Abstract
Purpose
In this pharmacokinetic/pharmacodynamic meta-analysis, we investigated relationships between clinical endpoints and sunitinib exposure in patients with advanced solid tumors, including patients with gastrointestinal stromal tumor (GIST) and metastatic renal cell carcinoma (mRCC).
Methods
Pharmacodynamic data were available for 639 patients of whom 443 had pharmacokinetic data. Sunitinib doses ranged from 25 to 150 mg QD or QOD. Models to express endpoint values and/or changes from baseline by the highest-correlating exposure measures were developed in S-PLUS or NONMEM using fixed- and mixed-effects modeling.
Results
Tentative relationships were identified between (1) steady-state AUC of total drug (sunitinib + its active metabolite SU12662) and time to tumor progression (TTP), overall survival (OS), with AUC significantly associated with longer TTP and OS in patients with GIST and mRCC, and incidence, but not severity, of fatigue; (2) steady-state AUC of sunitinib and response probability, with AUC significantly associated with objective response in patients with mRCC and stable disease in patients with both mRCC and GIST (with no such correlations in patients with solid tumors); (3) dose and tumor size reductions; (4) total drug concentration and diastolic blood pressure (DBP), with a typical patient on sunitinib 50 mg QD (the recommended dose) predicted to experience a maximum DBP increase of 8 mmHg; and (5) cumulative AUC of total drug and absolute neutrophil count (ANC), with ANC reductions occurring predominantly after one treatment cycle.
Conclusions
The results of this meta-analysis indicate that increased exposure to sunitinib is associated with improved clinical outcomes (longer TTP, longer OS, greater chance of antitumor response), as well as some increased risk of adverse effects. A sunitinib 50-mg starting dose seems reasonable, providing clinical benefit with acceptably low risk of adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sunitinib malate (SUTENT®, SU11248) is an oral multi-targeted tyrosine kinase inhibitor exhibiting direct antitumor and antiangiogenic activity. It selectively inhibits vascular endothelial growth factor receptors (VEGFRs-1, -2, and -3), platelet-derived growth factor receptors (PDGFRs-α and -β), stem-cell factor receptor (KIT), FMS-like tyrosine kinase 3 (FLT3), colony-stimulating factor 1 receptor (CSF-1R), and glial cell line-derived neurotrophic factor receptor (REarranged during Transfection; RET) [1–7]; Pfizer Inc., data on file. Sunitinib has been approved multinationally for the treatment of advanced renal cell carcinoma (RCC) and for gastrointestinal stromal tumor (GIST) after disease progression on or intolerance to imatinib mesylate therapy. In addition, clinical studies confirm that the drug shows activity in several other solid tumor types [8, 9].
Pharmacokinetic studies show that sunitinib is well absorbed, and that its bioavailability is unaffected by food [10, 11]. After absorption, sunitinib is converted to an equipotent metabolite, SU12662 [11, 12]. Since SU12662 has a similar inhibitory profile to sunitinib in preclinical assays, the combination of sunitinib plus SU12662 represents the total active drug in plasma—although sunitinib exposure is 3–4 times higher than SU12662 exposure after administration of the drug [13].
Plasma levels of sunitinib peak between 6 and 12 h after a single oral dose, and total oral clearance (CL/F) is independent of dose at 50–150 mg/day [11, 13]. Sunitinib and SU12662 have prolonged terminal half-lives of approximately 40–60 and 80–110 h, respectively [13]. Following repeated daily administration, sunitinib accumulates 3–4-fold and SU12662 accumulates 7–10-fold; steady-state concentrations are achieved within 10–14 days [13]. No significant differences in pharmacokinetics are observed comparing either repeated with single dosing, or healthy volunteers with cancer patients. Both sunitinib and SU12662 are metabolized predominately by cytochrome P450 (CYP) 3A4, and elimination is primarily via the feces [12, 13].
Three phase I studies in patients with advanced solid tumors identified sunitinib 50 mg daily as the maximum tolerated dose (MTD; defined in each protocol as the maximum dose with less than 33% incidence of dose-limiting toxicity [DLT]) [2, 14, 15]. The schedule selected for phase II and III studies was sunitinib 50 mg daily given for 4 weeks followed by 2 weeks off treatment (Schedule 4/2), comprising a 6-week cycle.
