Abstract
Purpose
RACGAP1 is a Rac GTPase-activating protein involved in cell growth regulation, cell transformation and metastasis. The aim of the present study was to explore the prognostic and/or predictive significance of RACGAP1 mRNA expression on disease-free survival (DFS) and overall survival (OS) in high-risk early breast cancer patients and compare it to that of Ki67 protein expression and to the Nottingham prognostic index (NPI).
Methods
A total of 595 high-risk breast cancer patients were treated in a two-arm trial evaluating postoperative dose-dense sequential chemotherapy with epirubicin followed by CMF with or without paclitaxel. RNA was extracted from 314 formalin-fixed paraffin-embedded primary tumor tissue samples followed by one-step quantitative RT-PCR for assessing RACGAP1 mRNA expression.
Results
High RACGAP1 mRNA expression (above the median) was associated with poor DFS (log-rank, p = 0.002) and OS (p < 0.001). High histological grade, as well as high Ki67 protein expression, was more frequent in the high-expression group of RACGAP1. Results of the Cox multivariate regression analysis revealed that high RACGAP1 mRNA expression independently predicted poor overall survival (Wald’s p = 0.008). High Ki67 protein expression was also an adverse prognostic factor for death (p = 0.016), while high NPI score values were not.
Conclusions
High RACGAP1 mRNA expression, as assessed by qRT-PCR, was found to be of adverse prognostic significance in high-risk early breast cancer patients treated with dose-dense sequential chemotherapy. The utility of RACGAP1 mRNA expression in patient selection for treatment with aggressive chemotherapy regimens should be further explored and validated in larger cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a disease with declining mortality rates in both the USA and UK between 1990 and 2000 [1]. These reductions were probably due to the application of breast cancer screening, as well as the use of systemic adjuvant therapies in early breast cancer. Usually, the risk for recurrence is considered in the selection of patients who should be offered adjuvant treatment. This risk has been estimated by established prognostic factors, including tumor size, histological grade, lymph node involvement and hormone receptor status [2]. As we understand the biology of breast cancer, more prognostic factors, such as HER2, have being identified and, recently, other molecular approaches, such as classification and prognostic systems, have been described. These factors reflect the aggressiveness of the tumor, are usually interrelated and provide independent prognostic information [3].
The Rho family of guanosine triphosphatases (GTPases) is a subfamily of the Ras superfamily and consists of small (~21 kDa) signaling G proteins. The three most widely known Rho GTPases are Rho (A, B and C isoforms), Rac (1 and 2 isoforms) and Cdc42 [4]. The Rho family of GTPases has been described to act as “molecular switches” between an active GTP-bound and an inactive GDP-bound state to play a role in cell proliferation, motility, invasion and metastasis of breast cancer cells and is inactivated by GTPase-activating proteins (GAPs) [4]. The RACGAP1 gene encodes Rac GTPase-activating protein 1 (RACGAP1) that is essential for the induction of cytokinesis [5] and may therefore promote cancer proliferation and growth, despite the stimulation of intrinsic GTPase activity leading to RAC inactivation.
Active Rac helps to initiate signaling events, which control the actin cytoskeleton reorganization, cell migration and adhesion [6]. There are also reports implicating the involvement of Rac1 in human cancer. Rac seems to play a key role in the control of malignant transformation and metastatic cascade in various models, including breast cancer cells [7]. Various researchers have postulated a role of Rac in mitogenesis, through the regulation of G1/S transition and cyclin D1 expression [8]. Moreover, Rac overexpression in human breast cancer leads to a higher proliferation rate. Elevated Rac1 GTPase protein is seen in malignant versus benign breast tissues, suggesting that constitutive activation of Rac1 signaling may be present in aggressive breast tumors [9]. Lastly, the importance of Rac in breast cancer tumorigenesis is underscored by the observation that Rac effectors, such as p21-activated kinase 1 and p27, are suppressed in breast cancer cells [10].
Ki67 is a marker of cell proliferation, and many studies have shown a good correlation between grade and Ki67 [11, 12]. Recently, there has been increased interest in assessing Ki67 as a prognostic and/or predictive marker in breast cancer [13]. The development of new genetic tests, such as OncotypeDx, emphasizes the role of proliferative markers, including Ki67, since many of the genes tested reflect the proliferative status of the tumor [14]. Furthermore, in the St. Gallen International Expert Consensus, the panel recommended the use of proliferation markers, such as the Ki67 index, along with traditional parameters, such as stage, histological grade and endocrine status, when choosing the appropriate systemic treatment for early breast cancer [15].
