Abstract
Purpose
Women at high risk of breast cancer and those with carcinoma in situ need non-toxic, well-tolerated preventive interventions. One promising approach is drug delivery through the breast skin (local transdermal therapy, LTT). Our goal was to test novel drugs for LTT, to establish that LTT is applicable to non-steroidal drugs.
Methods
Athymic nude rats were treated with oral tamoxifen, transdermal 4-hydroxytamoxifen (4-OHT) or endoxifen gel applied daily to the axillary mammary gland for 6 weeks (Study 1). Study 2 was identical to Study 1, testing transdermal telapristone acetate (telapristone) gel versus subcutaneous implant. At euthanasia, mammary glands and blood were collected. In Study 3, consenting women requiring mastectomy were randomized to diclofenac patch applied to the abdomen or the breast for 3 days preoperatively. At surgery, eight tissue samples per breast were collected from predetermined locations, along with venous blood. Drug concentrations were measured using liquid chromatography–tandem mass spectroscopy.
Results
Mammary tissue concentrations of 4-OHT, endoxifen, and telapristone were significantly higher in the axillary glands of the gel-treated animals, compared to inguinal glands or to systemically treated animals. Plasma concentrations were similar in gel and systemically treated animals. The clinical trial showed significantly higher mammary concentrations when diclofenac was applied to the breast skin versus the abdominal skin, but concentrations were variable.
Conclusions
These results demonstrate that lipophilic drugs can be developed for LTT; although the nude rat is suitable for testing drug permeability, delivery is systemic. In human, however, transdermal application to the breast skin provides local delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite successful breast cancer prevention trials that established the efficacy of selective estrogen receptor modulators [1] and aromatase inhibitors [2, 3], the acceptance of these drugs by women at high risk of breast cancer has been low. Reasons include quality-of-life impairments, the possibility of more serious side effects, and reluctance by healthy women to take oral medication for prevention. However, breast cancer prevention requires only that the breast be exposed to the drug; systemic exposure is both unnecessary and harmful. Oral tamoxifen is a good example; 5 years of systemic exposure leads to benefits to the breast and bone, but with costs to quality of life and health [4–6]. The avoidance of systemic exposure through prevention strategies that target the breast locally, and have minimal systemic toxicity, may overcome these barriers. One proposed method of local therapy to the breast involves drug delivery to the ductal epithelium by cannulating the ductal orifice with a catheter [7]. However, this requires an office procedure by a specialist, the value of a single injection is not known, the feasibility of multiple injections is untested, and dissemination across multiple practice settings and varied clinical environments seems dubious. A far simpler alternative is transdermal delivery of drugs through the breast skin; its advantages include the avoidance of fast hepatic metabolism, non-invasiveness, and self-administration across the globe without costly devices. Therefore, local transdermal therapy (LTT) to the breast is likely to improve the tolerability and the acceptance of pharmacological cancer prevention regimens by women.
The unique features of the breast predict the success of LTT; these include the embryological origin of the breast as a skin appendage [8] with a well-developed internal lymphatic circulation [9] and the presence of a subcutaneous and retromammary fatty envelope. We hypothesize that the fatty envelope of the breast may serve as drug reservoir for prolonged distribution to the breast, aided by the intra-mammary lymphatic circulation, so that transdermally delivered drugs are disseminated throughout the breast.
Previous studies of LTT, including our recently completed preoperative trial testing 4-OHT gel in women with ductal carcinoma in situ (DCIS), suggest that delivery is local with minimal systemic exposure and good biological effect [10–12]. These data prompt further questions: (1) Are other drugs candidates for LTT? (2) Is hormone receptor binding required? (3) What is the variability of drug distribution through the breast? In the present report, we describe a series of experiments to address these questions. In a rat model, we compare two tamoxifen metabolites (4-OHT and endoxifen) and test telapristone, an anti-progestational agent. We compare the drug concentrations of mammary tissue and plasma by transdermal delivery, to those achieved by systemic therapy. Given important differences between rodent and human mammary glands, and to test a non-steroid receptor binding drug, we have conducted a clinical trial to test the hypothesis that application of a transdermal diclofenac patch on the breast will result in higher breast concentrations of diclofenac than patch application to the abdomen, thus establishing that LTT to the breast constitutes local rather than systemic therapy.
Materials and methods
Materials
(Z) tamoxifen was purchased from Toronto Research Chemicals, Inc. (Toronto, Canada). 4-OHT (E:Z = 50:50), oleic acid, sesame oil, and anhydrous ethanol were purchased from Sigma-Aldrich, Inc. (Z) endoxifen citrate salt (>97 %) was a gift from Jina Pharmaceuticals, Inc. (Libertyville, IL, USA). Telapristone was a gift from Repros Therapeutics, Inc. (The Woodlands, TX, USA). Klucel hydroxypropyl cellulose (viscosity-type HF, 30,000 mPas) was purchased from Hercules Incorporated (Wilmington, DE, USA). Telapristone pellets (30 mg, 60 days release) were manufactured by Innovative Research of America, Inc. (Sarasota, FL, USA). Customized rat jackets were manufactured by Lomir Biomedical, Inc. (Quebec, Canada). Diclofenac patches (Flector® patches) were purchased from Pfizer Inc.