A sound understanding of key predictors of the pharmacokinetic and pharmacodynamic activity of a given drug facilitates its optimal use by helping to identify those patients most likely to respond to the drug, as well as factors that may predispose an individual to adverse effects. In addition, knowledge of key predictors can be used to guide and support dosing regimens in the target population and in special populations, as appropriate. A population pharmacokinetic analysis of sunitinib and its primary active metabolite, SU12662, found that the pharmacokinetics of both compounds were significantly influenced by several covariates including gender, age, and weight; however, the magnitude of the predicted changes in exposure minimized the necessity for dose adjustments [16]. In the present publication, we present the results of a pharmacokinetic/pharmacodynamic meta-analysis (using linear and non-linear mixed-effects modeling) investigating the relationship between sunitinib exposure and efficacy and tolerability endpoints. A further objective of our analysis was to identify factors that affect response to sunitinib in patients with solid tumors, including GIST and RCC.
Materials and methods
Study design
Data collected in six studies of sunitinib were used in this analysis (Table 1). The study design, population, and timing of measurements varied between studies. Patients had any solid tumor (two studies, protocols 002 and 005) [2, 15], advanced GIST (two studies, 013 and 1004) [17, 18], or metastatic RCC (mRCC; two studies, 014 and 1006) [19, 20]. Sunitinib doses ranged from 25 to 150 mg given orally once daily (QD) or once every other day (QOD) and was administered in three different treatment schedules (i.e., weeks on, weeks off treatment), including the 4/2, 2/2 and 2/1 schedules, with QOD dosing in the first two schedules only. All protocols were approved by an institutional review board and studies were run in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients.
Population pharmacokinetic data and pharmacodynamic data were collected for preliminary exploratory analyses to characterize exposure–efficacy and exposure–tolerability relationships for sunitinib, SU12662, and total drug (sunitinib + SU12662). Population pharmacokinetic data are reported separately [16]. Potential relationships identified were investigated further, using linear and non-linear mixed-effects modeling. Potential relationships included correlation of exposure with objective tumor response, time to tumor progression (TTP), overall survival (OS), tumor size changes, diastolic blood pressure, absolute neutrophil count (ANC), and fatigue.
Study assessments
To obtain best estimates of a variety of exposure measures for each patient in the six studies, descriptive pharmacokinetic models (described previously [16]) for the parent and metabolite were used, as only trough levels were available for the majority of patients in the included studies. The estimated exposure measures included the following: trough plasma concentrations over time (C trough, taking into account the patient’s dosing history); cumulative area under the concentration–time curve (AUCcum, also taking into account the patient’s dosing history); a 28-day ‘windowed’ cumulative AUC (AUC28day, including only doses taken over the previous 28 days); and steady-state AUC based on the patient’s last dose level (AUClast) or mean daily AUC at steady state (AUCss). Each measure was calculated for sunitinib, SU12662, and total drug (sunitinib + SU12662). Evaluations of dose–response relationships included the entire patient population. Evaluations of pharmacokinetic-response relationships were limited to the patient population with evaluable pharmacokinetic data.
Efficacy endpoints were based on the response evaluation criteria in solid tumors (RECIST) [21]. They included objective response [classified as a complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD)], with confirmation on repeat imaging at least 4 weeks after initial documentation of response; TTP, defined as time from start of treatment to first documentation of objective tumor progression or death due to cancer, and OS, defined as time from start of treatment to death. Efficacy was assessed by investigators.
Tolerability endpoints were those treatment-related adverse events deemed by investigators to be probably or definitely related to sunitinib treatment. In patients with solid tumors, the most common treatment-related adverse events of grade 3 maximum severity were fatigue, hypertension, and neutropenia, and the most frequent treatment-related adverse event of grade 4 maximum severity is increased lipase [SUTENT® investigator brochure (June 2007)]. All events were measured at baseline and at least one other timepoint after the first dose of sunitinib. Adverse events were graded according to the National Cancer Institute (NCI) Common Toxicity Criteria (CTC) Version 3.0.
Modeling and statistical analysis
In the exploratory analysis, measured efficacy and tolerability endpoints were assessed for being normally distributed and plotted against exposure measures. Potential relationships identified were tested with a linear regression model, and Pearson’s correlation coefficients were computed and tested for statistical significance. Exposure measures demonstrating the highest correlations were selected for further analysis.
