Abstract
Purpose
Administration of cisplatin causes changes in magnesium and potassium metabolism. The purpose of this study was to investigate day-to-day changes in renal and intestinal homeostasis of magnesium (Mg) and potassium (K) during repeated cisplatin treatments in rats to provide guidelines for human supplementation studies.
Experimental design
Rats were housed in metabolic cages with access to a diet containing excess Mg and K. Treatment was administered once a week for 3 weeks and comprised either cisplatin 2.5 mg/kg body weight i.p or, as sham treatment, isotonic NaCl 2.5 ml/kg body weight i.p. Urine and feces were collected every 24 h. Blood samples for measurement of plasma Mg and K were obtained from a permanent arterial catheter prior to each treatment cycle and at the termination of the study.
Results
Cisplatin exerted a significant negative effect on total Mg balance. This effect was cumulative with repeated doses of cisplatin. The observed difference was mainly due to the difference in Mg balance between the treatment day and the following 2–3 days. The cumulated urinary excretion of Mg did not differ significantly between the two groups at the end of follow-up. A significant decrease was observed in cumulated intestinal absorption in treated rats compared to control rats at the end of follow-up. Lowered intestinal absorption accounted for 90% of the difference in total Mg balance between the two groups as compared to the renal loss. Cisplatin treatment also exerted a negative effect on total K balance, although the difference between cisplatin-treated and control rats was not significant at the end of follow-up.
Conclusions
The Mg loss associated with cisplatin treatment was mainly the result of lowered intestinal absorption and not, as presently thought, the result of increased renal elimination. Instead, an increased renal reabsorption capacity was observed in response to decreased intestinal absorption. The study further showed that Mg and K metabolism are subject to predictable changes in intestinal absorption and renal excretion with each cisplatin treatment, and that knowledge of these changes can be used in planning supplementation. Thus, the experimental observations support intravenous supplementation on the day of treatment and 2–3 days after treatment followed by oral supplementation until the next treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The administration of cisplatin causes changes in magnesium (Mg) metabolism [1], expressed as a decrease in plasma Mg and a renal Mg reabsorption defect demonstrated by an inappropriate renal elimination in both humans and rats when introduced to an intravenous Mg load after cisplatin treatment [2]. The renal Mg elimination has been suggested to explain the observed decrease in plasma Mg [3]. Since Mg is almost entirely an intracellular cation, the effect of cisplatin on bone and skeletal muscle Mg stores becomes a major determinant of total body Mg homeostasis during treatment [4]. We recently reported a substantial intracellular depletion of both Mg and potassium (K) in patients treated with cisplatin, and also that this depletion was not correlated with the plasma concentration of either ion [5]. The study suggests that substitution of Mg and K stores during treatment with cisplatin is of importance.
For obvious reasons total balance studies during cisplatin treatment in patients are not feasible, and therefore one has to rely in part upon data derived from animal models when considering the effects of cisplatin treatment on Mg and K balance. The purpose of this study was to investigate the day-to-day renal and intestinal homeostasis of Mg and K during repeated cisplatin treatment in rats to provide guidelines for human supplementation studies.
Materials and methods
Animals and treatments
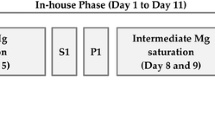
Female Wistar rats from Charles River (Sulzfeld, Germany) weighing 230–270 g were used. All animals had permanent tygon catheters placed in the left femoral artery for blood sampling. The animals were housed in metabolic cages under conditions of controlled temperature (22–24°C) and moisture (40–70%) with a 12-h light/dark cycle (light on from 6:00 a.m. to 6:00 p.m.). Animals were given free access to demineralized water and a granulated diet containing 2000 μg Mg/g (Altromin # 1320, Lage, Germany). The animals were given 3 days of adaptation to the new environment after which they were randomly assigned to active or sham treatment. Baseline data were obtained 24 h prior to the first treatment. Treatment was administered once a week for 3 weeks and comprised either cisplatin (Bristol-Myers Squibb, 1 mg/ml) 2.5 mg/kg body weight i.p or, as sham treatment, isotonic NaCl 2.5 ml/kg body weight i.p. The animals did not receive hydration treatment. After the animals were killed the abdominal cavity was inspected for signs of inflammation and agglutination. There was no evidence of intraperitoneal inflammation or intestinal agglutination after death and fecal output continued in all cisplatin-treated rats during the days after cisplatin injection.