Preparation of medications for rats
(Z) tamoxifen was prepared as 3 mg/mL in sesame oil. For transdermal gel formulations, 4-OHT (E:Z = 50:50) (1 mg/mL), (Z) endoxifen (1 mg/mL), and telapristone (1.5 mg/mL) were prepared in 60 % (v/v) ethanol–phosphate buffer containing 0.5 % (v/v) oleic acid [13] with 1.5 % (w/v) Klucel hydroxypropyl cellulose.
Animal studies and treatments
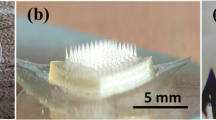
Studies 1 and 2, see Fig. 1: Animal experiments were approved by the Animal Care and Use Committee of Northwestern University. Athymic nude rats (Hsd:RH-Foxn1rnu/rnu, Harlan Laboratories, Inc.) were provided with standard laboratory food and water ad libitum. In Study 1, rats weighting 180–200 g were randomized to four groups (no treatment control, 4-OHT gel, endoxifen gel, and oral tamoxifen) and treated daily for 6 weeks. In the gel groups, animals were anesthetized with isoflurane inhalation; the skin surface of axillary mammary glands was cleaned with alcohol swabs and air-dried; 0.1 mL drug gel was applied using a template with an exposed ellipse (π × R 1 × R 2 = π × 1 cm × 0.6 cm) around the no. 2 nipple on each side and allowed to dry (total of 1, 0.5 mg/kg/day on each side); animals wore jackets fitted over the forelegs, to prevent loss of gel through grooming. In the oral tamoxifen group, the tamoxifen (3 mg/kg/day) was delivered through feeding needles (20G-3″, Cadence Science Inc.), and the animals wore jackets and were exposed to anesthesia similar to the transdermal treatment group.
Preclinical studies to test local transdermal therapy to mammary tissues. a Chemical structures of study drugs. b Preclinical studies were designed to compare transdermal delivery with systemic delivery methods. The control group of Study 1 was no treatment group, and the rats treated with placebo pellet and placebo gel were the control groups of Study 2. c Transdermal gels were applied to the skin area around second nipples of axillary mammary glands (yellow circle), and jackets were used to prevent the drug ingestion by the animals. Axillary and inguinal mammary fat pads and blood from heart were collected for determination of drug concentration
In Study 2, we compared subcutaneous versus transdermal administration of telapristone. Rats were randomized to three groups (no treatment control, telapristone gel, and telapristone implant). The transdermal group was prepared and treated with telapristone gel (1.5 mg/kg/day) similar to Study 1. The implant group was subcutaneously given with telapristone pellet (30 mg, 60 days release) in lower dorsal area and delivered 2.5 mg/kg/day, assuming zero-order kinetics. All rats wore jackets and were exposed to anesthesia.
In both studies, rats were euthanized after 6 weeks of treatment for blood and tissue collections. The treated skin area was cleansed with alcohol prior to dissection. Blood samples were collected from the heart. We collected the whole mammary glands (1 axillary and 1 inguinal) per animal and measured their drug concentrations separately.
Study 3: Diclofenac patch in women
A pilot study to test the uniformity of transdermal drug delivery to the breast using diclofenac epolamine patch was approved by the Northwestern University Institutional Review Board (http://www.clinicaltrials.gov, NCT01380353). Non-pregnant women scheduled for mastectomy to prevent or treat breast cancer were recruited through the Lynn Sage Comprehensive Breast Center of Northwestern Medicine. All participants were randomized to patch application to one surgical breast (per participant) or the abdominal skin. The diclofenac patch (Flector® patch, 10 cm × 14 cm) is a semi-occlusive, bioadhesive patch containing 129.7 mg of diclofenac acid. After baseline evaluation, the participants were instructed on site of patch application and to replace patch every 12 h over 72 h prior to surgery.
The structure of diclofenac and schema of patch applications are shown in Fig. 2a. The breast group wore the patch over the upper outer breast, with the lower inner corner of the patch at the level of the nipple (Fig. 2b). The abdominal group wore the patch on the lower abdomen on the side opposite the planned mastectomy (Fig. 2a). Participants were assessed for baseline signs/symptoms and then by telephone the second day of the treatment and on the day of surgery. All adverse events were coded using the NCI Common Terminology Criteria for Adverse Events version 4.0.
