Abstract
Purpose
The aim of this study was to determine the expression of molecular markers in metastatic colorectal cancer (mCRC) and the concordance between primary tumor and metastasis. We also aimed to determine the relationship between molecular markers and clinical outcomes of cetuximab-containing chemotherapy.
Methods
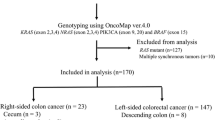
Seventy-five mCRC patients who received cetuximab-containing chemotherapy between 2000 and 2008 were consecutively enrolled. EGFR, p-EGFR, PTEN, and IGF-1R expression by immunohistochemistry, DNA sequencing for EGFR, KRAS, BRAF, and PI3 KCA, and EGFR amplification by FISH were done.
Results
The positive expression of EGFR, p-EGFR, PTEN, and IGF-1R was determined in 45 (64.3%), 9 (14.8%), 35 (50.7%), and 10 patients (16.1%), respectively. EGFR gene amplification or high polysomy was detected in 10 patients (17.6%). KRAS mutation and BRAF mutation were detected in 19 patients (27.5%) and five patients (7.0%), respectively. Among tested biomarkers, only the EGFR intron 1 CA repeat polymorphism and BRAF mutation showed concordance (kappa = 0.600, P = 0.003; and kappa = 0.692, P = 0.001, respectively) between primary tumor and paired metastasis. Skin rash was a strong predictive marker for response rate, PFS, and OS. In KRAS mutant tumors, PTEN expression was associated with a longer PFS. BRAF mutation was related to poor outcome in KRAS wild-type tumors.
Conclusions
BRAF mutations and EGFR intron 1 CA repeat polymorphisms were concordant between primary tumors and paired metastases. In KRAS mutant tumors, PTEN expression was a predictive marker for favorable outcomes. In KRAS wild type, BRAF mutation was strong predictive markers for poor outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since cetuximab was introduced for the treatment of mCRC, there have been many studies aimed at identifying the predictive markers for chemotherapeutic responsiveness. Several studies have shown, by immunohistochemistry (IHC), that EGFR protein expression in cancer tissues does not predict the response to cetuximab treatment [1]. In contrast, a gain in the EGFR gene copy number due to polysomy or gene amplification, which has been evaluated by fluorescent in situ hybridization (FISH), seems to be a better predictive marker for response to anti-EGFR therapy [2, 3]. KRAS mutation and PTEN loss by IHC are well known as predictive markers for poor outcome to cetuximab treatment [4]. BRAF and PIK3CA mutations are considered to predict a poor response to cetuximab treatment [5, 6].
IGF1R results in upregulation in the majority of CRCs, most likely contributing to the aggressive growth characteristics of the tumor and poor prognosis [7, 8]. Retrospective data suggest that overexpression of IGF1R is a potential predictive factor for cetuximab treatment [9].
The number of CA single sequence repeats in intron 1 of the EGFR gene, which affects the transcription efficiency of the gene, is associated with the response to EGFR antibodies. Several data suggest a correlation between polymorphic variations in intron 1 of the EGFR gene and the response to EGFR inhibitors [10].
Most of these data were obtained by analyzing the clinical outcomes and molecular features in primary tumors. It is possible, however, that primary tumors and paired metastatic lesions might be different with respect to molecular marker expression or gene status and that these differences may affect the clinical significance of a predictive test. Few data exist regarding the concordance of expression of molecular markers between primary sites and paired metastases. Furthermore, little is known about predictive molecular markers for cetuximab treatment in Eastern countries.
We conducted this study to determine the variable expression of molecular markers that could affect the response to cetuximab treatment in Eastern countries and to determine whether or not the status of molecular markers between primary tumors and paired metastases is concordant. We also determined the predictive markers for cetuximab treatment.
Patients and methods
We consecutively enrolled CRC patients who underwent cetuximab-containing palliative chemotherapy at Seoul National University Hospital between 2000 and 2008, and from whom tumor tissue specimens were available.
All patients were treated with cetuximab with or without combined cytotoxic chemotherapy. The initial cetuximab dose was 400 mg/m2, followed by 250 mg/m2 every week. Treatment was continued until disease progression (PD), intolerable toxicity, or patient refusal.