Possible covariate effects on exposure–response were explored by segmenting the patient population on the basis of covariate values and exploring individual endpoint–exposure-measure relationships within each sub-group (using linear regression). The following covariates were screened: gender, age, body mass index (BMI) quartiles, race, baseline diastolic blood pressure (DBP), dosing schedule (Schedules 4/2, 2/2 and 2/1), and tumor type (healthy volunteer, solid tumor, mRCC, and GIST).
After completion of the exploratory analysis, models expressing endpoint value and/or change of this value from baseline, as a function of exposure measure, were developed in either S-PLUS or NONMEM. Models were tested for all efficacy endpoints and identified potential adverse event relationships (fatigue, DBP, and ANC). Fixed-effects modeling used S-PLUS (Version 6.1). Mixed-effects modeling used NONMEM (Version 5, level 1.1) [22] with first-order conditional estimation (FOCE) and/or Laplacian methods of maximum likelihood estimation. When NONMEM was preceded by S-PLUS, the S-PLUS best-fit parameters were used as starting values for the corresponding NONMEM mixed-effects model.
Efficacy endpoints
To explore the relationships between exposure and TTP and exposure and OS, AUCss was evaluated against each of these efficacy endpoints. For Kaplan–Meier analysis, patients were subdivided into two groups (less than the median AUCss; greater than or equal to the median AUCss). Patients with documented progression between the screening date and first assessment were removed from the analysis (n = 10), as it could not be ruled out that progression had occurred prior to sunitinib dosing.
The time-to-event analysis for TTP and OS [23] utilized a Weibull probability distribution model [24, 25], which is characterized by parameters φ and γ as shown below. This method can be used to model events with a decreasing, increasing, or constant hazard rate
where S(t) is the survival function (P[T > t]); p(t) is the probability density function (PDF[t]); φ = median time to the event (tumor progression/death); and γ = shape parameter.
Drug effect was described by:
where Slope is the slope of the drug exposure effect on time-to-event.
Tumor growth kinetics (dy/dt), assessed using sum of longest diameter (SLD) data from computed tomography (CT) scans, were described as a function of sunitinib concentrations with a drug effect amplifying the tumor death rate [26].
where k growth is the estimated tumor growth rate; k death is the tumor death rate; C(t) is the sunitinib concentration estimated from the population pharmacokinetic model [16] at time t; Progression(t) is the estimated progression at time t (represented by the function: exp(-λt), where λ is an estimated progression appearance factor); and y(t) represents the SLD at time t.
The categorical endpoints (RECIST-defined response and the graded tolerability endpoints) displaying potential relationships by exploratory analysis were investigated using a mixed-effects modeling approach with repeated-measures logistic regression [24, 27–29]. The probability that the grade of the event (Y) is less than or equal to grade m (e.g., m = 0, 1, 2, 3, or 4 for NCI-CTC) was modeled in the form:
where Pr = probability; Logit = logit transform; and η Y is a random individual effect parameter that accounts for the variability in response at the same exposure.
Fatigue
Fatigue data were analyzed using repeated-measures logistic regression. A two-part mixture model was used to account for the high proportion of observations of no event [28]. Two logit probability models were used together to describe the data, the first describing incidence of fatigue as a function of exposure:
The second model was a standard logit probability model for repeated measurements, describing the probability of exceeding a given fatigue grade for an individual patient:
where i = subject index; j = time index; k = fatigue severity of (NCI-CTC) 0, 1, 2, 3, or 4; Time = time after start of study; Fatigue ij = fatigue score at time j in subject i; Exposure ij = exposure measure (as described above) at time j in subject i; Maximum Fatigue i = maximum fatigue in subject i. The model parameters are: P max = maximum placebo response; k = time constant to reach maximum placebo response; β k = fatigue rates at time 0 with no drug; Slope = slope of exposure–response relationship for incidence or severity, and η i is the inter-subject variability.
Model parameters were estimated using the Laplacian estimation to the likelihood in NONMEM. The effect of tumor type on the exposure–response relationship was also examined.