Clinical trial to evaluate the distributions of diclofenac within the breast. a Chemical structure of diclofenac and the study schema. Women waiting for mastectomy were randomized either to breast patch group or to abdominal patch group of diclofenac using Flector patch®. b Fresh tissues were collected from predetermined sampling locations of the breast (1 through 8): an upper central (1), an outer central (2), a lower central (3), an inner central (4), an upper peripheral (5), an outer peripheral (6), a lower peripheral (7), and an inner peripheral (8) area. UIQ upper inner quadrant, UOQ upper outer quadrant, LIQ lower inner quadrant, LOQ lower outer quadrant. In the breast patch group, the patch (blue line) was worn over the upper outer breast, with the lower inner corner of the patch at the level of the nipple. Red highlighted inner central and peripheral locations (4, 5, 7, and 8) of breast patch group had significantly higher amount of diclofenac compared to abdominal patch group, and an outer peripheral location (6, yellow highlight) contained the least amount of diclofenac in breast patch group. c Representative compositions of the breast samples. Note that we sub-categorized tissue samples into three types: fatty type if the tissue on slide contains >75 % adipocytes; fibrous type if >75 % fibrous stroma; and mixed type (otherwise compositions). Diclofenac concentrations by the tissue compositions were represented in a scatter plot with median values (black bars). *p < 0.001
On the day of surgery, the transdermal patch was removed in the operating room prior to anesthesia and 30 mL venous blood was collected with anticoagulant K2EDTA (BD Vacutainer®, BD Hemogard™ product no. 366643). Tissue samples from the mastectomy specimen were obtained from eight predetermined locations of one breast per participant (Fig. 2b), four central/periareolar and four peripheral samples 5 cm away, at 12, 3, 6, and 9 O’clock. Each tissue sample was weighed and snap-frozen in liquid nitrogen and kept in −80 °C until analysis.
Formalin-fixed, paraffin-embedded (FFPE) samples were taken from locations adjacent to the drug assay samples, for histological evaluation of tissue composition, and were available from all subjects. For the last nine subjects, each frozen tissue sample taken for drug assay had a face shaving taken for the evaluation of tissue composition before freezing.
Quantitation of plasma and tissue concentrations of drugs
The concentrations of all the drugs used in rats and humans were determined by liquid chromatography–tandem mass spectroscopy (API 3000; AB SCIEX, Foster City, CA, USA). Chromatographic separation was achieved with a Kinetex C18 2.6-μm column (50 mm × 2.1 mm, Phenomenex, Torrance, CA, USA) for rat samples and a BETASIL Phenyl-Hexyl 3-µm column (30 × 2.1 mm, Thermo Fisher Scientific Inc., Waltham, MA, USA) for human samples. The mobile phase was A: 0.1 % formic acid in water (v/v) and B: 0.1 % formic acid in acetonitrile (v/v). Details of sample processing and quantitation methods are described in the Supplementary Materials. The lowest limits of quantification (LLOQ) were as follow: tamoxifen and N-desmethyl tamoxifen (NDT) (plasma 10 ng/mL; tissue 40 ng/g); 4-OHT and endoxifen (plasma 0.5 ng/mL; tissue 2 ng/g); telapristone and N-desmethyl telapristone (d-telapristone) (plasma 1 ng/mL; tissue 1.5 ng/g); and diclofenac (plasma 0.5 ng/mL; tissue 2 ng/g).
Statistical design and analysis
For preclinical studies, the summary statistics as medians and interquartile range (IQR) were reported by treatment groups for each analyte obtained from plasma, axillary, and inguinal mammary glands. Concentration differences of each analyte between treatment groups and differences between mammary glands within each treatment group were assessed via the Wilcoxon rank-sum test, and the Wilcoxon signed rank-sum test, respectively. In the diclofenac clinical study, categorical variables comparing women in the treatment groups were compared using Fisher’s exact test (Table 3). The medians and IQR’s were reported for diclofenac concentrations by breast region and patch groups (Table 4). To compare breast concentrations by site of patch application, we replaced non-detectable values with “zero” and considered the median concentration from eight samples as the representative breast concentration per individual for statistical purposes. The Wilcoxon rank-sum test was used to assess median concentration differences between patch groups, among regions of the breast, and by menopausal status within each treatment group.
Results
The structures and the study schema of the agents for LTT studies are summarized in Fig. 1a, b for the preclinical studies, and in Fig. 2a for the clinical study.
Study 1: Oral TAM versus transdermal 4-OHT and endoxifen delivery in rats
We used a mixture of 4-OHT isomers (E:Z = 50:50) and the (Z) endoxifen isomer (>97 % pure) for transdermal gel formulations since these compounds have been used in human trials of transdermal 4-OHT gel [14] and oral endoxifen [15]. The (Z) isomers of 4-OHT and endoxifen are believed to be highly anti-estrogenic, whereas the (E) isomers are not [16]; both isomers have equivalent binding affinities to ERα [17].
Mammary concentrations [Table 1(a)]
Oral tamoxifen treatment resulted in mammary concentrations that were highest for NDT followed by tamoxifen, then endoxifen, and 4-OHT. Concentrations were significantly higher in inguinal than in axillary glands (p $ = 0.02 for all).
In the 4-OHT gel group, the mammary concentrations of (Z) 4-OHT were fourfold higher at the site of application (the axillary gland) than in the inguinal gland (p $ = 0.008). The axillary mammary concentration of (Z) 4-OHT was about sevenfold higher in the 4-OHT gel group than in the oral tamoxifen group (25.5 vs. 3.90 g/g, p < 0.001), whereas the inguinal concentration was comparable with that of the oral group (6.62 vs. 5.06 ng/g, p = 0.49). Furthermore, at both locations, the concentration of (Z) 4-OHT was higher than that of (E) 4-OHT (Z:E = 3:1 for the axillary gland, p = 0.001; 6:1 for the inguinal gland, p < 0.001). There was minimal conversion of 4-OHT to endoxifen in the 4-OHT gel group; the (Z) endoxifen concentration of the 4-OHT gel group was 0.34 and 0.27 ng/g in axillary and inguinal glands, respectively, significantly lower than in the oral tamoxifen group (p < 0.001).