Clinical evaluation and response criteria
The response was evaluated every 6 weeks with computed tomography according to response evaluation criteria in solid tumors (RECIST). The patients who had a complete response (CR) or partial response (PR) were defined as responders. The disease control rate reflects the proportion of the patients who had a CR, PR, and stable disease (SD).
Molecular analysis
Paraffin-embedded tumor specimens were used to construct a tissue microarray with 2-mm-diameter cores in tissues which were operative specimens. In biopsy specimens, all tissues were used. Genomic DNA was extracted using the QIAamp Mini Kit (Qiagen, Chatsworth, CA, USA), according to the manufacturer’s instructions. For patients with tissues from primary tumors and corresponding metastases, the sample from the primary lesion was used to represent the patient in the correlative analyses with a clinical outcome.
Immunohistochemistry
Immunohistochemistry (IHC) was performed on a Leica Bond-max automated immunostainer (Leica Microsystems, Newcastle, UK) following the manufacturer’s protocols.
The following antibodies were used: EGFR (clone 31G7; Zymed, San Francisco, CA, USA), p-EGFR (clone 1H12; Cell Signaling, Beverly, MA, USA), PTEN (clone 6H2.1; Dako, Glostrup, Denmark), and IGFIR (β subunit; Cell Signaling). Antibody binding was detected using the Bond Polymer Refine Detection kit (Leica Microsystems).
Interpretation of IHC
EGFR was assessed according to the EGFR pharmDx™ scoring guidelines. PTEN staining was mainly cytoplasmatic. The intensity was scored according to a four-tier system, as follows: 0, no staining; 1, weak; 2, moderate; and 3, strong. We assigned 1, 2, or 3 additional points if the percentage of positive cells was <25, 25–50, or >50%, respectively. Specimens were defined as positive if the score was ≥4 [11].
To detect tyrosine phosphorylation of EGFR, only membranous staining was considered positive for EGFR. A cut-off value of 10% positive cells with an intensity >2 was defined as a positive expression of EGFR [12].
The staining of IGF1R protein (membranous and/or cytoplasmic) was also semi-quantitatively defined as a positive expression based on >10% positive tumor cells with >2 intensity.
EGFR FISH
FISH assays were carried out in 2-mm cores in tissue microarrays containing representative malignant cells. The EGFR FISH assay was performed with the LSI EGFR SpectrumOrange/CEP 7 SpectrumGreen probe (Vysis/Abbott Molecular, Des Plaines, IL, USA), according to methods described elsewhere [13]. Four physically distant tumor areas were selected on the H&E-stained slides, and the EGFR and CEP7 signals were counted in at least 100 nuclei per tumor area at 1,000× magnification.
EGFR gene polymorphisms
Fifty nanograms of DNA was amplified in a 20-μl reaction solution containing 10 μl of 2X concentrated HotStarTaq Master Mix (Qiagen, Hilden, Germany), including polymerase chain reaction (PCR) buffer with 3 mM MgCl2, 400 μM each dNTP, and 0.3 μM of each primer pairs. The primer sequences specific for microsatellite marker in EGFR intron 1 were as follows: 5′-FAM-labeled forward EGFR primer; 5′-TGAAGAATTTGAGCCAACCAAA-3′ and unlabeled reverse EGFR primer; 5′-CACTTGAACCAGGGACAGCA-3′. The number of CA dinucleotide repeats of the PCR products was resolved on the GeneMapper Software v3.7. PCR product from A431 was used to confirm the number of CA dinucleotide repeats.
KRAS, BRAF, and PI3KCA mutations
We searched for KRAS point mutations in codons 12 and 13, two hotspots that cumulatively include >95% of mutations in this gene [14]. BRAF mutations were investigated in exon 15, in which >95% of BRAF point mutations occur [15]. Exons 9 and 20 of the alpha polypeptide (the catalytic subunit of the PI3K protein [PI3KCA]), which are frequently mutated in CRC, were amplified using a standard PCR protocol, and previously described primers.
Statistical analyses
The association between primary tumors and paired metastatic sites for IHC, EGFR gene status, EGFR intron 1 CA repeat number, and mutational status of KRAS, BRAF, and PI3KCA was evaluated by means of the Cohen’s k test, appropriate for the assessment of the concordance between two categorical measurements of the same individual. A moderate and good agreement was defined as a coefficient of 0.41 ≤ κ ≤ 0.60 and 0.61 ≤ κ ≤ 0.80, respectively.