Breast cancer is a very heterogeneous disease, and validated prognostic/predictive biomarkers are in great need. In the present study, we sought to explore the prognostic/predictive significance of RACGAP1 mRNA expression on disease-free survival (DFS) and overall survival (OS) in high-risk operable breast cancer patients. The importance of RACGAP1 as a proliferation or antiproliferation gene was assessed by comparing the prognostic value of RACGAP1 mRNA expression to that of Ki67 protein expression assessed by immunohistochemistry, a known marker of cell proliferation, and to the Nottingham prognostic index (NPI).
Materials and methods
Patient population
This was a retrospective translational research study among 595 patients who had been enrolled in a prospective clinical trial (HE10/97). Accordingly, collection of formalin-fixed paraffin-embedded (FFPE) primary tumor tissue samples was possible in 314 patients only, due to logistical/organizational barriers. The HE10/97 trial randomized 595 high-risk (T1–3N1M0 or T3N0M0) breast cancer patients, between 1997 and 2000, to receive either four cycles of epirubicin (E) followed by four cycles of intensified CMF (cyclophosphamide, methotrexate and 5-fluorouracil) combination chemotherapy (E-CMF) or three cycles of epirubicin followed by three cycles of paclitaxel (T, Taxol®, Bristol Myers-Squibb, Princeton, NJ) and three cycles of intensified CMF (E-T-CMF). The trial was included in the Australian New Zealand Clinical Trials Registry (ANZCTR) and allocated the following Registration Number: ACTRN12611000506998. Chemotherapy cycles were administered every 2 weeks, and patients received granulocyte colony-stimulating factor (G-CSF) support. None of the HER2-positive patients received trastuzumab, since it was not approved for treatment in the adjuvant setting at the time of the study, which has probably influenced DFS and OS in this high-risk group. The present study was approved from the Bioethics Committee of the Aristotle University of Thessaloniki, and patients provided written informed consent prior to enrollment. All participating patients also signed informed consent for research use of their biological material. The results of the HE10/97 study have been previously reported [16]. Primary tumor diameter and axillary nodal status were obtained from the pathology report. NPI was calculated according to Galea et al. [17]. Histological grade was evaluated according to the Scarff, Bloom and Richardson system.
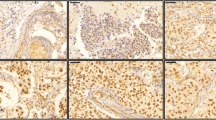
Tissue microarray (TMA) construction
Representative hematoxylin–eosin-stained sections from the tissue blocks were reviewed by a pathologist, and the most representative tumor areas were marked for the construction of the ΤΜΑ blocks, as previously described [18]. Each case was represented by two tissue cores, 1.5 mm in diameter, with each TMA block also containing cores from various neoplastic, non-neoplastic and reactive tissues serving as assay controls. Cases not represented, damaged or inadequate on the TMA sections were recut from the original blocks, and these sections were used for protein and gene analysis.
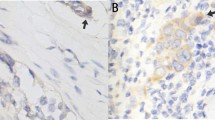
Immunohistochemistry (IHC)
IHC for ER (clone 6F11, Novocastra™, Leica Biosystems, Newcastle, UK), PgR (clone 1A6, Novocastra™, Leica Biosystems), HER2 (A0485 polyclonal antibody, Dako, Glostrup, Denmark) and Ki67 (clone MIB-1, Dako) was performed on serial 2.5-μm-thick TMA sections, using a Bond Max™ autostainer (Leica Microsystems, Wetzlar, Germany), as previously described [18]. All cases were also stained for vimentin (clone V9, Dako) and cytokeratin 8/18 (clone 5D3, Novocastra™, Leica Biosystems), which were used as control stains for tissue immunoreactivity and fixation, as well as identification of tumor cells. Tissue samples negative for the above antibodies were excluded from the study. The evaluation of all IHC sections was done by experienced breast cancer pathologists, blinded as to the patients’ clinical characteristics and survival data.
Interpretation of the IHC results
ER, PgR, HER2 and Ki67 protein expression was evaluated according to established or proposed criteria [19–21]. The ER and PgR immunostaining was scored using the histoscore method. Tissue sections stained for ER/PgR were considered to be positive when ≥1 % of neoplastic cells displayed nuclear immunoreactivity [19]. HER2 protein expression was scored according to the recent guideline recommendations (scores 0–3+) [20]. HER2 was considered to be positive in cases with an IHC score of 3+ (uniform, intense membrane staining in >30 % of invasive tumor cells). Ki67 scores were defined as the number of immunostained cells (nuclear staining) divided by the total number of cells in the evaluated area. For protein expression of Ki67, 14 % was used as cutoff to categorize low (<14 %) and high (≥14 %) protein expression, according to Cheang et al. [21].
Fluorescence in situ hybridization (FISH)
TMA sections or whole tissue sections (5 μm thick) were used for FISH analysis, using the ZytoLight® SPEC HER2/TOP2A/CEN17 triple-color probe (ZytoVision, Bremerhaven, Germany), as previously described [22]. Four carcinoma cell lines (MDA-MB-231, MDA-MB-175, MDA-MB-453 and SK-BR-3) from the Oracle HER2 Control Slide (Leica Biosystems), with a known HER2 gene status, were also used as a control of the FISH assays and analyzed for HER2 genomic status. TOP2A gene amplification was not evaluated for the purpose of the present study.