Absolute neutrophil count
Correlation coefficients were calculated for the relationship between estimated exposure measure and observed ANC; the greatest correlation was between 28-day cumulative area under the concentration–time curve for total drug (AUCCum28Tot) and ANC. Repeated-measures mixed-effects modeling methods were used to analyze the relationship between ANC and exposure measures. The final model described ANC as a function of baseline ANC levels, and a linear function of exposure. The slope of the exposure–response relationship varied among subjects, and was dependent on baseline ANC and tumor type. The baseline factor was introduced because patients with greater baseline ANC levels could have greater ANC reduction. The model equations were:
where i = subject index; j = time index. The variables are defined as follows: ANC ij = absolute neutrophil count at time j in subject i; Baseline ANC = baseline absolute neutrophil count; Exposure ij = exposure (as described above) at time j in subject i; X GIST is an indicator variable = 1 in GIST patients and 0 otherwise; X mRCC is an indicator variable = 1 in mRCC patients and 0 otherwise; η i is inter-individual variability in slope with mean zero and variance ω2; ε ij is intra-individual variability in ANC count with mean zero and variance σ2. The model parameters are defined as follows: SlopeTyp = slope of exposure–response relationship in a typical solid-tumor patient; k GIST = slope factor in GIST patients; k mRCC = slope factor in mRCC patients; k Base = slope factor for different baseline ANC counts; k = onset of effect; ω2 = inter-individual variance; σ2 = intra-individual variance. The value 5.4 represents the median baseline ANC count in this patient population.
Model parameters were estimated using the FOCE method in NONMEM. Models were compared on the basis of the distribution of post-hoc inter-subject variability estimates (η s), the reasonableness and precision of model parameters, a comparison of post-hoc predictions with observations in each individual, and a comparison of the model-prediction with the data.
Diastolic blood pressure
Correlation coefficients were calculated for the relationship between estimated exposure measure and observed DBP; the greatest correlation was between total drug trough concentrations (C troughTot) and DBP. Three models (linear, E max, and power models) were developed to describe DBP and its change from baseline as a function of C troughTot. The E max model provided the best descriptive summary of this relationship, and was subsequently implemented as a mixed-effects non-linear model in NONMEM.
The E max model was:
where E 0 is the DBP at baseline, E max is the maximum possible increase in DBP, and EC 50 is the C troughTot value that achieves 50% of the maximum DBP increase.
Results
Patient data
Patient demographics and a summary of the pharmacodynamic and pharmacokinetic datasets are shown in Table 2. A total of 639 patients had evaluable pharmacodynamic data and 443 of these patients had pharmacokinetic parameter estimates. Pharmacokinetics were shown, previously, to be similar between patients with RCC, GIST and solid tumors [16]. Table 3 summarizes the number of patients for which each endpoint measurement was available and the median value for each endpoint.
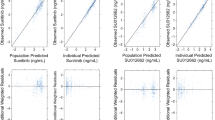
Figure 1 shows mean daily AUCss by final dose level, calculated using clearance estimated in the pharmacokinetic models for parent and total drug [16]. The majority of patients received sunitinib 50 mg, although final doses ranged from 25 to 100 mg. However, the variability in clearance produced similar exposure ranges across the doses, making dose–response modeling challenging.
Efficacy endpoints
Patients with the highest exposure to sunitinib displayed longer TTP and OS (Fig. 2). This relationship was consistent across the different tumor types. Similar results were seen when the data were analyzed using total drug concentrations (the primary active metabolite, SU12662, comprises 23–37% of the total exposure [13]). To further assess the significance of the relationships between drug exposure and TTP and drug exposure and OS, a time-to-event model was utilized. This model indicated that AUCss was significantly associated with longer TTP and OS in GIST and mRCC (Table 4).
To evaluate the relationship between investigator-assessed RECIST-based objective responses and exposure to sunitinib, logistic regression was performed. There was a significant relationship between exposure and the probability of a PR or CR in mRCC patients (P = 0.00001; Fig. 3). This trend was consistent but did not reach statistical significance for patients with GIST (P = 0.06) and solid tumors (P = 0.28; Fig. 3). The relationship between the probability of SD and sunitinib exposure was significant for both patients with mRCC (P = 0.002) and patients with GIST (P = 3 × 10−9) but not for patients with solid tumors (P = 1.7; Fig. 4). Collectively, these data indicate a trend toward a higher probability of tumor size decreases (PR) or halting of tumor growth (SD) in patients with higher exposure to sunitinib.