The statistical analyses of categorical variables were performed using Pearson’s χ2 test or Fisher’s exact test. Comparison of the mean between groups was calculated by Student’s t test. The median duration of progression-free survival (PFS) and overall survival (OS) was calculated using the Kaplan–Meier method. Comparisons between different groups were made using the log-rank tests. Multivariate analyses were performed using a logistic regression model for response and Cox regression model for PFS and OS to identify independent factors and adjust for baseline characteristics. Two-sided P values of <0.05 were considered significant. All analyses were performed using SPSS for Windows, version 17.0 (SPSS Inc., Chicago, IL, USA).
This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No: H-0808-031-253).
Results
Patient characteristics and efficacy
The patient characteristics are summarized in Table 1.
The median number of metastatic sites before starting treatment was 2 (range, 1–6). The most common metastatic site in these patients was the liver (52 patients [69.3%]). Thirty-five (46.7%), 36 (48%), and 24 (32%) patients had lung, lymph node, and peritoneum metastasis, respectively. All but three patients (4%) received cetuximab-containing chemotherapy as a second-line or greater treatment. In 75 patients, the number of available tissues was 97, and primary tumor only was available in 38 patients, whereas metastatic tissue only was available in 15 patients. In 22 patients, we obtained primary tumors and paired metastases.
Response was evaluable in 64 patients (85.3%). We observed 11 PRs, 27 SDs, and 26 instances of progressive disease (PD). Therefore, the overall response rate (RR) was 17.2% (95% CI, 7.7–26.7), and the disease control rate was 59.4% (95% CI, 47.0–71.7). The median duration of follow-up was 197 days (range, 16–1,022 days).
During treatment, a skin rash developed in 38 patients (50.7%). Grades 1, 2, and 3 skin toxicity were observed in 19 (25.3%), 15 (20%), and four patients (5.3%), respectively. Median PFS and OS were 122 days (95% CI, 82–161) and 246 days (95% CI, 158–333).
Results of molecular characteristics
The molecular characteristics are shown in Table 2.
Among 57 patients who were evaluated by FISH, EGFR gene amplification and high polysomy was observed in 5 (8.8%) and five patients (8.8%), respectively.
Sixty-eight patients were assessable for the EGFR intron 1 CA repeat polymorphism. The median sum of both alleles was 39 (range, 29–48). We defined low and high CA repeats as those presenting the sum of both allele ≤36 and ≥37. Twenty-three patients (33.3%) showed a low CA repeat, whereas 46 (66.7%) had a high repeat.
A KRAS mutation was found in the tumor from 19 patients (27.5%) in codon 12 (14 patients) or codon 13 (five patients). A BRAF V600E mutation was observed in tumors of five patients (7.0%), and a PI3KCA mutation was detected in 1 of 57 patients (1.8%).
Concordance between primary tumors and paired metastases
The concordance of molecular markers between primary tumors and paired metastases is summarized in Table 3. A BRAF mutation tested on primary tissues was concordant with the results of metastases (kappa = 0.692; good strength of agreement, P = 0.001). The EGFR intron 1 CA repeat number showed concordant expression (kappa = 0.600, moderate strength of agreement, P = 0.003). While a KRAS mutation between primary tumors and metastases did not show statistically significant concordance (95% CI, kappa = 0.433, P = 0.074), KRAS mutations had a tendency toward concordant expression. Other markers were discordant.
Comparison of characteristics between KRAS wild types and mutants
We identified 19 KRAS mutant tumors and 50 KRAS WTs. There were no differences in expression of EGFR, P-EGFR positivity, PTEN positive rate, and EGFR gene amplification and high polysomy.
In KRAS WT patients, IGF-1R expression was lower (5, 11.6%) than KRAS mutants (5, 31.2%, P = 0.074). Even though there were no BRAF mutations in KRAS mutants, it was not statistically significant (P = 0.311; Table 4).