In the endoxifen gel group, the concentration of (Z) endoxifen in the axillary gland was over fivefold higher than in the inguinal gland (p $ = 0.004), and eightfold higher than in axillary glands of the oral tamoxifen group (p < 0.001). The inguinal concentration of (Z) endoxifen was similar to that of the oral tamoxifen group (p = 0.43). Comparing the axillary glands of the two gel groups, the (Z) endoxifen concentration of the endoxifen gel group was higher than the (Z) 4-OHT concentration of the 4-OHT gel group (37.3 vs. 25.5 ng/g). Inguinal gland concentrations were similar (7.29 vs. 6.62 ng/g).
Plasma concentrations [Table 1(b)]
The plasma concentrations of tamoxifen and its metabolites in the oral tamoxifen treatment group were: NDT > tamoxifen > endoxifen > 4-OHT. In both gel groups, plasma concentrations were similar to the oral tamoxifen group; (Z) 4-OHT 1.61 versus 2.48 ng/mL, p = 0.39 and (Z) endoxifen 1.81 versus 2.96 ng/mL, p = 0.77. In the endoxifen gel group, we found trace levels of (Z) 4-OHT in the plasma of the endoxifen group (0.30 ng/mL), far lower than the levels in the oral tamoxifen group (p = 0.003) or the 4-OHT gel group (p # = 0.002).
Study 2: Comparison of transdermal versus subcutaneous implant of telapristone in rats
Telapristone is known to be primarily converted by CYP 3A4 in the liver to N-desmethyl telapristone (d-telapristone), a metabolite with similar anti-tumor activity; we measured both forms.
Mammary concentrations [Table 2(a)]
In the telapristone implant group, the concentration ratio of telapristone to d-telapristone was approximately 6 for both axillary and inguinal glands. The mammary concentrations of both telapristone and d-telapristone were higher in the inguinal gland than in the axillary gland (p $ = 0.055 for telapristone; p $ = 0.03 for d-telapristone). In the telapristone gel group, the mammary concentration of telapristone was sevenfold higher in axillary gland than in the inguinal gland (1212 vs. 167 ng/g, p $ < 0.004) and 26-fold higher than in the implant group (1212 vs. 46.5 ng/g, p < 0.001). The inguinal mammary concentration of telapristone was threefold higher in the gel group than in the implant group (167 vs. 53.1 ng/g, p = 0.02). The axillary mammary concentrations of d-telapristone was fourfold higher in the gel group than in the implant group (28.4 vs. 7.21 ng/g, p < 0.001), whereas the inguinal mammary concentration of d-telapristone was nonsignificantly lower in the gel group than in the implant group (6.05 vs. 8.42 ng/g, p = 0.09).
Plasma concentrations [Table 2(b)]
The plasma concentration of telapristone in the gel group (dose 1.5 mg/kg/day) was similar to the level of the implant group (10.9 vs. 13.2 ng/mL, p = 0.12). However, plasma concentrations of d-telapristone were significantly lower in the gel group than in the implant group (1.33 vs. 3.99 ng/mL, p < 0.001).
Study 3: A clinical trial of transdermal diclofenac to the breast or to the abdomen
Thirty women planning mastectomy were enrolled (September 2011–November 2012) and randomized to the breast group or the abdominal group. The diclofenac patch application started 3 days prior to surgery. Two women were withdrawn from analysis due to incorrect use of patch, and one withdrew consent, leaving 27 evaluable women: 14 in the abdominal and 13 in the breast group. The participant characteristics were similar between groups (Table 3).
Breast concentrations [Table 4(a)]
We measured diclofenac concentrations using fresh-frozen tissue samples collected from eight predetermined locations of the mastectomy specimen (Fig. 2b). In the abdominal group, 65/112 tissue samples (58 %) demonstrated detectable diclofenac. Two women had no detectable diclofenac, nine displayed trace levels, and three showed a range of concentrations (1.2–4.8 ng/g) in their tissue samples. In the breast group, diclofenac concentrations were measured in 96 (of 104 expected) tissue samples because we were not able to obtain all eight samples from two women. Diclofenac was detectable in all 13 women in the breast group and in 79 % (76/96) of tissue samples, although three women showed trace levels. A large variation in diclofenac breast tissue concentrations was observed, both within and between subjects. The overall breast concentration of diclofenac of the breast group was sixfold higher than that of the abdominal group (0.77 vs. 0.13 ng/g, p = 0.02).
The variation in diclofenac distribution throughout the breast was greater in the breast than in the abdominal group. Within each group, diclofenac concentrations were similar between the central locations (1 through 4) and peripheral locations (5 through 8). In the abdominal group, the median concentrations were 0.85 ng/g centrally versus 0.75 ng/g peripherally (p = 0.42); in the breast group, they were 4.91 ng/g centrally versus 9.92 ng/g, peripherally (p = 0.78). In both central and peripheral locations, the breast group had significantly higher median concentrations than the abdominal group (p = 0.006 for central and p < 0.001 for peripheral locations). The outer peripheral location (location 6 marked in yellow, Fig. 2b) contained the lowest amount of diclofenac in breast group [Table 4(a)], but even here the concentration remained higher in the breast patch than in the abdominal patch group (0.31 vs. 0.04 ng/g tissue).