Probability of a partial or complete response (by RECIST criteria) versus average daily exposure (mean daily AUC at steady state, AUCss) to sunitinib. Lines represent model prediction and shaded area represents 95% confidence interval. Modeling results only displayed for relationships displaying statistical significance
Probability of stable disease (by RECIST criteria) versus average daily exposure (mean daily AUC at steady state, AUCss) to sunitinib. Lines represent model prediction and shaded area represents 95% confidence interval. Modeling results only displayed for relationships displaying statistical significance
Tumor size changes over time were further described using a tumor growth dynamics model. Model-based predictions of tumor sizes were consistent with the observed study data for both GIST and mRCC patients (Figs. 5, 6, 7), although the diagnostic plots indicated an increase in the residuals and a larger under-prediction of tumor size after approximately 400 days. Parameter estimates for the tumor growth dynamics models are presented in Table 5. Simulations with the final model estimates for both GIST and mRCC displayed the increased tumor size changes expected at doses between 25 and 50 mg QD on Schedule 4/2 (Fig. 8). Simulations suggested that 38% more mRCC and 23% more GIST patients would be expected to achieve a 30% reduction in tumor size when administered sunitinib 50 mg versus 25 mg QD.
Treatment-related adverse events
In patients with solid tumors, the most common treatment-related adverse events of grade 3 maximum severity are fatigue, hypertension, and neutropenia, and the most frequent treatment-related adverse event of grade 4 maximum severity is asymptomatic increased lipase [SUTENT® investigator brochure (June 2007)]. These safety measures were evaluated against sunitinib exposure, initially by screening with linear regression and Pearson’s correlation coefficients (Table 6). Exposure measures demonstrating the highest correlations were then selected for detailed exposure–response analysis. Lipase changes correlated less than 5% with any exposure measure and were not evaluated further as a function of exposure.
Fatigue
A positive relationship between exposure (total drug AUCss) and incidence, but not severity, of fatigue was identified. This relationship displayed a distribution consistent with the existence of two sub-populations comprising (1) a normally distributed range of fatigue scores among patients who experienced fatigue (grade ≥ 1), and (2) a second sub-population of patients who did not display fatigue at any time during the study. This distribution among patients who experienced fatigue was evident by analysis of between-subject variability for the unconditional severity model versus fatigue incidence (Fig. 9). Using a simulation with 1,000 patients, the half-life for the appearance of fatigue was 8 days and the maximum level of fatigue (if experienced) was therefore reached after one treatment cycle of sunitinib (Fig. 10). The model showed a relationship between sunitinib exposure and the probability of grade ≥ 1 fatigue in the three tumor types, as summarized for the 25- and 50-mg QD doses as follows: GIST: 46 and 65%, respectively; mRCC: 57 and 74%, respectively; and solid tumors: 85 and 92%, respectively.
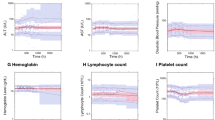
Absolute neutrophil count
Analysis of ANC values over the course of treatment revealed a negative relationship between ANC and exposure (AUCcum28Tot; Table 7; Fig. 11). The slope of the exposure–response relationship was also significantly greater (P < 0.05) in those with the highest ANC at baseline (for a 10% increase in baseline ANC, patients had approximately a 3.5% greater ANC reduction). Furthermore, relative to patients with solid tumors, a 36% greater ANC reduction occurred in patients with GIST (16% in mRCC). ANC level changes occurred predominantly after one cycle of sunitinib treatment and did not progress with later cycles. This model estimated that a solid tumor patient with a baseline ANC of 5 (counts/nL) might display a decrease of 0.9 (counts/nL) at a dose of sunitinib 25 mg QD, and 1.3 (counts/nL) at a dose of 50 mg QD.
Diastolic blood pressure
A positive relationship was identified between DBP changes and total drug (sunitinib + SU12662) exposure (trough plasma concentration for total drug, C troughTot). The relationship between DBP elevations at any time during treatment with sunitinib was best described by a non-linear (E max) function (Fig. 12). The estimate of the baseline DBP across the population was 74 mmHg and the estimated inter-individual variability (standard deviation) of baseline DBP was approximately 10% of the baseline value. The estimated maximum drug-mediated change in DBP for the population was 17 mmHg, with an inter-individual variability of approximately 36% of this value. The median C trough value for the population on sunitinib 50 mg QD was 0.068 μg/mL, below the estimated EC 50 of the effect on DBP of 0.084 μg/mL. This suggests that a typical patient on sunitinib 50 mg QD would be expected to experience a maximum elevation in DBP of 8 mmHg. At a dose of sunitinib 25 mg QD, an estimated 5-mmHg change in DBP is predicted.