We detected 10 PRs (23.8%) and 1 PR (5.9%) in KRAS WTs and mutants (P = 0.151), respectively. The median PFS of KRAS WTs and mutants was 123 (95% CI, 25–220) and 121 days (95% CI, 70–175; P = 0.298), respectively. The median OS in KRAS WTs and mutants was 246 (95% CI, 174–317) and 258 days (95% CI, 125–390; P = 0.809), respectively.
Predictive markers for treatment outcomes in KRAS WT tumors
Among 50 patients with KRAS WT tumors, responses were evaluable in 42 patients, showing a response rate of 23.8% (95% CI, 10.4–37.2%), and the disease control rate was 59.5% (95% CI, 44.0–75.0%). The first- and second-line treatment compared to greater than second-line treatment was associated with good response based on multivariate analysis (HR 0.046; 0.004–0.497, P = 0.011). Single organ metastasis was the only meaningful factor related to higher disease control rate (P = 0.001). Based on multivariate analysis, single organ metastasis (HR 2.425; 1.231–4.775, P = 0.01) and development of skin toxicity (HR 0.461; 0.255–0.832) were related to a longer PFS. Skin toxicity (307 days vs. 159 days, P = 0.037), good PS (307 days vs. 74 days, P < 0.001), and single organ metastasis (535 days vs. 159 days, P = 0.002) were associated with a longer OS based on univariate and multivariate analyses.
There was no responder with a BRAF mutation (P = 0.563). Also, the disease control rate was higher in BRAF WT patients than patients with BRAF mutations (P = 0.636). Patients with BRAF mutations had shorter PFSs (139 days vs. 69 days, P = 0.068) and OSs (226 days vs. 74 days, P = 0.908; Fig. 1). In KRAS WTs, patients with high EGFR intron 1 CA repeat numbers showed a tendency for shorter PFS and OS than those with short CA repeat numbers (Fig. 1). The results of PFS and OS of KRAS WT patients are summarized in Table 5.
Kaplan–Meier curve for progression-free survival and overall survival according to molecular character. a Progression-free survival according to BRAF mutation in KRAS WT. b Overall survival according to BRAF mutation in KRAS WT. c Progression-free survival according to EGFR intron 1 CA repeat number in KRAS WT. d Overall survival according to EGFR intron 1 CA repeat number in KRAS WT. e Progression-free survival according to PTEN expression of primary sites in KRAS mutant
Predictive markers for treatment outcomes in KRAS mutant tumor
Among 19 patients with KRAS mutations, only one patient responded to cetuximab-containing chemotherapy. The PFS and OS in these patients were 121 days (95% CI, 78–163) and 258 days (95% CI, 125–390). Based on univariate analysis, PTEN expression in primary tumors was associated with a longer PFS, with a median PFS of 150 days (95% CI, 75–224) compared to 84 days in tumors that did not express PTEN (95% CI, 60–107; P = 0.019; Fig. 1). Additionally, development of skin toxicity was also a predictive marker of a favorable PFS (140 days vs. 77 days, P = 0.002). Based on multivariate analysis, expression of PTEN correlated with improved PFS (HR 0.141; 0.023–0.857, P = 0.033), and skin toxicity was a predictive marker for a longer PFS (HR 0.243; 0.059–1.003, P = 0.050). In addition, there was a trend toward a longer PFS in patients with a short EGFR intron 1 CA repeat number, but the difference did not reach the threshold of significance (126 days vs. 94 days, P = 0.704).
Discussion
This study can give us the information of discrepancy of molecular markers between primary tumor tissue and metastatic tumor tissue, and more detailed predictive markers for obtaining benefit from cetuximab therapy beyond KRAS.
It is widely accepted that EGFR expression does not predict benefit from cetuximab treatment as was the same in our study, and the role of pEGFR should be validated in more studies even though our study did not support its predictive role. Loss of PTEN by IHC or loss of PTEN gene function was reported as one of the predictive markers [16]. In patients who were treated with cetuximab plus irinotecan and did not have KRAS mutations in primary tumors, PTEN loss in metastases was reported to be predictive of resistance to cetuximab [11]. On the other hand, in KRAS mutants, our work suggested that PTEN loss could be a predictive marker for poor outcome.