Blood samples
Blood samples for measurement of plasma Mg and K were obtained from the arterial catheter prior to each treatment cycle and at the termination of the study. Immediately after sampling, the samples were centrifuged for 10 min at 3000 rpm at 4°C and the plasma was then frozen at −21°C until analysed using standard clinical chemistry systems VITROS 950 (Ortho-Clinical Diagnostics, Johnson & Johnson, N.J.).
Urine and feces samples
Total urine and fecal outputs were collected every 24 h. Prior to measurement fecal samples were hydrolysed in 20 ml 2 M HCl at 115°C for 1 h. Mg and K were then measured in samples of urine and feces by atomic absorption (AAnalyst 100; Perkin Elmer, Norwalk, Ct.). Creatinine clearance (Creacl) is urinary creatinine concentration × urinary volume/plasma creatinine. Electrolyte balance is intestinal absorption minus renal excretion. Fractional absorption is oral intake−fecal output/oral intake. All animal procedures followed the guidelines for the care and handling of laboratory animals established by the Danish government.
Statistics
SPSS statistical software was used. Data are presented as means±SEM. Differences were considered significant at the 0.05 level. Comparisons were made using an independent samples t-test. Correlations were established using Spearman’s test.
Results
Magnesium
Cisplatin exerted a significant negative effect on total Mg balance (Fig. 1). This effect was cumulative with repeated doses of cisplatin. The observed difference was mainly due to the difference in Mg balance between the treatment day and the following 2–3 days, whereas the slope of the curves were comparable for the remainder of each treatment cycle. The effect on Mg balance of cisplatin treatment was less during the first treatment cycle than during the subsequent two treatment cycles. The difference between treated and control rats in Mg balance at the end of follow-up was about 2500 μmol Mg, corresponding to 70% for cisplatin-treated compared to control rats.
As shown in Fig. 2a the cumulated urinary excretion of Mg did not differ significantly between the two groups at the end of follow-up. The observed difference in total renal Mg excretion at the end of follow-up was about 200 μmol Mg.
Cumulated urinary Mg excretion (a) and cumulated intestinal Mg absorption (b) in cisplatin-treated rats (n=12) and vehicle-treated rats (n=10). Bars indicate SEM. Arrows indicate cisplatin or NaCl treatment. Mg excretion (a) was not significantly different (n.s.), whereas Mg absorption (b) was significantly different (P<0.01), between groups at the end of follow-up
Figure 2b shows the cumulated intestinal Mg absorption. A significant decrease was observed in cumulated intestinal absorption in cisplatin-treated compared to vehicle-treated rats at the end of follow-up. The pattern of the curve for the cisplatin-treated rats followed the pattern shown in Fig. 1 reflecting the fact that intestinal absorption was the major determinant of Mg balance during cisplatin treatment. Thus, the difference between the two groups in intestinal absorption of Mg at the end of follow-up was about 2300 μmol Mg. Lowered intestinal absorption therefore accounted for 90% of the difference in total Mg balance between the two groups as compared to renal loss. Fractional intestinal Mg absorption was also lower in cisplatin-treated rats in the days following cisplatin injection, and immediately after the second and third injection net intestinal Mg secretion was observed (Fig. 3a). Between treatments, Mg absorption averaged 25–30%. A significantly decreased (P<0.01) mean intake of dietary Mg per 100 g body weight was observed in cisplatin-treated rats compared to controls as at the end of follow-up. Thus, after the first cisplatin injection dietary intake dropped by 40–50% and remained so throughout most of the follow-up period (Fig. 3b). The proportional decrease also applied to K. Renal Mg excretion was linearly correlated with intestinal Mg absorption in cisplatin-treated rats (r=0.64, P<0.01; Fig. 4a). This association was not present in control rats.
Potassium
Cisplatin treatment also exerted a negative effect on total K balance although the difference between cisplatin-treated and vehicle-treated rats was not significant at the end of follow-up (Fig. 5). The effect was seen immediately after each cisplatin injection which produced a steep decline in K balance lasting for 2 days following the injection. A similar effect was seen in control rats following the first injection with NaCl. After 2 days a more positive K balance was observed in cisplatin-treated rats than in vehicle-treated rats, and this difference persisted until the next injection. The difference between cisplatin-treated and vehicle-treated rats in K balance at the end of follow-up totalled about 1500 μmol K corresponding in cisplatin-treated rats to 70% of the balance in control rats taken as the optimal balance.
