Abstract
Purpose
SPI-077 and SPI-077 B103 are formulations of cisplatin encapsulated in pegylated STEALTH liposomes that accumulate in tumors. However, the extent to which active platinum (Pt) is released from the liposome is unknown. Thus, we evaluated the disposition of encapsulated and released Pt in plasma and tumors after administration of STEALTH liposomal and nonliposomal cisplatin.
Methods
Cisplatin (10 mg/kg), SPI-077 (10 mg/kg), and SPI-077 B103 (5 mg/kg) were administered i.v. to mice bearing B16 murine melanoma tumors. Microdialysis probes were placed into the right and left sides of each tumor, and serial samples were collected from tumor extracellular fluid (ECF) after administration of each agent. After each microdialysis procedure, tumor samples were obtained at each probe site to measure total Pt and Pt-DNA adducts. In a separate study, serial plasma samples (three mice per time point) were obtained. Unbound Pt in tumor ECF and plasma, and total Pt in tumor homogenates were measured by flameless atomic absorption spectrophotometry. Area under the tumor ECF (AUCECF) concentration versus time curves of unbound Pt were calculated. Intrastrand GG (Pt-GG) and AG (Pt-AG) Pt-DNA adducts were measured via 32P-postlabeling.
Results
Mean±SD peak concentrations of total Pt in tumor homogenates after administration of cisplatin, SPI-077, and SPI-077 B-103 were 3.2±1.9, 11.9±3.0, and 3.5±0.3 μg/g, respectively. After cisplatin, mean±SD AUCECF of unbound Pt was 0.72±0.46 μg/ml·h. There was no detectable unbound Pt in tumor ECF after SPI-077 or SPI-077 B-103 treatment. Mean±SD peak concentration of Pt-GG DNA adducts after administration of cisplatin, SPI-077, and SPI-077 B-103 were 13.1±3.3, 3.5±1.3, and 2.1±0.3 fmol Pt/μg DNA, respectively.
Conclusion
This study suggests that more SPI-077 and SPI-077 B103 distribute into tumors, but release less Pt into tumor ECF, and form fewer Pt-DNA adducts than does cisplatin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cisplatin has antitumor activity against a wide range of solid tumors, especially in the treatment of epithelial malignancies [1]. STEALTH liposomal cisplatin formulations (SPI-077 and SPI-077 B103) were developed for the treatment of cancers that are generally sensitive to platinum (Pt), but may be resistant to conventional cisplatin, and to reduce toxicities by preferentially delivering drug to the tumor [2, 3, 4, 5, 6]. SPI-077 B103, an alternative formulation of SPI-077, was developed to enhance the release of Pt from the liposome. The plasma, tissue, and tumor disposition of liposomal encapsulated drugs is dependent on the liposomal vehicle [2, 3, 4, 5]. SPI-077 has a prolonged elimination phase with a systemic t1/2 of 30 to 40 h and 40 to 55 h in animals and humans, respectively [3, 4, 5]. After the cisplatin is released from the liposome, its disposition follows the pharmacokinetics of cisplatin [7, 8]. The clearance of cisplatin is rapid (i.e., t1/2 of unbound Pt is 15 to 20 min) and primarily represents irreversible binding to plasma proteins (i.e., 99% protein bound) [7, 8].
In theory, STEALTH liposomes accumulate in the intracellular spaces within tumors, and as the liposome disintegrates the encapsulated drug (e.g., cisplatin) is gradually released [9, 10]. However, the exact mechanisms for the rate and extent of drug release are unknown. In preliminary studies comparing SPI-077 and cisplatin tumor disposition in tumor-bearing mice, the Pt exposure in tumors was severalfold higher and prolonged after SPI-077 administration than after cisplatin administration [6]. However, because the Pt exposure was measured in tumor homogenates as total Pt, it is unclear what portion of the Pt measured was SPI-077 (i.e., encapsulated Pt), released active unbound Pt, or inactive protein-bound Pt. Even though there is a severalfold higher exposure of total Pt in tumors after SPI-077 compared to cisplatin, this did not translate into significant antitumor response in clinical trials [2, 3, 4]. In addition, there were high plasma concentrations of total Pt in patients, but no detectable ultrafilterable Pt in the plasma after administration of SPI-077 at doses <200 mg/m2 [2, 3, 5]. Since previous studies have shown that the intact liposome does not enter cells [6], one possible explanation for the inconsistency between the high tumor exposure in preclinical animal models and low antitumor effect in clinical trials could be the lack of release of active unbound Pt from the liposome into the tumor extracellular fluid (ECF).