For the evaluation of the HER2 gene status, non-overlapping nuclei from the invasive part of the tumor were randomly selected and scored. The virtual slides of HER2, ER or PgR stains were used for selecting the invasive part of the tumor in each TMA. The virtual slides were created as previously described [23]. Twenty tumor nuclei were counted according to Press et al. [24]. The HER2 gene was considered to be amplified when the ratio of the gene probe/centromere probe was ≥2.2 [20], or the HER2 copy number was >6 [25]. In cases with values at or near the cutoff (1.8–2.2), additional 20 or 40 nuclei were counted and the ratio was recalculated. In cases with a borderline ratio at 60 nuclei, additional FISH assays were performed in whole sections. HER2 was considered to be positive if it was amplified (ratio ≥2.2 or copy number >6) by FISH, and/or a HER2 score of 3+ was obtained by IHC.
RNA isolation from FFPE tissue and quantitative reverse transcription-polymerase chain reaction (qRT-PCR) assessment
Hematoxylin–eosin sections from all available FFPE tissue specimens were evaluated histologically by a certified pathologist who recorded percentage of tumor cell content in each one. Prior to RNA isolation, macrodissection of tumor areas was performed in most of the FFPE sections with <50 % tumor cell content. The tumor cell content was >30 % in practically all (97 %) of the samples and >50 % in the majority (76 %) of the samples. More than one FFPE section was used for RNA extraction when the tumor surface of a given sample was less than 0.25 cm2.
Sufficient RNA was isolated from 314 FFPE specimens followed by qRT-PCR, as previously described [26]. From each FFPE section or macrodissected tissue fragments (10 μm thick), RNA was isolated using a standardized fully automated isolation method for total RNA from FFPE tissue, based on silica-coated magnetic beads (VERSANT Tissue Preparation Reagents, Siemens Healthcare Diagnostics, Tarrytown, NY) in combination with a liquid handling robot, as previously described in detail [27]. The method involves extraction-integrated deparaffinization and DNase I digestion steps. DNA-free total RNA was eluted with 100 μL elution buffer and stored in −80 °C.
One-step qRT-PCR was applied for the relative quantification of RACGAP1 mRNA expression, by using gene-specific TaqMan®-based assays. Forty cycles of nucleic acid amplification were applied, and the cycle threshold (CT) values of the target gene were identified. CT values were normalized by subtracting the CT value of the housekeeping gene RPL37A (ribosomal protein L37a) from the CT value of the target gene (ΔCT). RNA results were then reported as 40–ΔCT values, which correlate proportionally to the mRNA expression level of the target gene. For assessment of DNA contamination, a qPCR analysis specific to the PAEP gene (progestagen-associated endometrial protein) was performed, without the preceding reverse transcription step. Samples were considered to be substantially free of DNA when CT values above 38 were detected. In case of DNA contamination, samples were manually re-digested with DNase I. The quantity of RNA following isolation (yield) was checked by measuring RPL37A expression as a surrogate marker for amplifiable mRNA. Samples with average RPL37A CT values <32 were considered to have sufficient RNA and were eligible for analysis.
Expression of the target gene, as well as the reference gene RPL37A, was assessed in triplicate by qRT-PCR using the SuperScript III PLATINUM One-Step Quantitative RT-PCR System with ROX (Invitrogen, Karlsruhe, Germany) in an ABI PRISM 7900HT (Applied Biosystems, Darmstadt, Germany) [28]. The lengths of the amplicons detected by the RACGAP1 and RPL37A assays were 86 and 65 bp, respectively, with PCR efficiencies [E = 1(10-slope)] of 98.5 and 86.0 %, respectively. A commercially available human reference RNA (Stratagene qPCR Human Reference Total RNA, Agilent Technologies, Waldbronn, Germany) was used as positive control. No-template controls were assessed in parallel to exclude contamination.
The Primer/Probe (FAM/TAMRA-labeled) sets used for amplification of the target and reference genes were the following (5′–>3′):
-
RACGAP1 Probe ACTGAGAATCTCCACCCGGCGCA (antisense)
-
Forward Primer GAATGTGCGGAATCTGTTTGAG
-
Reverse Primer TCGCCAACTGGATAAATTGGA
-
-
RPL37A Probe TGGCTGGCGGTGCCTGGA
-
Forward Primer TGTGGTTCCTGCATGAAGACA
-
Reverse Primer GTGACAGCGGAAGTGGTATTGTAC
-
Statistical methodology
Categorical data are presented as counts and corresponding percentages, while continuous data are presented as medians and ranges. The prognostic value of mRNA expression for the RACGAP1 gene was examined in terms of OS and DFS in the quartiles of the mRNA distribution as possible thresholds. In case a cutoff had prognostic significance, it was used to dichotomize tumor expression into low and high. Relationships between RACGAP1 groups and other parameters were determined by using the nonparametric Mann–Whitney test if continuous and the Pearson chi-square test or Fisher’s exact test if discrete.