Although it has been hypothesized that PIK3CA mutations may be a predictive marker for poor response to cetuximab treatment [6, 17], several data, including our results, showed no correlation between PI3KCA mutations and the response to cetuximab treatment [18]. The mutation rate of PIK3CA in colon cancer was reported to be 7–18% [19, 20]; we had only one patient with a PIK3CA mutation. Interestingly, a PIK3CA mutant also presented with a KRAS mutation simultaneously. Also, we recognized the tendency of poor outcomes in BRAF mutants, although it did not reach the threshold of significance because of the small sample size.
There have been some concerns that EGFR FISH is not a standardized and easily reproducible method, and EGFR gene copy number could reflect EGFR activity [21, 22]. Our results showed that the EGFR amplification by FISH in KRAS WT could be a good predictive marker for treatment outcome of cetuximab, though it was not statistically significant.
Interestingly, we found the concordant expression of EGFR intron 1 CA repeat number between primary tumor and metastasis. It has been hypothesized that the number of CA single sequence repeat in the intron 1 of EGFR gene, which affects transcription efficiency of the genes, is associated with the response to EGFR inhibitors [23]. Previous report suggested that in a clinical study in colorectal cancer, polymorphic variations in the intron 1 of the EGFR gene are associated with response to EGFR inhibitors and may provide an explanation as to why the development of skin toxicity is associated with a favorable outcome [10]. Patients presenting high CA repeats, regardless of mutational status of KRAS, had a shorter PFS, which is similar to a previous report [24]. Our data added to growing evidence that EGFR intron 1 CA repeat number may be a predictive marker for cetuximab treatment outcome. These data warrant additional large-scale clinical studies to validate and integrate EGFR genotyping as a marker for the selection of patients to be treated with cetuximab.
So far, molecular marker studies of cetuximab have been mostly evaluated in primary tumors. Among several studies that investigated primary tumors and paired metastases by IHC, some studies have shown discordance of EGFR expression [2], and there was another study showing concordance of EGFR IHC [25]. We observed a different EGFR expression in primary tumors and metastases and suggest a genetic alteration in metastases.
KRAS mutations were found in 19 patients (27.6%) in this study, which was lower than that of previously reported data. Several considerations might be given to this point. First, technical problems could be the reason. Second, this might be explained by ethnic differences. One report suggested KRAS mutation rates are higher among African American than Caucasian [26]. Whereas majority of studies about KRAS mutation were done in Western country, there was no data about KRAS mutation rates in Asian population. Our study population consisted of Asian population. For this issue, more studies with large number of patients should be further needed. Third, this may reflect discordance of KRAS mutation between primary sites and metastases. While many previous studies had assessed the mutation status of KRAS in primary sites, our study included results from metastatic site if there was not available primary tumor tissue.
In case of KRAS mutation, a high concordance rate of 90% between primary tumors and metastases has been reported [27, 28]. But in our data, the concordance rate of KRAS mutation was lower (76%) than previous reports, and there was marginal statistical significance in the concordant expression of KRAS mutations between primary tumors and metastases. We suggest a change in the carcinogenesis pathway and the requirement of rebiopsy before cetuximab treatment is taken into consideration.
There is one previous report about differences in BRAF mutations. According to the results, one patient out of two with BRAF mutations in primary tumors showed a BRAF WT in metastasis [29]. We evaluated 20 patients with primary tumors and metastases and showed a high concordance rate (up to 90%) that was statistically significant.
All other molecular markers except the EGFR intron 1 CA repeat number and BRAF mutation were discordant between the primary site and metastasis.
These were meaningful results because there have been no published data regarding a discordance between these markers in mCRC.
In addition, our data showed a different expression rate of IGF-1R based on KRAS mutational status. In KRAS mutants, IGF-1R expression was observed more frequently than in KRAS WT patients. Previous reports have suggested the activation of IGF1/IGF1-R involved in transformation and tumorigenicity in colon cancer, and there is a tendency for a stronger expression of IGF-1R in larger colon tumors and in the presence of metastatic disease [7, 8]. Although we did not show differences in treatment outcome according to IGF-1R expression, it would be worthwhile to evaluate the functional association between both of them.
We confirmed that skin toxicity is a strong predictive marker for cetuximab treatment in mCRC, as previous studies have proved [30].