Discussion
This study systematically analyzed pharmacokinetic and pharmacodynamic data from six clinical studies of sunitinib to identify sources of variability affecting clinical response or adverse events. As with most clinical studies in oncology, there are many constraints to identifying an exposure–response relationship. Primarily, these include sparse (if any) placebo data and the narrow dose ranges employed (typically all patients on cancer therapy initiate treatment at the MTD); the latter constraint was a specific potential limitation in this model given the number of patients included from phase I studies who received the lower and upper range of sunitinib dosing, the analysis of which may have been more relevant to exposure-toxicity than exposure-efficacy modeling. In addition, sparse sampling in some patients may have adversely impacted the individual estimates of pharmacokinetic parameters, and lack of inclusion of dose reductions or dose delays due to adverse events may have led to overly optimistic simulated results in the model. Furthermore, individualized dose titration during the time a patient is on study eliminates the possibility of performing a dose–response analysis on parallel dose groups (i.e., no two subjects receive the exact same dosing regimen throughout the entire study). The clinical studies included in this analysis were no exception. A small sub-set of placebo patients from one GIST study (n = 59, median of 62 days on placebo) provided the only patients for identification of baseline hazard rates for disease progression or adverse-event occurrence. Additionally, within treated subjects, the dose ranges were small (25–100 mg; and the vast majority of patients [85%] started treatment with sunitinib 50 mg QD) with individualized dose titration. However, using fixed- and mixed-effects modeling approaches, relationships were identified between exposure to sunitinib and efficacy and safety endpoints.
Patients with the highest exposure to sunitinib displayed longer TTP, longer OS, a higher probability of a response, and greater tumor size decreases. Thus, the analysis highlights the importance of maintaining patients on a 50-mg dose of sunitinib and striving to avoid unscheduled dosing interruptions or titration during treatment. In those patients for whom it may not be possible to maintain a full dose, use of alternative dosing schedules (e.g., Schedules 4/2, 2/2 or 2/1), as were employed in some studies used in this analysis, may provide benefit in some patients; however, this supposition requires verification in further analysis of additional data.
The relationship between RECIST-based objective response and exposure only reached statistical significance for patients with mRCC, possibly as a result of the higher incidence of response in patients with mRCC (40–43%) [19, 20] compared to those with GIST (7–8%) [17, 18] or solid tumors (10–27%) [2, 15] and the resulting contribution to statistical significance in the analyses reported here.
Tentative relationships were identified between sunitinib exposure and fatigue, diastolic hypertension, and neutropenia. Again, analysis of the adverse events was limited by the paucity of placebo data and the narrow range of doses, making it difficult to attribute these adverse events to sunitinib alone versus the disease process itself. Analysis of fatigue adverse-event data suggested that increased sunitinib exposure affected the incidence but not the severity of fatigue. The severity of fatigue reached a plateau after one cycle and was predicted to be more common in the group of patients with advanced solid tumors than in those with GIST or RCC. Clinical experience shows that the fatigue associated with sunitinib 50 mg/day when given for 4 weeks followed by 2 weeks off treatment is manageable [18, 20]. Relationships between sunitinib exposure and ANC and DBP adverse events were also identified. Specifically, these analyses indicated that increasing sunitinib exposure was correlated negatively with changes in ANC and positively with changes in DBP. However, at a dose of 50 mg/day given on Schedule 4/2, these effects are generally mild to moderate in severity and easy to manage [18, 20].
In a population pharmacokinetic analysis of data from studies in healthy volunteers and patients with cancer, sunitinib and its metabolite (SU12662) were modeled [16]. This analysis showed high inter-patient variability in pharmacokinetics, with coefficients of variation in the range of 40–60%. Thus, certain patients in a given population treated with the same dose/schedule may experience increased exposure to sunitinib. For example, population pharmacokinetic modeling suggested that approximately 8% of patients given sunitinib 50 mg QD would have at least as much exposure (AUCss) as a typical individual receiving a 75-mg QD dose [16]. The population pharmacokinetic analysis identified female gender and low body weight as covariates that significantly increase exposure to sunitinib [16]. Combining these findings with our pharmacokinetic/pharmacodynamic data suggests that such patients may be at greater risk of fatigue, DBP elevation or ANC reduction. However, per the exposure–adverse-event relationships reported here, such adverse events were mild to moderate in severity and must be balanced against the trend toward greater efficacy observed in patients with higher exposure to sunitinib.