OS was measured from the date of randomization until death from any cause. Surviving patients were censored at the date of last contact. DFS was measured from the date of randomization until recurrence of tumor or secondary neoplasm or death from any cause [29]. Time-to-event distributions were estimated using Kaplan–Meier curves and compared using log-rank tests.
Univariate Cox’s proportional hazard regression analyses, adjusted for treatment, were performed for RACGAP1 mRNA expression, Ki67 protein expression and NPI score values to assess prognostic significance on OS and DFS. Predictive significance of RACGAP1 mRNA expression was examined by interaction tests between RACGAP1 and treatment group using Cox regression models. In multivariate analysis, a backward selection procedure with a removal criterion p > 0.10 based on likelihood ratio test was performed in order to identify significant clinicopathological variables among the following: age, treatment group (E-T-CMF vs. E-CMF), menopausal status (pre vs. post), histological grade (I–II vs. III–undifferentiated), Ki67 protein expression (low vs. high), NPI score values (as a continuous variable), tumor size (≤2 cm vs. 2–5 cm vs. >5 cm), number of positive axillary nodes (0–3 vs. ≥4), ER/PgR status (negative vs. positive), HER2 status (negative vs. positive), adjuvant hormone therapy (yes vs. no), adjuvant radiotherapy (yes vs. no), type of operation (modified radical mastectomy vs. breast-conserving surgery) and time interval from breast surgery (<2 weeks vs. 2–4 weeks vs. >4 weeks). Treatment group (E-T-CMF vs. E-CMF) and RACGAP1 mRNA expression (binary or continuous) were kept in the final model, in order to examine whether RACGAP1 added independent prognostic information in the presence of treatment and significant clinicopathological parameters.
Results of this study were presented according to reporting recommendations for tumor marker prognostic studies [30]. The design of the study is prospective-retrospective as described in Simon et al. [31]. The SPSS software was used for statistical analysis (SPSS for Windows, version 15.0, SPSS Inc.).
Results
Basic patient and tumor characteristics
For the entire patient population, the median age was 50 years (range 22–78 years). The majority of patients were ER/PgR positive (80 % of the 270 tumors centrally assessed by IHC), premenopausal (54 %), had undergone radical mastectomy (79 %) and had received adjuvant RT (82 %) and adjuvant hormonal therapy (92 %). Most tumors were T2 (53 %), grade I–II (50 %), HER2 negative (73 % of the 250 tumors centrally assessed by IHC and FISH) and had four or more axillary lymph nodes (76 %). Of the 273 patients assessed centrally by IHC for Ki67, 227 (83 %) were found to have high protein expression (≥14 % of cells were positively stained). One hundred and seventy patients and 144 patients were randomized in the E-CMF arm and the E-T-CMF arm, respectively. The two groups were well balanced for patient and tumor characteristics (Table 1), except for NPI score (p = 0.033) and histological grade (p = 0.013). This imbalance in histological grade was also reported in the clinical paper [16]. In addition, there were no significant differences in basic clinicopathological characteristics between the patients included in the present study and the rest of the HE10/97 randomized patients, for which tissue samples were not available, except for decreased number of nodes removed (Mann–Whitney test, p = 0.002) and administration of adjuvant RT (Fisher’s exact test, p = 0.014) in the patients studied.
Normalized mRNA expression of RACGAP1
Results for RACGAP1 mRNA expression were available in 314 patients. The distribution of the normalized mRNA values of RACGAP1 had a range between 29.4 and 35.6 (Fig. 1). The median value was 32.9, while the 25th and 75th percentiles were 32.2 and 33.7, respectively. No bimodal distribution of RACGAP1 mRNA expression was evident in Fig. 1 that would indicate the existence of a natural cutoff. Both the median and the 25th percentile of RACGAP1 mRNA expression were found to be significant cutoffs in terms of OS and DFS, while the 75th percentile was not. The median was used in the primary analysis on associations and comparisons presented in the following sections. However, the prognostic/predictive value of continuous RACGAP1 mRNA expression values and values above the 25th percentile were examined as well, in univariate and multivariate Cox regression analyses.