A significant difference in cumulated urinary K excretion between cisplatin-treated and vehicle-treated rats was observed at the end of follow-up. Cisplatin-treated rats had a lower excretion of K than vehicle-treated rats, in contrast to the observations for Mg which showed a higher excretion in cisplatin-treated rats (Fig. 6a). Although the effect on Mg was proportionally much greater, a decrease in K excretion was seen after each cisplatin injection lasting approximately 2 days, after which the slope of the curve was comparable to that of control rats. The difference in urinary K excretion between cisplatin-treated and vehicle-treated rats totalled about 22,000 μmol.
Cumulated urinary K excretion (a) and cumulated intestinal K absorption (b) in cisplatin-treated rats (n=12) and vehicle-treated rats(n=10). Bars indicate SEM. Arrows indicate cisplatin or NaCl treatment. The differences in both K excretion and K absorption between groups at the end of follow-up were significant (both P<0.01)
Cumulated intestinal K absorption was significantly less in cisplatin-treated than in vehicle-treated rats at the end of follow-up (Fig. 6b). Again, the negative effect on K absorption occurred mainly immediately after cisplatin injection. The difference in intestinal K absorption between cisplatin-treated and vehicle-treated rats totalled about 23,500 μmol at the end of follow-up. Although the effect on Mg was proportionally much greater, decreases in fractional K absorption were observed after the second and third cisplatin injection (Fig. 7). Between treatments, K absorption averaged approximately 95% but never decreasing below 85% even during cisplatin treatment.
Renal K excretion was linearly correlated with intestinal K absorption in cisplatin-treated rats (r=0.73, P<0.01; Fig. 4b). This association was not present in vehicle-treated rats.
Table 1 shows the plasma concentrations of Mg, K, Na, creatinine and urea, and weight and creatinine clearance during follow-up. No significant differences were observed between the two groups in the recorded plasma concentrations. A significant weight gain was recorded at the end of follow-up in the vehicle-treated group (P<0.01) compared to the cisplatin-treated group.
Discussion
In the present study cisplatin exerted a significant negative effect on total Mg balance. Although evidence of a cumulative negative effect on renal Mg conservation was observed, this effect was not the major determinant of the observed difference in Mg balance between cisplatin-treated and control animals. Previous studies have shown that changes in plasma Mg are due to a decrease in renal Mg reabsorption, which is also evidenced by the fact that following an intravenous Mg load increased Mg excretion is observed, despite cisplatin-induced hypomagnesaemia. This Mg leakage would therefore mainly account for the hypomagnesaemia and skeletal muscle Mg depletion observed in patients treated with cisplatin.
However, in the present study, 90% of the Mg loss compared to controls seemed to be the result of a decrease in fractional intestinal Mg absorption and that increased renal reabsorption was actually present during cisplatin treatment most likely as a response to the decreased intestinal absorption as evidenced by the linear association between intestinal Mg absorption and renal Mg excretion. Urinary loss was therefore at a minimum immediately after cisplatin injection indicating an adaptive increase in renal reabsorption. This effect did not seem to be mediated by a stable decrease in plasma Mg since plasma Mg remained unaffected in cisplatin-treated animals throughout the study. However, an unobserved decline in plasma Mg in the days following each cisplatin injection is possible since the study design measured plasma Mg in the relatively steady phase immediately prior to each injection.
It is noteworthy, that following both the second and third injection, urinary excretion occurred almost 0–3 days after treatment, despite the fact that intestinal absorption was quantitatively less affected following the third injection. Overall, the cisplatin-treated animals were able to retain 81% of the intestinally absorbed Mg, whereas control animals retained 87%. Nevertheless, the cisplatin-treated animals tended to show a slightly steeper renal excretion curve between treatments. It is not unlikely that further cisplatin injections or a larger population would have revealed significant differences in Mg excretion between the groups.
The fractional absorption decreased markedly after cisplatin injections. The exact mechanism by which Mg is absorbed in the intestine is not well understood. Mg absorption has been reported to rely mainly on passive diffusional transport [6] suggesting that Mg absorbance should be sensitive to lowered dietary intake. This is not, however, in accordance with the findings of the present study. For several days between treatments cisplatin-treated animals showed an increase in fractional absorption of Mg compared to control animals, thereby producing almost identical slopes on the cumulated intestinal absorption curves despite a reduced dietary Mg consumption. This would indicate at least some ability to actively alter intestinal Mg absorption in response to reduced dietary intake under these conditions, as would the fact that the fractional intestinal Mg absorption was sensitive to cisplatin.