Drug concentrations by tissue composition of the breast samples
Based on histological examination of FFPE and frozen samples for drug quantitation (see “Materials and methods”), we categorized tissue samples into fatty, fibrous, and mixed types (Fig. 2c). The proportion of fatty, fibrous, and mixed samples was similar between the 134 FFPE and the 72 frozen samples. For both FFPE and frozen sample, the mixed-type samples were most numerous (58–62 %), followed by the fibrous (20–30 %) and then the fatty type (11–18 %) (Supplementary materials; Fig. 1a). Among the 72 frozen samples from nine women, the distribution in the abdominal group was: two fatty, 10 fibrous, and 20 mixed samples; in the breast group, six fatty, 12 fibrous, and 22 mixed samples. Since there were only eight fatty samples, we did not separate the samples by patch group for the analysis. The median breast concentrations of diclofenac with IQR were 8.71 (0.15, 29.4) ng/g in fatty samples, 0.52 (0.13, 1.42) ng/g in the mixed samples, and 0.19 (0.00, 0.58) ng/g in fibrous samples (Fig. 2c). Fatty samples contained significantly more diclofenac than fibrous or mixed type (fatty vs. fibrous, p = 0.008; fatty vs. mixed, p = 0.005); however, there was no concentration difference between fibrous and mixed tissue types (p = 0.93).
Correlations of diclofenac breast concentrations with age, body mass index (BMI), and breast size
Diclofenac breast concentrations significantly decreased with increasing age in the abdominal group (Spearman correlation coefficient, r = −0.77, p = 0.001), but not in the breast group (r = 0.20, p = 0.51) (Supplementary material; Fig. 1b). There was no significant correlation between breast concentration of diclofenac and BMI in either group (r = −0.26, p = 0.37 in abdominal group; r = −0.38, p = 0.20 in breast group) (Supplementary materials; Fig. 1c). Finally, to see whether breast size affects drug distribution, we grouped women into small, medium, and large breasts based on bra cup sizes (small = A and B; medium = C and D; large = DD, E, and H). There were 11 women with small, 13 women with medium, and 3 women with large breasts, only one of whom belonged to the breast patch group. We were therefore not able to examine the effect of breast size larger than D cup. There was no significant difference in diclofenac concentration by small or medium breast size within each patch group. In the abdominal group, the median concentrations were 0.60 (0.06, 1.20) ng/g and 0.21 (0.00, 0.32) ng/g for small (n = 5)-, and medium-sized breasts (n = 7), respectively (p = 0.22). In the breast group, corresponding values were 1.12 (0.23, 8.70) ng/g and 1.31 (0.06, 2.97) ng/g for small (n = 6)-, and medium-sized (n = 6) breasts, respectively (p = 0.75).
Plasma concentrations [Table 4(a)]
The median plasma concentration of diclofenac in the breast patch group was similar to that of the abdominal patch group (1.02 vs. 1.06 ng/mL, p = 0.73).
Adverse events
We did not observe any skin irritation in rats, changes in general health, or weight loss, among controls, or any of the treatment groups. Women did not report any common side effects including skin irritation due to patch application.
Discussion
There are presently two seminal problems in the field of breast cancer prevention: the low acceptance of proven drugs and the lack of drugs that prevent non-luminal breast cancer. The approach we present here has the potential to address both of these barriers. Since only the breast needs to be exposed to a drug for breast cancer prevention and for therapy of DCIS, effective drug therapy that can be limited to the breast should increase acceptance by reducing toxicity through low systemic exposure. This in turn will allow the development of drugs that will target other sub-types of breast cancer but cannot at present be considered for breast cancer prevention because of safety concerns. Together, these two attributes of local therapy for breast cancer prevention carry the seeds of high-impact innovations in this area.
In the present report, building on encouraging data on LTT with 4-OHT [11, 12], we address key questions that will guide the design of additional trials. In preclinical studies, we assessed whether the nude rat was a suitable model for the study of LTT and evaluated additional drug candidates for LTT. We found that dermal permeation of all three steroid receptor modulators (4-OHT, endoxifen, and telapristone) was excellent, with the highest drug concentrations observed in the targeted axillary mammary gland; markedly lower inguinal gland concentrations were seen in all three transdermal groups. Contrary to expectations, however, plasma levels of these drugs were similar with transdermal and with systemic delivery; thus, the rat model, although useful to define permeability, does not test local therapy. The differences between human and rodent mammary gland topology are important to remember in interpreting these differences, since human data from previous studies [10-12] and the present Study 3 consistently demonstrate the validity of LTT in humans. Using a diclofenac patch, we were able to show that local transdermal delivery provides high concentrations in the breast, compared to transdermal application elsewhere. For the clinical trial, we could not use the same drugs as in the rat studies since these are not currently available for human use, but the use of diclofenac allows us to conclude that selective retention in the breast also occurs with non-steroidal drugs.