Association of RACGAP1 mRNA expression with clinicopathological parameters
The associations of RACGAP1 mRNA expression with selected patient and tumor characteristics are shown in Table 2. High RACGAP1 mRNA expression (above the median) was significantly associated with high NPI score values (Mann–Whitney test, p = 0.007). RACGAP1 mRNA expression was significantly associated with histological grade (p = 0.002). Specifically, 59 % of the high RACGAP1 tumors were of high grade versus 41 % among the low RACGAP1 tumors (Fisher’s exact test, p = 0.002). Finally, there was a significant association between RACGAP1 and Ki67 protein expression (Fisher’s exact test, p = 0.002). Seventy-six percent among the low-RACGAP1-expressing tumors had high Ki67 protein expression, in comparison with 90 % among the high-RACGAP1-expressing tumors.
Prognostic/predictive value of RACGAP1 mRNA expression
After a median follow-up of 8 years, 5- and 7-year overall survival rates were 84 and 78 %, respectively. There were 80 deaths (25.5 %) in a range of 12–111 months. The 5- and 7-year DFS were 71 and 66 %, respectively. One hundred and ten patients had disease progression, and five patients had a second malignancy and/or death without documented progression.
Using the 50th percentile in the distribution of RACGAP1 mRNA expression values as a cutoff allowed us to distinguish two populations of significantly different prognosis, as stated above. High expression of RACGAP1 (above the median) was significantly associated with reduced OS (log-rank, p < 0.001) and DFS (log-rank, p = 0.002). More specifically, 54 deaths (34 %) and 67 relapses (43 %) occurred in the high RACGAP1 group of patients versus 26 deaths (17 %) and 43 documented relapses (27 %) in the low RACGAP1 group. Kaplan–Meier curves representing the probability of survival and DFS according to RACGAP1 mRNA expression are presented in Fig. 2. Five-year OS and DFS rates were 92 and 79 % in the low-RACGAP1-expressing tumors versus 76 and 63 % in the high-RACGAP1-expressing tumors, respectively. Univariate Cox regression analysis, adjusted for treatment, showed an increased risk for death in patients with high RACGAP1 mRNA expression (hazard ratio [HR] = 2.48, 95 % confidence interval [CI] 1.55–3.95, Wald’s p < 0.001), as well as an increased risk for relapse (HR = 1.78, 95 % CI 1.22–2.58, p = 0.003). However, RACGAP1 mRNA expression was not predictive for benefit from adjuvant treatment with paclitaxel (tests for interaction, p = 0.43 for OS and p = 0.68 for DFS). Moreover, when we examined the prognostic value of continuous RACGAP1 mRNA values, we found that increasing RACGAP1 mRNA levels were also prognostic for worse OS (HR = 1.46, 95 % CI 1.19–1.80, Wald’s p < 0.001) and DFS (HR = 1.29, 95 % CI 1.09–1.53, p = 0.004). Examining the prognostic value of RACGAP1 mRNA expression values above the 25th percentile in univariate analysis resulted in similarly increased risk for death (HR = 3.11, 95 % CI 1.55–6.22, Wald’s p = 0.001) and relapse (HR = 1.91, 95 % CI 1.18–3.10, p = 0.009).
High Ki67 protein expression was significantly associated with increased risk for death (HR = 2.53, 95 % CI 1.09–5.86, Wald’s p = 0.030) and marginally associated with increased risk for relapse (HR = 1.75, 95 % CI 0.95–3.21, p = 0.071). Finally, increasing NPI score values were associated with worse DFS and OS (HR = 1.68, 95 % CI 1.34–2.11, p < 0.001 and HR = 1.73, 95 % CI 1.31–2.28, p < 0.001, respectively).
Multivariate analysis
Multivariate Cox regression analysis (Table 3) revealed that RACGAP1 mRNA expression independently predicted OS. More specifically, high RACGAP1 mRNA expression (above the median) was an adverse prognostic factor for death (HR = 2.00, 95 % CI 1.20–3.34, Wald’s p = 0.008). In terms of DFS, RACGAP1 mRNA expression did not retain significance in the multivariate model (HR = 1.33, 95 % CI 0.88–2.02, p = 0.18). Including continuous RACGAP1 mRNA expression values in the multivariate model, RACGAP1 independently predicted OS (HR = 1.45, 95 % CI 1.12–1.87, Wald’s p = 0.005), but not DFS (HR = 1.14, 95 % CI 0.93–1.40, p = 0.20). Similar were the results when RACGAP1 mRNA expression values above the 25th percentile cutoff were included in the multivariate model. High Ki67 protein expression independently predicted OS as well (HR = 3.56, 95 % CI 1.27–9.97, p = 0.016), but not DFS (HR = 1.88, 95 % CI 0.96–3.68, p = 0.067).