Although concentrations of SPI-077 and cisplatin in the tumor ECF represent exposure in the immediate vicinity of the tumor cells, the mechanism of cytotoxicity of Pt-containing antitumor drugs is related to the formation of Pt-DNA adducts [11, 12]. Therefore, a more appropriate marker of cytotoxic exposure to liposomal encapsulated cisplatin and nonliposomal cisplatin may be the formation of Pt-DNA adducts. In addition, the relationships between unbound Pt in tumor ECF and total Pt in tumor homogenates, and formation of Pt-DNA adducts have not been evaluated for STEALTH liposomal cisplatin formulations.
Microdialysis is a relatively new in vivo sampling technique applied to the study of pharmacokinetics and drug metabolism in the blood and ECF of tissue [13, 14, 15]. Microdialysis has recently been used to evaluate tumor ECF disposition of anticancer agents in tumor xenografts and in patients with solid tumors [15, 16, 17, 18, 19]. Microdialysis is based on the diffusion of non-protein-bound drugs from interstitial fluid across the semipermeable membrane of the microdialysis probe. Due to the pore cut-off size (20 kDa) of the semipermeable membrane and size of the liposome (110 nm), use of microdialysis allows differentiation between liposomally encapsulated or protein-bound Pt and active released Pt in the tumor ECF. In addition, microdialysis provides a technique to obtain serial samples of drugs in tumor ECF from which a concentration versus time profile can be determined within a single tumor [13, 14, 15, 19].
The objectives of this study were: (1) to evaluate the in vitro recovery and release of Pt in solutions containing SPI-077 or SPI-077 B103 alone and in solutions containing cisplatin in combination with SPI-077 or SPI-077 B103; (2) to evaluate the disposition of unbound Pt in plasma and in tumor ECF using microdialysis methodology, and total Pt in tumor and tissue homogenates after administration of cisplatin, SPI-077, and SPI-077 B103; and (3) to determine the formation of intrastrand GG (Pt-GG) and AG (Pt-AG) platinum-DNA adducts within the tumor after administration of cisplatin, SPI-077, and SPI-077 B103.
Materials and methods
In vitro calibration studies
To characterize the recovery and release of Pt from STEALTH liposomes, and the effect of STEALTH liposomes on the recovery of Pt, we performed in vitro recovery studies of Pt in solutions containing SPI-077 or SPI-077 B103 alone, and in solutions containing cisplatin in combination with SPI-077 or SPI-077 B-103. CMA20 microdialysis probes (CMA 20, Stockholm, Sweden) with a molecular weight cut off of 20 kDa were used [14, 15, 19]. The microdialysis probe was perfused using a microdialysis microperfusion pump (CMA 102, Stockholm, Sweden). Dialysate samples were collected using a microfraction collector (CMA 142, Stockholm, Sweden). Each probe was placed into a 250-ml glass beaker that contained the following in vitro base solutions: (1) 0.5 μg/ml of cisplatin alone; (2) 0.5 μg/ml of SPI-077 alone; (3) 0.5 μg/ml of SPI-077 B-103 alone; (4) 0.5 μg/ml of cisplatin and 0.5 μg/ml of SPI-077; or (5) 0.5 μg/ml of cisplatin and 0.5 μg/ml of SPI-077 B103. The microdialysis probe was perfused with Ringer’s solution at 2 μl/min. Dialysate samples were collected every 30 min for four samples. In vitro recovery was calculated as the ratio of Pt concentration in the dialysate solution to the concentration of Pt in the in vitro base solution [14, 15, 19]. Pt concentrations in the dialysate and base solutions were measured by a flameless atomic absorption spectrophotometry (FAAS) [7, 8, 19].