In conclusion, this analysis indicates that increased exposure to sunitinib is associated with longer TTP, longer OS, a higher probability of a response, and greater tumor size decreases. Increased exposure was also associated with adverse events; however, these were generally mild to moderate in severity. A 50-mg initial dose can provide clinical benefit with acceptably low risk of adverse events.
References
Abrams TJ, Lee LB, Murray LJ et al (2003) SU11248 inhibits KIT and platelet-derived growth factor receptor beta in preclinical models of human small cell lung cancer. Mol Cancer Ther 2:471–478
Faivre S, Delbaldo C, Vera K et al (2006) Safety, pharmacokinetic, and antitumor activity of SU11248, a novel oral multitarget tyrosine kinase inhibitor, in patients with cancer. J Clin Oncol 24:25–35
O’Farrell AM, Foran JM, Fiedler W et al (2003) An innovative phase I clinical study demonstrates inhibition of FLT3 phosphorylation by SU11248 in acute myeloid leukemia patients. Clin Cancer Res 9:5465–5476
Kim DW, Jo YS, Jung HS et al (2006) An orally administered multi-target tyrosine kinase inhibitor, SU11248, is a novel potent inhibitor of thyroid oncogenic RET/papillary thyroid cancer kinases. J Clin Endocrinol Metab 91:4070–4076
Mendel DB, Laird AD, Xin X et al (2003) In vivo antitumor activity of SU11248, a novel tyrosine kinase inhibitor targeting vascular endothelial growth factor and platelet-derived growth factor receptors: determination of a pharmacokinetic/pharmacodynamic relationship. Clin Cancer Res 9:327–337
Murray LJ, Abrams TJ, Long KR et al (2003) SU11248 inhibits tumor growth and CSF-1R-dependent osteolysis in an experimental breast cancer bone metastasis model. Clin Exp Metastasis 20:757–766
O’Farrell AM, Abrams TJ, Yuen HA et al (2003) SU11248 is a novel FLT3 tyrosine kinase inhibitor with potent activity in vitro and in vivo. Blood 101:3597–3605
Burstein HJ, Elias AD, Rugo HS et al (2008) Phase II study of sunitinib malate, an oral multitargeted tyrosine kinase inhibitor, in patients with metastatic breast cancer previously treated with an anthracycline and a taxane. J Clin Oncol 26:1810–1816
Socinski MA, Novello S, Brahmer JR et al (2008) Multicenter, phase II trial of sunitinib in previously treated, advanced non-small-cell lung cancer. J Clin Oncol 26:650–656
Bello CL, Sherman L, Zhou J et al (2006) Effect of food on the pharmacokinetics of sunitinib malate (SU11248), a multi-targeted receptor tyrosine kinase inhibitor: results from a phase I study in healthy subjects. Anticancer Drugs 17:353–358
Sakamoto KM (2004) SU-11248 Sugen. Curr Opin Invest Drugs 5:1329–1339
Bello CL, Bu H-Z, Patyna S et al (2007) A phase I mass-balance study to evaluate the metabolism and excretion of [14C]-sunitinib in healthy male subjects. Poster presented at the annual meeting of the American Association for Cancer Research, Los Angeles, 2007 (Abstract 9072)
SUTENT® prescribing information (revised November 2008) Pfizer Labs, Division of Pfizer Inc., New York. Available at: http://www.sutent.com. Accessed Feb 2009
Demetri DG, George S, Heinrich MC et al (2003) Clinical activity and tolerability of the multi-targeted tyrosine kinase inhibitor SU11248 in patients with malignant gastrointestinal stromal tumors refractory to imatinib mesylate. Presented at the 39th annual meeting of the American Society of Clinical Oncology, Chicago, 31 May–3 June 2003 (Abstract 3273). Available at: http://www.asco.org. Accessed Mar 2009
Rosen L, Mulay M, Long J et al (2003) Phase I trial of SU011248, a novel tyrosine kinase inhibitor in advanced solid tumors. Presented at the 39th annual meeting of the American Society of Clinical Oncology, Chicago, 31 May–3 June 2003 (Abstract 765). Available at: http://www.asco.org. Accessed Mar 2009