Discussion
In the present study, we evaluated the prognostic significance of RACGAP1 mRNA expression in a high-risk group of patients treated with dose-dense sequential chemotherapy. In univariate analysis, we demonstrated that RACGAP1 mRNA levels were inversely correlated with OS and DFS, as patients with high RACGAP1 mRNA expression had increased risk for death and relapse. In addition, high RACGAP1 mRNA expression was significantly associated with higher histological grade, high Ki67 protein expression and high NPI scores. Specifically, high histological grade, high Ki67 protein expression and high NPI score values were more prevalent in high- compared to low-RACGAP1 mRNA-expressing tumors.
The findings of our study appear to contradict a body of evidence suggesting that Rac overexpression in human breast cancer leads to higher proliferation rates and a more aggressive tumor behavior [9]. Schnelzer et al. [32] demonstrated significantly higher Rac1 protein and mRNA levels in breast cancer tissues compared to normal. Specifically, benign breast tissue showed weak Rac1 expression, while ductal in situ carcinoma, primary breast cancer and lymph node metastases had higher expression levels. Additionally, patients with recurrent disease had Rac1 expression at the cytoplasmic membrane, suggesting Rac1 activation in aggressive states of disease [32]. Finally, in cell lines, Rac1-activating mutations appear to cause tumorigenic transformation [33].
RACGAP1, a Rac GTPase-activating protein, is known to stimulate intrinsic GTPase activity leading to Rac inactivation. Based on this effect, high RACGAP1 mRNA expression would be expected to be associated with lower histological grade, low Ki67 protein expression and NPI scores and decreased risk for death and relapse in our patients. Zondag et al. [34], however, have shown the existence of a cross talk between Rho and Rac GTPases. Rac activation leads to the inactivation of Rho, while the downregulation of Rac activity leads to increased Rho activity and epithelial-mesenchymal transition. Therefore, it appears that cell transformation is largely dependent on the balance between Rac and Rho activity and that inactivation of Rac due to high RACGAP1 mRNA expression results in increased Rho activity, leading to cell cycle progression by suppressing Ras-mediated induction of the cyclin-dependent kinase inhibitor p21Waf1/Cip1 [35].
In agreement with the above notion, RACGAP1 seems to contribute to the regulation of numerous biological processes, including gene transcription, cytoskeletal organization and cell proliferation and transformation. It also appears to play a key role in cellular motility and metastasis [36]. Moreover, Fritz et al. also showed that Rho GTPases are related to prognostic markers, such as histological grade and proliferation index. They demonstrated that levels of Rho GTPases increase with histological grade and the proliferation index (MIB-1) of the tumors. Interestingly, high Rac1 expression was associated with grade I and II but not grade III tumors, pointing out that Rac function might be important in the early stages of tumor progression [9]. Consistent with the above data, our study showed a strong association of high RACGAP1 mRNA expression with high histological grade, pointing out the important role of RACGAP function in early breast cancer. Conversely, our study showed a statistically significant difference of RACGAP1 mRNA expression between low-to-intermediate and high-grade tumors, suggesting that high RACGAP1 mRNA levels could reflect increased aggressiveness of the tumor.
RACGAP1 mRNA and Ki67 protein expression were shown to be stronger prognostic indicators than the NPI score, since they independently predicted risk for death in the multivariate analysis. Furthermore, this analysis showed similar results in terms of OS and DFS between the two treatment groups, suggesting that the addition of paclitaxel provided no benefit in this high-risk group of patients and that RACGAP1 mRNA expression was not predictive for benefit from adjuvant treatment with paclitaxel.
Conclusively, our study is the first to associate RACGAP1 mRNA expression in early high-risk breast cancer patients with disease outcome, highlighting the important role of Rho/Rac signaling in breast cancer cell proliferation and tumor behavior and suggesting a role for RACGAP1 as a potentially important prognostic biomarker. The utility of RACGAP1 mRNA expression, assessed in FFPE tumor tissue samples by qRT-PCR, in patient selection for treatment with aggressive chemotherapy regimens should be further explored and validated in larger cohorts.