Our study was performed retrospectively in a small population; this is one of limitation of our study. Furthermore, enrolled patients were heterogenous. The majority of our population (80%) was treated with two or more chemotherapy regimens before cetuximab treatment. The benefit of cetuximab added to first-line or second-line irinotecan containing therapy has been addressed in two trials: the CRYSTAL and OPUS trials [30, 31]. However, our data provided some valuable information for the clinician that cetuximab has efficacy in heavily pre-treated patients with KRAS WTs. Furthermore, we demonstrated expression of variable molecular markers which could be predictive for treatment outcome of cetuximab therapy in mCRC. There have been few results about the association between EGFR intron 1 CA repeat length and outcome. The results that we obtained in primary tumors and paired metastases showed discordant expression of the majority of molecular markers. Furthermore, there have been few studies that have been performed in Eastern countries. Therefore, our data could provide a reference of expression for molecular markers in the Asian population, simultaneously giving information about who has a higher possibility to get benefits from cetuximab therapy before starting treatment.
We conclude that a skin rash is strong predictive marker, regardless of molecular markers, for good outcome in mCRC patients receiving cetuximab chemotherapy. And all other molecular markers except the EGFR intron 1 CA repeat number and BRAF mutation were discordant between the primary tumor and metastasis. In KRAS mutants, PTEN expression by IHC in the primary site could be a promising predictive marker, and in KRAS WT patients, a BRAF mutation was a strong predictive marker for poor treatment outcome. It is possible that EGFR intron 1 CA short repeat number and EGFR amplification are associated with favorable outcome in KRAS WT.
References
Chung KY, Shia J, Kemeny NE, Shah M, Schwartz GK, Tse A, Hamilton A, Pan D, Schrag D, Schwartz L, Klimstra DS, Fridman D, Kelsen DP, Saltz LB (2005) Cetuximab shows activity in colorectal cancer patients with tumors that do not express the epidermal growth factor receptor by immunohistochemistry. J Clin Oncol 23:1803–1810
Cappuzzo F, Finocchiaro G, Rossi E, Janne PA, Carnaghi C, Calandri C, Bencardino K, Ligorio C, Ciardiello F, Pressiani T, Destro A, Roncalli M, Crino L, Franklin WA, Santoro A, Varella-Garcia M (2008) EGFR FISH assay predicts for response to cetuximab in chemotherapy refractory colorectal cancer patients. Ann Oncol 19:717–723
Sartore-Bianchi A, Moroni M, Veronese S, Carnaghi C, Bajetta E, Luppi G, Sobrero A, Barone C, Cascinu S, Colucci G, Cortesi E, Nichelatti M, Gambacorta M, Siena S (2007) Epidermal growth factor receptor gene copy number and clinical outcome of metastatic colorectal cancer treated with panitumumab. J Clin Oncol 25:3238–3245
Lievre A, Bachet J-B, Boige V, Cayre A, Le Corre D, Buc E, Ychou M, Bouche O, Landi B, Louvet C, Andre T, Bibeau F, Diebold M-D, Rougier P, Ducreux M, Tomasic G, Emile J-F, Penault-Llorca F, Laurent-Puig P (2008) KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol 26:374–379
Di Nicolantonio F, Martini M, Molinari F, Sartore-Bianchi A, Arena S, Saletti P, De Dosso S, Mazzucchelli L, Frattini M, Siena S, Bardelli A (2008) Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J Clin Oncol 26:5705–5712
Jhawer M, Goel S, Wilson AJ, Montagna C, Ling Y-H, Byun D-S, Nasser S, Arango D, Shin J, Klampfer L, Augenlicht LH, Soler RP, Mariadason JM (2008) PIK3CA mutation/PTEN expression status predicts response of colon cancer cells to the epidermal growth factor receptor inhibitor cetuximab. Cancer Res 68:1953–1961
