25.8 vs. 6.2%, respectively). There were no statistically significant differences between the two groups in the mean doses of CDDP and GEM actually delivered, whether in the 1st cycle or overall.
Evaluation of grade 3/4 hematologic toxicity
The incidences of grade 3/4 neutropenia (SK: 68.8%, BK: 74.2%; P = 0.959), thrombocytopenia (SK: 31.2%, BK: 51.6%; P = 0.307), and anemia (SK: 12.5%, BK: 38.7%; P = 0.094) were not significantly different between the SK and BK groups (Table 3). However, there were more incidences of thrombocytopenia within each grade in the BK group that within each grade of the SK group; moreover, the difference in the incidence of anemia between the two groups was particularly large. Additionally, there were no significant differences in the types of cytopenia between patients who received more than the median number of GC chemotherapy cycles vs. those who received less [neutropenia: 68.2 vs. 76.0%, respectively (P = 0.786); thrombocytopenia: 40.9 vs. 48.0%, respectively (P = 0.846); and anemia: 40.9 vs. 20.0%, respectively (P = 0.213)].
Multivariate analysis of the association between grade 3/4 hematologic toxicities and the presence of a solitary kidney
Crude and multivariate-adjusted analyses revealed no association between the presence of a solitary kidney and grade 3/4 neutropenia (Table 4a). Additionally, the other variables associated with the development of grade 3/4 neutropenia were not found to be influential. Similarly, there was no association between a solitary kidney and grade 3/4 thrombocytopenia or anemia on crude and multivariate-adjusted analyses (Table 4b, c). Conversely, serum albumin levels were significantly associated with grade 3/4 anemia (Table 4c). Pre-existing anemia (grade ≥1) was not significantly associated with grade 3/4 anemia in Model 2, although it was significantly associated according to Model 1.
Evaluation of renal safety
AKI incidence rates were similar in the SK and BK groups (6.2% [1/16] and 9.7% [3/31], respectively; data not shown). Although changes in SCre and e-GFR were evaluated after each GC chemotherapy cycle up to the 3rd since only one patient received over three cycles in the SK group (Table 5), no statistically significant differences were observed between the two groups in terms of mean SCre and e-GFR between baseline and post-chemotherapy treatment after each cycle.
Discussion
There was no statistically significant association between the presence of a solitary kidney and grade 3/4 hematologic toxicities, even after adjusting for age, sex, and established risk factors of chemotherapy-induced hematologic toxicities [12, 13]. Moreover, renal toxicity was not significantly different between the two groups. These results suggest that tolerability of patients with a solitary kidney to CBCT is not inferior to those who have both their kidneys.
The intensity of chemotherapy did not differ between the two groups, although renal function in the SK group was significantly lower than that in the BK group. The incidences of hematologic toxicities would therefore be expected to be higher in the SK group than in the BK group; however, there were no significant differences in the incidences of each tested type of cytopenia between the groups. In fact, patients in the BK group tended to exhibit higher incidences of cytopenia than those in the SK group; the difference was particularly large for anemia. Furthermore, multivariate analysis revealed an association between low serum albumin at baseline and grade 3/4 anemia.
In the present study, patients in the BK group tended to exhibit lower serum albumin levels at baseline and to undergo a greater number of GC chemotherapy cycles. Additionally, neither hepatic metastasis at baseline nor severe hepatic toxicity was observed in any of the patients during chemotherapy. Therefore, our results suggest that the patients’ nutritional statuses or the number of chemotherapy cycles administered likely contributed to the development of anemia, but not to any effects specific to having a solitary kidney.
The evaluation of renal safety was limited to the first three cycles of GC chemotherapy, as only one solitary kidney patient was administered over three cycles. However, we detected no evidence that renal safety was inferior among patients with a solitary kidney.
Generally, neoadjuvant or adjuvant chemotherapy is administered as part of a previously planned number of cycles in patients with solid tumors, and 3–4 cycles of GC chemotherapy are recommended for UC patients in such settings [2]. In the present study, 81.2% of SK group patients received UC in an adjuvant setting, indicating that the majority of patients in this group had 3–4 cycles preplanned. In fact, the mean number of cycles was not significantly different between SK and BK group patients (2.3 and 2.4 cycles, respectively; P = 0.799 using the Student’s t test; data not shown) on subgroup analysis of neoadjuvant or adjuvant settings. Hence, the reason for not administering more than three cycles to most SK group patients was unlikely to be due to poor CDDP tolerability.
A previous retrospective study in patients with a solitary kidney after nephroureterectomy for UUTUC evaluated the changes in renal function after long-term CBCT administration (a maximum of 21 cycles) [9]. The authors concluded that long-term CBCT can be administered to the majority of solitary kidney patients without severe renal dysfunction. However, their study did not include a control population (i.e., patients who had both kidneys). Moreover, hematologic toxicities are not evaluated despite the fact that renal dysfunction is one of the risk factors of chemotherapy-induced neutropenia or anemia [12, 13], and patients with a solitary kidney tend to develop reduced renal function post-nephroureterectomy. To our knowledge, our present study is the first to compare tolerability to CBCT between patients with a solitary kidney and those with both kidneys, and in which hematologic toxicities and renal safety are used as indicators. While we showed that patients with a solitary kidney did not have inferior tolerability to those with both kidneys, and a prospective control study is required to confirm the equivalence.