It is interesting that despite an immediate effect on dietary intake after the first injection, the effect on absorption was much less pronounced in the first cycle than following the second and third injections. This might be due to a cumulative effect asserted by cisplatin, for example through an increased loss of transport capacity resulting in decreased fractional absorption. Finally, Mg absorption seems to be both a more sensitive and a much less effective process than K absorption with only about a 25% absorbance as compared to the absorbance of about 90% seen in K even after cisplatin treatment. This proportionally different effect also indicates that intestinal paralysis resulting from the intraperitoneal injection of cisplatin in the present model could not explain the observed effects.
As seen with Mg, intestinal absorption of K was also decreased in cisplatin-treated animals compared to control animals. However, the proportion of absorbed K excreted in the urine remained the same in both cisplatin-treated and control animals. Accordingly, the observed renal excretion was significantly lower in cisplatin-treated animals and the relative importance of renal K conservation in determining the total K balance was therefore much higher than observed with Mg. By comparison the difference in total Mg balance was 2500 μmol of which only 200 μmol was due to increased renal excretion in cisplatin-treated animals, whereas the difference in total K balance was only 1500 μmol despite the fact that the cisplatin-treated animals had a 23,500 μmol lower intestinal absorption.
The fact that both Mg and K are depleted in patients receiving cisplatin treatment, and that this depletion may pose a cardiac and a nephrotoxic risk, indicate that proper supplementation with Mg and possibly also K is relevant in these patients. Due to the tight regulatory association between intracellular levels of Mg and K, the question as to whether K supplementation is necessary during cisplatin treatment or whether the observed K depletion can be resolved just by correcting Mg levels is unresolved. The animal data from the present study indicate that planning the best supplementation should focus on the fact that intestinal absorption of especially Mg is at its lowest on the treatment day and during the following 2 days. Therefore, oral supplementation of Mg will not be beneficial in this period. In contrast intravenous supplementation in the same period would be beneficial because renal reabsorption is at its highest, whereas intravenous supplementation in between treatment would have less effect.
Therefore, based on the present animal studies it seems, that the best supplementation should consist of intravenous supplementation in prehydration and posthydration fluids combined with oral supplementation from approximately day 3 after treatment. Another option would be to consider whether Mg loading commencing before treatment might serve to avoid part of the observed depletion. Only carefully planned prospective studies in humans will be able to answer these important clinical questions for patients receiving platinum-containing chemotherapy.
In conclusion, this study showed that the Mg loss associated with cisplatin treatment is the result of lowered intestinal absorption and not, as presently thought, the result of increased renal elimination. Instead an increased renal reabsorption capacity was observed in response to decreased intestinal absorption. It further shows that Mg and K metabolism are subject to predictable changes in intestinal absorption and renal excretion with each cisplatin treatment, and that knowledge of these changes could be used in planning supplementation. Thus, the experimental observations support intravenous supplementation for and 2–3 days after treatment followed by oral supplementation until the next treatment.
References
Lajer H, Daugaard G (1999) Cisplatin and hypomagnesemia. Cancer Treat Rev 25(1):47–58
Mavichak V, Wong NL, Quamme GA, Magil AB, Sutton RA, Dirks JH (1985) Studies on the pathogenesis of cisplatin-induced hypomagnesemia in rats. Kidney Int 28(6):914–921
Lam M, Adelstein DJ (1986) Hypomagnesemia and renal magnesium wasting in patients treated with cisplatin. Am J Kidney Dis 8(3):164–169
Elin RJ (1987) Assessment of magnesium status. Clin Chem 33(11):1965–1970
Lajer H, Bundgaard H, Secher NH, Hansen HH, Kjeldsen K, Daugaard G (2003) Severe intracellular magnesium and potassium depletion in patients after treatment with cisplatin. Br J Cancer 89(9):1633–1637
Coudray C, Feillet-Coudray C, Grizard D, Tressol JC, Gueux E, Rayssiguier Y (2002) Fractional intestinal absorption of magnesium is directly proportional to dietary magnesium intake in rats. J Nutr 132(7):2043–2047
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lajer, H., Kristensen, M., Hansen, H.H. et al. Magnesium and potassium homeostasis during cisplatin treatment. Cancer Chemother Pharmacol 55, 231–236 (2005). https://doi.org/10.1007/s00280-004-0899-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-004-0899-6