Weber MM, Fottner C, Liu SB, Jung MC, Engelhardt D, Baretton GB (2002) Overexpression of the insulin-like growth factor I receptor in human colon carcinomas. Cancer 95:2086–2095
Hakam A, Yeatman TJ, Lu L, Mora L, Marcet G, Nicosia SV, Karl RC, Coppola D (1999) Expression of insulin-like growth factor-1 receptor in human colorectal cancer. Hum Pathol 30:1128–1133
Cappuzzo F, Varella-Garcia M, Finocchiaro G, Skokan M, Gajapathy S, Carnaghi C, Rimassa L, Rossi E, Ligorio C, Di Tommaso L, Holmes AJ, Toschi L, Tallini G, Destro A, Roncalli M, Santoro A, Janne PA (2008) Primary resistance to cetuximab therapy in EGFR FISH-positive colorectal cancer patients. Br J Cancer 99:83–89
Amador ML, Oppenheimer D, Perea S, Maitra A, Cusati G, Iacobuzio-Donahue C, Baker SD, Ashfaq R, Takimoto C, Forastiere A, Hidalgo M (2004) An epidermal growth factor receptor intron 1 polymorphism mediates response to epidermal growth factor receptor inhibitors. Cancer Res 64:9139–9143
Loupakis F, Pollina L, Stasi I, Ruzzo A, Scartozzi M, Santini D, Masi G, Graziano F, Cremolini C, Rulli E, Canestrari E, Funel N, Schiavon G, Petrini I, Magnani M, Tonini G, Campani D, Floriani I, Cascinu S, Falcone A (2009) PTEN expression and KRAS mutations on primary tumors and metastases in the prediction of benefit from cetuximab plus irinotecan for patients with metastatic colorectal cancer. J Clin Oncol 27:2622–2629
Kim SJ, Rabbani ZN, Dong F, Vollmer RT, Schreiber EG, Dewhirst MW, Vujaskovic Z, Kelley MJ (2009) Phosphorylated epidermal growth factor receptor and cyclooxygenase-2 expression in localized non-small cell lung cancer. Med Oncol 27:91–97
Cappuzzo F, Hirsch FR, Rossi E, Bartolini S, Ceresoli GL, Bemis L, Haney J, Witta S, Danenberg K, Domenichini I, Ludovini V, Magrini E, Gregorc V, Doglioni C, Sidoni A, Tonato M, Franklin WA, Crino L, Bunn PA Jr, Varella-Garcia M (2005) Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer Inst 97:643–655
Frattini M, Balestra D, Suardi S, Oggionni M, Alberici P, Radice P, Costa A, Daidone MG, Leo E, Pilotti S, Bertario L, Pierotti MA (2004) Different genetic features associated with colon and rectal carcinogenesis. Clin Cancer Res 10:4015–4021
Frattini M, Ferrario C, Bressan P, Balestra D, De Cecco L, Mondellini P, Bongarzone I, Collini P, Gariboldi M, Pilotti S, Pierotti MA, Greco A (2004) Alternative mutations of BRAF, RET and NTRK1 are associated with similar but distinct gene expression patterns in papillary thyroid cancer. Oncogene 23:7436–7440
Frattini M, Saletti P, Romagnani E, Martin V, Molinari F, Ghisletta M, Camponovo A, Etienne L, Cavalli F, Mazzucchelli L (2007) PTEN loss of expression predicts cetuximab efficacy in metastatic colorectal cancer patients. Br J Cancer 97:1139–1145
Sartore-Bianchi A, Martini M, Molinari F, Veronese S, Nichelatti M, Artale S, Di Nicolantonio F, Saletti P, De Dosso S, Mazzucchelli L, Frattini M, Siena S, Bardelli A (2009) PIK3CA mutations in colorectal cancer are associated with clinical resistance to EGFR-targeted monoclonal antibodies. Cancer Res 69:1851–1857
Lievre A, Bachet J, Le Corre D, Boige V, Landi B, Emile J, Cote J, Tomasic G, Penna C, Ducreux M, Rougier P, Penault-Llorca F, Laurent-Puig P (2005) Kras mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res 66:3992–3995
Ogino S, Nosho K, Kirkner GJ, Shima K, Irahara N, Kure S, Chan AT, Engelman JA, Kraft P, Cantley LC, Giovannucci EL, Fuchs CS (2009) PIK3CA mutation is associated with poor prognosis among patients with curatively resected colon cancer. J Clin Oncol 27:1477–1484