Nevertheless, our rodents studies did demonstrate that excellent axillary mammary concentrations of (Z) 4-OHT, (Z) endoxifen, and telapristone can be achieved by transdermal administration and that this is not dependent on the presence of estrogen receptor-rich tumors, as suggested by previous authors [10, 11]. The high drug concentrations observed in the axillary mammary gland replicate the human data and provide evidence that both of the new drugs tested (endoxifen and telapristone) show superior permeation and retention in the axillary gland, compared to 4-OHT, and are candidates for further development as transdermal agents for the breast.
The plasma concentrations of tamoxifen and its metabolites (NDT, 4-OHT and endoxifen) after oral dosing (3 mg/kg/day) were similar to those observed in previous study comparing rats and humans [18]. Likely reasons for the systemic exposure that we observed with transdermal delivery include the difficulty of ensuring that the gel was applied only to the skin area of the mammary gland/fat pad, given the small area and the flat structure of rat mammary gland/fat pad. Furthermore, rat skin is more permeable than human skin [19, 20], and it is possible that the transdermal doses that we chose were too high. Unfortunately, there is no animal model which perfectly mimics the morphology and physiology of human breast. We used nude rats because they are preferable to mice for the testing of transdermal delivery; rabbits and guinea pigs have been used in dermatotoxicology testing, and the domestic pig is the closest match to human skin. However, the human breast is a three-dimensional structure, each breast has a fatty envelope, is a compact unit with abundant fat and stroma, and a fairly distinct border to the skin envelope. No other non-primate mammal has a similar anatomy. For these reasons, we conclude that although non-human models can be used to test drug permeability, testing of the local component of the LTT concept needs to be performed in humans.
Surprisingly, for both tamoxifen and telapristone, systemic delivery resulted in higher concentrations of each drug and its metabolites in the inguinal than in the axillary gland. This unequal distribution across mammary glands implies that even with systemic delivery, tissue distribution of drugs in the same organ depends on local conditions.
We cannot comment on the efficacy of transdermal delivery based on the present data, but the effectiveness of endoxifen as a prevention agent is not in question given the long experience with tamoxifen and the emerging data on oral endoxifen [21]. Preclinical data on telapristone are promising [22, 23], but it is untested as a prevention agent in humans. We are presently conducting a presurgical window trial in Stage I–II breast cancer patients, the results of which will guide further development (NCT01800422).
We have previously discussed the importance of the embryological origin of the breast as a modified sweat or eccrine gland [12, 13], with the parenchyma and its skin envelope comprising a single unit with a well-developed internal lymphatic and venous circulation [8, 24, 25]. This anatomy predicts that drugs applied to the breast skin should concentrate in the parenchyma to a greater degree than if applied to skin elsewhere, that LTT can be generalized to any drug that can penetrate the skin, and that receptor binding is not involved. Diclofenac, non-steroidal anti-inflammatory drug (NSAID), is a cyclooxygenase inhibitor and therefore a potentially effective breast cancer prevention agent [26]; it is available as a patch for analgesic use, with low systemic exposure [27]; a tissue reservoir forms when diclofenac is applied to the skin of joints [27, 28]; and binding of diclofenac within the breast to its target enzyme is expected to represent a minor component of its retention in adipose tissue of the breast. Additionally, the absence of cardiovascular and gastrointestinal toxicity or a platelet effect allowed use in the preoperative period. Our clinical trial tested breast application (local) with abdominal application (systemic) of the patch. An additional oral diclofenac group, although ideal, was not feasible related to concerns about platelet effects during the surgical procedure. Our results, showing significantly (sixfold) higher breast tissue concentrations of diclofenac when the patch was applied to the breast, provide proof-of-principle that extends the concept of LTT to non-steroidal drugs.
Transdermal penetration of NSAIDs has been previously reported as variable [28] with high inter-individual variation in plasma and urine levels of exposed subjects. As hypothesized, the breast concentrations of diclofenac of the breast patch group were significantly higher than those of the abdominal patch group, and not surprisingly, plasma concentrations of diclofenac were similar between breast and abdominal patch groups. Diclofenac breast concentrations declined significantly with increasing age in the abdominal patch group, but not in the breast patch group. BMI showed no significant correlation with breast concentration of diclofenac in both groups, and there was a nonsignificant decline in diclofenac concentrations in C–D cup compared to A–B cup-sized breasts.
We found that the tissue distribution of diclofenac in the eight breast regions of each woman was non-homogeneous in both groups, with greater variation in the breast group, where concentrations were also significantly higher. Fatty tissue samples contained significantly more diclofenac than other types, although the small number of fatty samples limits definitive conclusions. Recognizing the complex structure of breast tissue, we used the entire 100-mg tissue specimen for extraction and analyzed drug concentrations in duplicate, but assay variation related to tissue composition remains a concern. It is intriguing that the paucity of drug at location 6 (outer peripheral) in breast group was unlikely due to a mechanical reason (such as patch non-adherence at the edge). Whether this is related to lymphatic circulation, tissue composition, or other factors will need further study, but is reminiscent of the lower drug levels in the axillary gland of rats that were observed with both tamoxifen and telapristone delivered systemically. Of note, there are no previous studies of drug distribution through the breast, even with oral delivery, no gold standard exists, and the degree of variation with oral delivery is unknown. Although breast drug concentrations achieved with transdermal delivery may be lower or more variable than those achieved with oral delivery, it is helpful to recall that for disease prevention drug dose should be defined as the lowest effective dose, rather than the maximal tolerated dose. Along these lines, data on low dose tamoxifen [29] are encouraging and remind us that the more relevant endpoint in early trials of transdermal therapy is biological effect rather than drug concentration.