References
Early Breast Cancer Trialists’Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365:1687–1717
Lee AH, Pinder SE, Macmillan RD, Mitchell M, Ellis IO, Elston CW, Blamey RW (2006) Prognostic value of lymphovascular invasion in women with lymph node negative invasive breast carcinoma. Eur J Cancer 42:357–362
Brenton JD, Carey LA, Ahmed AA, Caldas C (2005) Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol 23:7350–7360
Mackay DJ, Hall A (1998) Rho GTPases. J Biol Chem 273(33):20685–20688
Zhao WM, Fang G (2005) MgcRacGAP controls the assembly of the contractile ring and the initiation of cytokinesis. Proc Natl Acad Sci USA 102:13158–13163
Evers EE, Zondag GM, Malliri A, Price LS, ten Klooster JP, van der Kammen RA, Collard JG (2000) Rho family of proteins in cell adhesion and cell migration. Eur J Cancer 36:1269–1274
Tang Y, Olyfemi L, Wang MT, Nie D (2008) Role of Rho GTPases in breast cancer. Frontiers Biosc 13:759–776
Welsh CF (2004) Rho GTPases as key transducers of proliferative signals in G1 cell cycle regulation. Breast Cancer Res Treat 84:33–42
Fritz G, Brachetti C, Bahlmann F, Schmidt M, Kaina B (2002) Rho GTPases in human breast tumors: expression and mutation analyses and correlation with clinical parameters. Br J Cancer 87:635–644
Bohmer RM, Scharf E, Assoian RK (1996) Cytoskeletal integrity is required throughout the mitogen stimulation phase of the cell cycle and mediates the anchorage-dependent expression of cyclin D1. Mol Biol Cell 7:101–111
Barbareschi M, Girlando S, Mauri FM, Forti S, Eccher C, Mauri FA, Togni R, Dalla Palma P, Doglioni C (1994) Quantitative growth fraction evaluation with MIB1 and Ki67 antibodies in breast carcinomas. Am J Clin Pathol 102:171–175
Kennedy JC, El-Badawy N, DeRose PB, Cohen C (1992) Comparison of cell proliferation in breast carcinoma using image analysis (Ki67) and flow cytometric systems. Anal Quant Cytol Histol 14:304–311
Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, Somerfield MR, Hayes DF, Bast RC Jr (2007) American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 25:5287–5312
Oakman C, Bessi S, Zafarana E, Galardi F, Biganzoli L, Di Leo A (2009) Recent advances in systemic therapy: new diagnostics and biological predictors of outcome in early breast cancer. Breast Cancer Res 11:205
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ (2011) Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747
Fountzilas G, Skarlos D, Dafni U, Gogas H, Briasoulis E, Pectasides D, Papadimitriou C, Markopoulos C, Polychronis A, Kalofonos HP, Siafaka V, Kosmidis P, Timotheadou E, Tsavdaridis D, Bafaloukos D, Papakostas P, Razis E, Makrantonakis P, Aravantinos G, Christodoulou C, Dimopoulos AM (2005) Postoperative dose-dense sequential chemotherapy with epirubicin, followed by CMF with or without paclitaxel, in patients with high-risk operable breast cancer: a randomized phase III study conducted by the Hellenic Cooperative Oncology Group. Ann Oncol 16:1762–1771
Galea MH, Blamey RW, Elston CH, Ellis IO (1992) The Nottingham prognostic index in primary breast cancer. Breast Cancer Res Treat 22:207–219
Skarlos P, Christodoulou C, Kalogeras KT, Eleftheraki AG, Bobos M, Batistatou A, Valavanis C, Tzaida O, Timotheadou E, Kronenwett R, Wirtz RM, Kostopoulos I, Televantou D, Koutselini E, Papaspirou I, Papadimitriou CA, Pectasides D, Gogas H, Aravantinos G, Pavlidis N, Arapantoni P, Skarlos DV, Fountzilas G (2012) Triple negative phenotype is of adverse prognostic value in patients treated with dose-dense sequential adjuvant chemotherapy: a translational research analysis in the context of a Hellenic Cooperative Oncology Group (HeCOG) randomized phase III trial. Cancer Chemother Prarmacol 69:533–546
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FC, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28:2784–2795
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 25:118–145
Cheang MCU, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS, Perou CM, Ellis MJ, Nielsen TO (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750
Psyrri A, Kalogeras KT, Kronenwett R, Wirtz RM, Batistatou A, Bournakis E, Timotheadou E, Gogas H, Aravantinos G, Christodoulou C, Makatsoris T, Linardou H, Pectasides D, Pavlidis N, Economopoulos T, Fountzilas G (2012) Prognostic significance of UBE2C mRNA expression in high-risk early breast cancer. A Hellenic Cooperative Oncology Group (HeCOG) Study. Ann Oncol 23:1422–1427
Fountzilas G, Ciuleanu E, Bobos M, Kalogera-Fountzila A, Eleftheraki AG, Karayannopoulou G, Zaramboukas T, Nikolaou A, Markou K, Resiga L, Dionysopoulos D, Samantas E, Athanassiou H, Misailidou D, Skarlos D, Ciuleanu T (2012) Induction chemotherapy followed by concomitant radiotherapy and weekly cisplatin versus the same concomitant chemoradiotherapy in patients with nasopharyngeal carcinoma: a randomized phase II study conducted by the Hellenic Cooperative Oncology Group (HeCOG) with biomarker evaluation. Ann Oncol 23:427–435