Lievre A, Bachet J-B, Le Corre D, Boige V, Landi B, Emile J-F, Cote J-F, Tomasic G, Penna C, Ducreux M, Rougier P, Penault-Llorca F, Laurent-Puig P (2006) KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res 66:3992–3995
Lenz H, Van-Cutsem E, Khambata-Ford S, Mayer R, Gold P, Stella P, Mirtsching B, Cohn A, Pipas A, Azarnia N, Tsuchihashi Z, Mauro D, Rowinsky E (2006) Multicenter phase II and translational study of cetuximab in Metastatic Colorectal Carcinoma refractory to irinotecan, oxaliplatin and fluoropyrimidines. J Clin Oncol 24:4914–4921
Khambata-Ford S, Garrett CR, Meropol NJ, Basik M, Harbison CT, Wu S, Wong TW, Huang X, Takimoto CH, Godwin AK, Tan BR, Krishnamurthi SS, Burris HA III, Poplin EA, Hidalgo M, Baselga J, Clark EA, Mauro DJ (2007) Expression of epiregulin and amphiregulin and K-ras mutation status predict disease control in metastatic colorectal cancer patients treated with cetuximab. J Clin Oncol 25:3230–3237
Chrysogelos SA (1993) Chromatin structure of the EGFR gene suggests a role for intron 1 sequences in its regulation in breast cancer cells. Nucl Acids Res 21:5736–5741
Ruzzo A, Cremolini C, Loupakis F, Fornaro L, Santini D, Vincenzi B, Canestrari E, Magnani M, Falcone A, Graziano F (2009) Association of BRAF mutations and EGFR Intron-1 L/L genotype with resistance to cetuximab plus irinotecan treatment in KRAS wild-type metastatic colorectal cancer patients. J Clin Oncol (Meeting Abstracts) 27:4058
Molinari F, Martin V, Saletti P, De Dosso S, Spitale A, Camponovo A, Bordoni A, Crippa S, Mazzucchelli L, Frattini M (2009) Differing deregulation of EGFR and downstream proteins in primary colorectal cancer and related metastatic sites may be clinically relevant. Br J Cancer 100:1087–1094
Abboud R, Pai R, Picus J, Hall-Daniels LE, Suresh R, Wang-Gillam A, Sorscher S, Tan BR (2010) Demographic factors on the incidence of KRAS mutation in colorectal cancers. J Clin Oncol 28 (suppl):e14040 (abstr)
Rajagopalan H, Bardelli A, Lengauer C, Kinzler KW, Vogelstein B, Velculescu VE (2002) Tumorigenesis: RAF/RAS oncogenes and mismatch-repair status. Nature 418:934
Cejas P, Lopez-Gomez M, Madero R, De Castro J, Casado E, Belda C, Larrauri J, Barriuso J, Gonzalez-Baron M, Feliu J (2009) Concordance of K-Ras status between colorectal cancer (CRC) primaries and related metastatic samples considering clinicopathological features. J Clin Oncol (Meeting Abstracts) 27:4053
Artale S, Sartore-Bianchi A, Veronese SM, Gambi V, Sarnataro CS, Gambacorta M, Lauricella C, Siena S (2008) Mutations of KRAS and BRAF in primary and matched metastatic sites of colorectal cancer. J Clin Oncol 26:4217–4219
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, Bets D, Mueser M, Harstrick A, Verslype C, Chau I, Van Cutsem E (2004) Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 351:337–345
Tabernero J, Van Cutsem E, Diaz-Rubio E, Cervantes A, Humblet Y, Andre T, Van Laethem JL, Soulie P, Casado E, Verslype C, Valera JS, Tortora G, Ciardiello F, Kisker O, de Gramont A (2007) Phase II trial of cetuximab in combination with fluorouracil, leucovorin, and oxaliplatin in the first-line treatment of metastatic colorectal cancer. J Clin Oncol 25:5225–5232
Acknowledgments
This study was partly supported by Merck, co, Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, J.H., Han, SW., Oh, DY. et al. Analysis of KRAS, BRAF, PTEN, IGF1R, EGFR intron 1 CA status in both primary tumors and paired metastases in determining benefit from cetuximab therapy in colon cancer. Cancer Chemother Pharmacol 68, 1045–1055 (2011). https://doi.org/10.1007/s00280-011-1586-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-011-1586-z