Houk BE, Bello CL, Kang D, Amantea M (2009) A population pharmacokinetic meta-analysis of sunitinib malate (SU11248) and its primary metabolite (SU12662) in healthy volunteers and oncology patients. Clin Cancer Res 15:2497–2506
Maki RG, Fletcher JA, Heinrich MC et al (2005) Results from a continuation trial of SU11248 in patients (pts) with imatinib (IM)-resistant gastrointestinal stromal tumor (GIST). Presented at the 41st annual meeting of the American Society of Clinical Oncology, Orlando, 13–17 May 2005 (Abstract 9011). Available at: http://www.asco.org. Accessed Mar 2009
Demetri GD, van Oosterom AT, Garrett CR et al (2006) Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet 368:1329–1338
Motzer RJ, Michaelson MD, Redman BG et al (2006) Activity of SU11248, a multi-targeted inhibitor of vascular endothelial growth factor receptor and platelet-derived growth factor receptor, in patients with metastatic renal cell carcinoma. J Clin Oncol 24:16–24
Motzer RJ, Rini BI, Bukowski RM et al (2006) Sunitinib in patients with metastatic renal cell carcinoma. JAMA 295:2516–2524
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Beal SL, Sheiner LB (1998) NONMEM users guides—Part I–VIII. NONMEM Project Group C255, University of California at San Francisco, San Francisco, 1988–1998
Fleming TR, Harrington DP (1991) Counting processes and survival analysis. Wiley Interscience, New York
Gieschke R, Burger HU, Reigner B et al (2003) Population pharmacokinetics and concentration–effect relationships of capecitabine metabolites in colorectal cancer patients. Br J Clin Pharmacol 55:252–263
Sheiner LB (1994) A new approach to the analysis of analgesic drug trials, illustrated with bromfenac data. Clin Pharmacol Ther 56:309–322
Claret L, Girard P, Zuideveld KP et al (2006) A longitudinal model for tumor growth size measurement in clinical oncology studies. Presented at the 15th annual meeting of the Population Approach Group in Europe, Bruges, Belgium, 14–16 June 2006 (Abstract 1004). Available at: http://www.page-meeting.org/page/page2006/P2006II_10.pdf. Accessed Mar 2009
Mould DR, Holford NH, Schellens JH et al (2002) Population pharmacokinetic and adverse event analysis of topotecan in patients with solid tumors. Clin Pharmacol Ther 71:334–348
Kowalski KG, McFadyen L, Hutmacher MM et al (2003) A two-part mixture model for longitudinal adverse event severity data. J Pharmacokinet Pharmacodyn 30:315–336
Wahlby U, Matolcsi K, Karlsson MO et al (2004) Evaluation of type I error rates when modeling ordered categorical data in NONMEM. J Pharmacokinet Pharmacodyn 31:61–74
Acknowledgments
The authors thank all of the patients and their families for their participation in the studies described herein. This work was supported in part by funding from Pfizer Inc, as well as support from the Ludwig Trust for Cancer Research (to G. D. Demetri). Editorial assistance was provided by ACUMED® (Tytherington, UK) and funded by Pfizer Inc.
Conflict of interest statement
B.E. Houk and C.L. Bello are full-time employees of Pfizer with stock ownership. B. Poland has a consultant/advisory role with Pharsight Corporation. L.S. Rosen has had a consultant/advisory role with and received funding from Pfizer. G.D. Demetri has had a consultant/advisory role with and received remuneration and funding from Novartis and Pfizer. R.J. Motzer has had a consultant/advisory role with Novartis and GlaxoSmithKline and received funding from Pfizer, Wyeth, and GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Houk, B.E., Bello, C.L., Poland, B. et al. Relationship between exposure to sunitinib and efficacy and tolerability endpoints in patients with cancer: results of a pharmacokinetic/pharmacodynamic meta-analysis. Cancer Chemother Pharmacol 66, 357–371 (2010). https://doi.org/10.1007/s00280-009-1170-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-009-1170-y