Press MF, Sauter G, Buyse M, Bernstein L, Guzman R, Santiago A, Villalobos IE, Eiermann W, Pienkowski T, Martin M, Robert N, Crown J, Bee V, Taupin H, Flom KJ, Tabah-Fisch I, Pauletti G, Lindsay MA, Riva A, Slamon DJ (2011) Alteration of topoisomerase II-alpha gene in human breast cancer: association with responsiveness to anthracycline-based chemotherapy. J Clin Oncol 29:859–867
Van den Bempt I, Van Loo P, Drijkoningen M, Neven P, Smeets A, Christiaens MR, Paridaens R, De Wolf-Peeters C (2008) Polysomy 17 in breast cancer: clinicopathologic significance and impact on HER-2 testing. J Clin Oncol 26:4869–4874
Pentheroudakis G, Batistatou A, Kalogeras KT, Kronenwett R, Wirtz RM, Bournakis E, Eleftheraki AG, Pectasides D, Bobos M, Papaspirou I, Kamina S, Gogas H, Koutras AK, Pavlidis N, Fountzilas G (2011) Prognostic utility of β-tubulin isotype III and correlations with other molecular and clinicopathological variables in patients with early breast cancer: a translational Hellenic Cooperative Oncology Group (HeCOG) study. Breast Cancer Res Treat 127:179–193
Bohmann K, Hennig G, Rogel U, Poremba C, Mueller BM, Fritz P, Stoerkel S, Schaefer KL (2009) RNA extraction from archival formalin-fixed paraffin-embedded tissue: a comparison of manual, semiautomated, and fully automated purification methods. Clin Chem 55:1719–1727
Mueller BM, Kronenwett R, Hennig G, Euting H, Weber K, Bohmann K, Weichert W, Altmann G, Roth C, Winzer KJ, Kristiansen G, Petry C, Dietel M, Denkert C (2011) Quantitative determination of estrogen receptor, progesterone receptor and HER2 mRNA in formalin-fixed paraffin-embedded tissue—a new option for predictive biomarker assessment in breast cancer. Diagn Mol Pathol 20:1–10
Hudis CA, Barlow WE, Costantino JP, Gray RJ, Pritchard KI, Chapman JA, Sparano JA, Hunsberger S, Enos RA, Gelber RD, Zujewski JA (2007) Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol 25:2127–2132
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) Reporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235
Simon RM, Paik S, Hayes DF (2009) Use of archived specimens in evaluation of prognostic and predictive biomarkers. J Natl Cancer Inst 101:1446–1452
Schnelzer A, Prechterl D, Knaus U, Dehne K, Gerhard M, Graeff H, Harbeck N, Schmitt M, Lengyel E (2000) Rac1 in human breast cancer: overexpression, mutation analysis, and characterization of a new isoform, Rac1b. Oncogene 19:3013–3020
Bouzahzah B, Albanese C, Ahmed F, Pixley F, Lisanti MP, Segall JD, Condeelis J, Joyce D, Minden A, Der CJ, Chan A, Symons M, Pestell RG (2001) Rho family GTPases regulate mammary epithelium cell growth and metastasis through distinguishable pathways. Mol Med 7:815–830
Zondag GCM, Evers EE, ten Klooster JP, Janssen L, van der Kammen RA, Collard JG (2000) Oncogenic Ras downregulates Rac activity which leads to increased Rho activity and epithelial-mesenchymal transition. J Cell Biol 149:775–781
Olson MF, Paterson HF, Marshall CJ (1998) Signals from Ras and Rho GTPases interact to regulate expression of p21Waf1/Cip1. Nature 394:295–299
Lin M, Van Colen KL (2004) Rho-regulatory proteins in breast cancer cell motility and invasion. Breast Cancer Res Treat 84:49–60
Acknowledgments
The authors wish to thank Evita Fragou and Dimitra Katsala for monitoring the study, Maria Moschoni for coordinating the data management and Thalia Spinari for tissue sample collection. Translational research was supported by a HeCOG research grant: HE TRANS_BR. The senior investigator (GF) has received Commercial Research Funding by Roche Hellas SA and Genesis Pharma SA, Athens, Greece.
Conflict of interest
On behalf of the Hellenic Foundation for Cancer Research, Athens, Greece, the senior author (GF) has pending patent applications with Siemens Healthcare Diagnostics, Tarrytown, NY. The third and fourth authors (RK and RMW) are both employed by companies that are developing and selling diagnostic test systems. The rest of the authors have declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Pliarchopoulou and K. T. Kalogeras contributed equally to this work.
Rights and permissions
About this article
Cite this article
Pliarchopoulou, K., Kalogeras, K.T., Kronenwett, R. et al. Prognostic significance of RACGAP1 mRNA expression in high-risk early breast cancer: a study in primary tumors of breast cancer patients participating in a randomized Hellenic Cooperative Oncology Group trial. Cancer Chemother Pharmacol 71, 245–255 (2013). https://doi.org/10.1007/s00280-012-2002-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-012-2002-z