Radical nephrectomy is known to be a significant risk factor for the development of chronic kidney disease [15]. Therefore, the assumed risk of nephrotoxicity in patients with a solitary kidney may deter oncologists from administering CDDP; it has been reported that only 22% of patients with high-risk UUTUC after nephroureterectomy receive adjuvant chemotherapy [16]. However, all solitary kidney patients in our study were treatable with GC chemotherapy without experiencing unacceptable toxicities such as treatment-related death or referral to hemodialysis. These results strongly suggest that it is possible to administer GC chemotherapy to patients with a solitary kidney.
The present study has several limitations. First, it was a retrospective study using a small and diverse population. Therefore, the performance status (PS) was unknown, although poor PS at baseline is one of the risk factors of severe neutropenia [12]. Moreover, the study population was heterogeneous, especially in terms of nutritional state and treatment goal. Second, selection bias could not be avoided; however, we analyzed all patients regardless of treatment goals or cancer stage to reduce bias as much as possible after excluding those with factors that could influence the evaluation of hematologic toxicities or renal safety.
In conclusion, patients with a solitary kidney may be eligible for CBCT. When administering CBCT to such patients, the same risk factors for hematologic toxicities as those considered for patients with both kidneys, including nutritional state before administration, should be taken into account.
References
Lynch CF, Cohen MB (1995) Urinary system. Cancer 75:316–329
National Comprehensive Cancer Network (2016) NCCN clinical practice guidelines in oncology. Bladder cancer, Version 2. http://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf. Accessed 23 Sept 2016
Chalasani V, Chin JL, Izawa JI (2009) Histologic variants of urothelial bladder cancer and nonurothelial histology in bladder cancer. Can Urol Assoc J 3:S193–S198
Hall MC, Womack S, Sagalowsky AI, Carmody T, Erickstad MD, Roehrborn CG (1998) Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology 52:594–601
von der Maase H, Hansen SW, Roberts JT, Dogliotti L, Oliver T, Moore MJ, Bodrogi I, Albers P, Knuth A, Lippert CM, Kerbrat P, Sanchez Rovira P, Wersall P, Cleall SP, Roychowdhury DF, Tomlin I, Visseren-Grul CM, Conte PF (2000) Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 18:3068–3077
Moore MJ, Winquist EW, Murray N, Tannock IF, Huan S, Bennett K, Walsh W, Seymour L (1999) Gemcitabine plus cisplatin, an active regimen in advanced urothelial cancer: a phase II trial of the national cancer institute of Canada clinical trials group. J Clin Oncol 17:2876–2881
Loehrer PJ, Einhorn LH (1984) Drugs 5 years later Cisplatin. Ann Intern Med 100:704–713
Go RS, Adjei AA (1999) Review of the comparative pharmacology and clinical activity of cisplatin and carboplatin. J Clin Oncol 17:409–422
Dogliotti L, Cartenì G, Siena S, Bertetto O, Martoni A, Bono A, Amadori D, Onat H, Marini L (2007) Gemcitabine plus cisplatin versus gemcitabine plus carboplatin as first-line chemotherapy in advanced transitional cell carcinoma of the urothelium: results of a randomized phase 2 trial. Eur Urol 52:134–141. doi:10.1016/j.eururo.2006.12.029
Galsky MD, Hahn NM, Rosenberg J, Sonpavde G, Hutson T, Oh WK, Dreicer R, Vogelzang N, Sternberg CN, Bajorin DF, Bellmunt J (2011) Treatment of patients with metastatic urothelial cancer “unfit” for cisplatin-based chemotherapy. J Clin Oncol 29:2432–2438. doi:10.1200/JCO.2011.34.8433
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Lyman GH, Kuderer NM, Crawford J, Wolff DA, Culakova E, Poniewierski MS, Dale DC (2011) Predicting individual risk of neutropenic complications in patients receiving cancer chemotherapy. Cancer 117:1917–1927. doi:10.1002/cncr.25691
Schwartz RN (2007) Anemia in patients with cancer: incidence, causes, impact, management, and use of treatment guidelines and protocols. Am J Health Syst Pharm 64:S5–S13. doi:10.2146/ajhp060601
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. doi:10.1038/bmt.2012.244
Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV, Scardino PT, Russo P (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 7:735–740. doi:10.1016/S1470-2045(06)70803-8
Hellenthal NJ, Shariat SF, Margulis Karakiewicz PI, Roscigno M, Bolenz C, Remzi M, Weizer A, Zigeuner R, Bensalah K, Ng CK, Raman JD, Kikuchi E, Montorsi F, Oya M, Wood CG, Fernandez M, Evans CP, Koppie TM (2009) Adjuvant chemotherapy for high risk upper tract urothelial carcinoma: results from the upper tract urothelial carcinoma collaboration. J Urol 182:900–906. doi:10.1016/j.juro.2009.05.011
Funding
This study did not rely on any external sources of funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Kondo, M., Hotta, Y., Ando, R. et al. The impact of a solitary kidney on tolerability to gemcitabine plus cisplatin chemotherapy in urothelial carcinoma patients: a retrospective study. Cancer Chemother Pharmacol 79, 995–1001 (2017). https://doi.org/10.1007/s00280-017-3277-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3277-x