Our future plans include an assessment of intra-mammary distribution of telapristone following transdermal versus oral delivery and the development of a gel formulation of endoxifen in partnership with the National Cancer Institute, an important consideration since new supplies of 4-OHT gel are not available. Encouragingly, transdermal permeation of both these drugs is superior to that of 4-OHT in the present study, and we have previously reported on the suitability of endoxifen for LTT [13, 30]. Since diclofenac is also available as a gel, this is another potentially fruitful avenue. We are presently conducting focus group studies of high-risk women to assess preferences between drug delivery routes. We continue to work on standardizing methods of drug concentration measurement in breast tissue.
In summary, we found that all three drugs tested in a rat model demonstrated excellent skin permeation with high tissue levels achieved in the target mammary gland; plasma concentrations, however, were similar between transdermal and systemic treatment, likely related to constraints which apply to the rat model. We also found that a diclofenac patch applied to the breasts of women results in significantly higher breast tissue concentrations overall, but with considerable variability across breast regions. Important next questions include definition of the biologically effective dose of transdermally applied drugs and how much variation in drug concentration is compatible with efficacy, recognizing the difficulties in drug concentration measurement in complex tissues.
References
Cuzick J, Sestak I, Bonanni B, Costantino JP, Cummings S, Decensi A, Dowsett M, Forbes JF, Ford L, LaCroix AZ et al (2013) Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data. Lancet 381(9880):1827–1834
Goss PE, Ingle JN, Ales-Martinez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, McTiernan A, Robbins J, Johnson KC, Martin LW et al (2011) Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med 364(25):2381–2391
Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, Saunders C, Roche N, Mansel RE, von MG et al (2013) Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): an international, double-blind, randomised placebo-controlled trial. Lancet 383(9922):1040
Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, Vogel V, Robidoux A, Dimitrov N, Atkins J et al (1998) Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 90(18):1371–1388
Port ER, Montgomery LL, Heerdt AS, Borgen PI (2001) Patient reluctance toward tamoxifen use for breast cancer primary prevention. Ann Surg Oncol 8(7):580–585
Day R, Ganz PA, Costantino JP, Cronin WM, Wickerham DL, Fisher B (1999) Health-related quality of life and tamoxifen in breast cancer prevention: a report from the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Clin Oncol 17(9):2659–2669
Stearns V, Mori T, Jacobs LK, Khouri NF, Gabrielson E, Yoshida T, Kominsky SL, Huso DL, Jeter S, Powers P et al (2011) Preclinical and clinical evaluation of intraductally administered agents in early breast cancer. Sci Transl Med 3(106):106ra108
Ackerman AB, Kessler G, Gyorfi T, Tsou HC, Gottlieb GJ (2007) Contrary view: the breast is not an organ per se, but a distinctive region of skin and subcutaneous tissue. Am J Dermatopathol 29(2):211–218
Suami H, Pan WR, Mann GB, Taylor GI (2008) The lymphatic anatomy of the breast and its implications for sentinel lymph node biopsy: a human cadaver study. Ann Surg Oncol 15(3):863–871
Pujol H, Girault J, Rouanet P, Fournier S, Grenier J, Simony J, Fourtillan JB, Pujol JL (1995) Phase I study of percutaneous 4-hydroxy-tamoxifen with analyses of 4-hydroxy-tamoxifen concentrations in breast cancer and normal breast tissue. Cancer Chemother Pharmacol 36(6):493–498
Rouanet P, Linares-Cruz G, Dravet F, Poujol S, Gourgou S, Simony-Lafontaine J, Grenier J, Kramar A, Girault J, Le Nestour E et al (2005) Neoadjuvant percutaneous 4-hydroxytamoxifen decreases breast tumoral cell proliferation: a prospective controlled randomized study comparing three doses of 4-hydroxytamoxifen gel to oral tamoxifen. J Clin Oncol 23(13):2980–2987
Lee O, Page K, Ivancic D, Helenowski I, Parini V, Sullivan ME, Margenthaler JA, Chatterton RT Jr, Jovanovic B, Dunn BK et al (2014) A randomized phase II presurgical trial of transdermal 4-hydroxytamoxifen gel versus oral tamoxifen in women with ductal carcinoma in situ of the breast. Clin Cancer Res 20(14):3672–3682
Lee O, Ivancic D, Chatterton RT, Rademaker A, Khan SA (2011) In vitro human skin permeation of endoxifen: potential for local transdermal therapy for primary prevention and carcinoma in situ of the breast. Breast Cancer Targets Ther 3(1):61–70
Mansel R, Goyal A, Nestour EL, Masini-Eteve V, O’Connell K (2007) A phase II trial of Afimoxifene (4-hydroxytamoxifen gel) for cyclical mastalgia in premenopausal women. Breast Cancer Res Treat 106(3):389–397
Ahmad A, Shahabuddin S, Sheikh S, Kale P, Krishnappa M, Rane RC, Ahmad I (2010) Endoxifen, a new cornerstone of breast cancer therapy: demonstration of safety, tolerability, and systemic bioavailability in healthy human subjects. Clin Pharmacol Ther 88(6):814–817
Lim YC, Li L, Desta Z, Zhao Q, Rae JM, Flockhart DA, Skaar TC (2006) Endoxifen, a secondary metabolite of tamoxifen, and 4-OH-tamoxifen induce similar changes in global gene expression patterns in MCF-7 breast cancer cells. J Pharmacol Exp Ther 318(2):503–512
Lim YC, Desta Z, Flockhart DA, Skaar TC (2005) Endoxifen (4-hydroxy-N-desmethyl-tamoxifen) has anti-estrogenic effects in breast cancer cells with potency similar to 4-hydroxy-tamoxifen. Cancer Chemother Pharmacol 55(5):471–478
Robinson SP, Langan-Fahey SM, Johnson DA, Jordan VC (1991) Metabolites, pharmacodynamics, and pharmacokinetics of tamoxifen in rats and mice compared to the breast cancer patient. Drug Metab Dispos 19(1):36–43
Morimoto Y, Hatanaka T, Sugibayashi K, Omiya H (1992) Prediction of skin permeability of drugs: comparison of human and hairless rat skin. J Pharm Pharmacol 44(8):634–639
Bartek MJ, LaBudde JA, Maibach HI (1972) Skin permeability in vivo: comparison in rat, rabbit, pig and man. J Invest Dermatol 58(3):114–123
Goetz MP, Suman VA, Reid JR, Northfelt DW, Mahr MA, Dockter T, Haluska PJ, Kuffel M, Burhow S, Safgren S et al (2013) A first-in-human phase I study of the tamoxifen (TAM) metabolite, Z-endoxifen hydrochloride (Z-Endx) in women with aromatase inhibitor (AI) refractory metastatic breast cancer (MBC) (NCT01327781). The 2013 San Antonio Breast Cancer Symposium 2013
Wiehle RD, Christov K, Mehta R (2007) Anti-progestins suppress the growth of established tumors induced by 7,12-dimethylbenz(a)anthracene: comparison between RU486 and a new 21-substituted-19-nor-progestin. Oncol Rep 18(1):167–174
Wiehle R, Lantvit D, Yamada T, Christov K (2011) CDB-4124, a progesterone receptor modulator, inhibits mammary carcinogenesis by suppressing cell proliferation and inducing apoptosis. Cancer Prev Res (Phila) 4(3):414–424
Povoski SP, Olsen JO, Young DC, Clarke J, Burak WE, Walker MJ, Carson WE, Yee LD, Agnese DM, Farrar WB (2006) Prospective Randomized trial comparing intradermal, intraparenchymal, and subareolar injection routes for sentinel lymph node mapping and biopsy in breast cancer. Ann Surg Oncol 13(2):10–11
Klimberg VS, Rubio IT, Henry R, Cowan C, Colvert M, Korourian S (1999) Subareolar versus peritumoral injection for location of the sentinel lymph node. Ann Surg 229(6):860–864
Cuzick J, Otto F, Baron JA, Brown PH, Burn J, Greenwald P, Jankowski J, La VC, Meyskens F, Senn HJ et al (2009) Aspirin and non-steroidal anti-inflammatory drugs for cancer prevention: an international consensus statement. Lancet Oncol 10(5):501–507
McCarberg BH, Argoff CE (2010) Topical diclofenac epolamine patch 1.3% for treatment of acute pain caused by soft tissue injury. Int J Clin Pract 64(11):1546–1553
Dehghanyar P, Mayer BX, Namiranian K, Mascher H, Muller M, Brunner M (2004) Topical skin penetration of diclofenac after single- and multiple-dose application. Int J Clin Pharmacol Ther 42(7):353–359
Decensi A, Robertson C, Viale G, Pigatto F, Johansson H, Kisanga ER, Veronesi P, Torrisi R, Cazzaniga M, Mora S et al (2003) A randomized trial of low-dose tamoxifen on breast cancer proliferation and blood estrogenic biomarkers. J Natl Cancer Inst 95(11):779–790
Yang Y, Pearson RM, Lee O, Lee CW, Chatterton RT, Khan SA, Hong S (2014) Dendron-based micelles for topical delivery of endoxifen: a potential chemo-preventive medicine for breast cancer. Adv Funct Mater 24(17):2442–2449
Acknowledgments
This work was supported by Breast Cancer Research Foundation for telapristone study, Lynn Sage Breast Cancer Research Foundation for diclofenac trial, and Susan G. Komen for the Cure for endoxifen study. We also appreciate Jina Pharmaceuticals, Inc., and Repros Therapeutics, Inc., for providing materials and other supports. The authors had full responsibility for the design of the study, the collection of the data, the analysis and interpretation of the data, the writing of the manuscript, and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, O., Ivancic, D., Allu, S. et al. Local transdermal therapy to the breast for breast cancer prevention and DCIS therapy: preclinical and clinical evaluation. Cancer Chemother Pharmacol 76, 1235–1246 (2015). https://doi.org/10.1007/s00280-015-2848-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2848-y