Mice
All mice were handled in accordance with the Guide for the Care and Use of Laboratory Animals (National Research Council, 1996), and studies were approved by the Institutional Animal Care and Use Committee at the University of Pittsburgh Medical Center. Mice (female C57Bl/6, 4–6 weeks of age, and specific-pathogen-free) were obtained from the NCI Animal Production Program (Frederick, Md.), and were allowed to acclimate to the animal facilities at the University of Pittsburgh for 1 week prior to initiation of the study. Mice were housed in microisolator cages and allowed Teklad LM-484 autoclavable rodent chow (Harlan Tekla Diets, Madison, Wis.) or ISDPRO RMH3000 irradiated rodent chow (PMI Nutrition International, Brentwood, Mo.) and autoclaved water ad libitum. Body weights and tumors were measured twice weekly and clinical observations were made twice daily.
Tumor line
B16 murine melanoma cells was obtained from the DCTD Tumor Repository (Frederick, Md.) and were mouse antigen production test-negative. B16 tumors, as approximately 25-mg fragments, were implanted subcutaneously into the right flank of C57BL/6 mice using aseptic techniques. Pharmacokinetic and microdialysis studies were performed when the tumors were approximately 1000 to 1500 mm3 (1 to 1.5 g) in size.
Formulations and administration
SPI-077 is a formulation of cisplatin encapsulated in the aqueous core of sterically stabilized liposomes [2, 4, 5, 6]. Approximately 80% of the lipid in STEALTH liposomes is fully hydrogenated soy phosphatidylcholine (HSPC) and cholesterol. Methoxypolyethylene glycol (MPEG) is covalently bound to phosphatidylethanolamine and a component of the lipid bilayer. The mean particle size of the liposomes is approximately 110 nm, and cisplatin encapsulation exceeds 90%. The drug-to-lipid ratio is approximately 14 g cisplatin per milligram of lipid. The cisplatin concentration is 1 mg/ml, and doses of SPI-077 refer to actual doses of cisplatin.
A second formulation, SPI-077 B103, was developed to enhance the release of cisplatin from the STEALTH liposomes. The main difference between the two formulations is that the HSPC was replaced with unsaturated phospholipids in the SPI-077 B103 formulation (Alza Corporation, data on file). Previous in vivo studies have shown that liposomes with unsaturated phospholipids have more rapid leakage (Alza Corporation, data on file).
The concentrations of encapsulated and released cisplatin in the formulations of SPI-077 and SPI-077 B103 were measured in each vial. For analysis of encapsulated Pt plus released Pt (i.e., total Pt), 0.5 ml SPI-077 or SPI-077 B103 was diluted in 0.9% NaCl (USP, Baxter, Deerfield, Ill.), and then analyzed by FAAS. For analysis of the released Pt, the dosing solutions were ultrafiltered by placing 50 μl of the dosing solution into an Amicon Centrifree micropartition device (Amicon Division, W.R. Grace, Beverly, Mass.), and then centrifuged at 2000 g for 20 min at 4°C [11, 12]. The resulting ultrafiltrates were stored at −70°C until analyzed. Total and ultrafilterable Pt were measured by FAAS [7, 8, 19].
Cisplatin (10 mg/kg), SPI-077 (10 mg/kg), and SPI-077 B103 (5 mg/kg) were administered as a bolus via a lateral tail vein over approximately 30 s. The dose of SPI-077 B-103 was reduced to 5 mg/kg due to the onset of toxicity (weight loss, significant necrosis of the intestinal lining and bone marrow suppression) at >96 h after administration of SPI-077. Cisplatin and SPI-077 were diluted to 1 mg/ml in sterile 0.9% NaCl (USP, Baxter), and SPI-077 B103 was diluted to 0.5 mg/ml in sterile 0.9% NaCl. Doses were delivered at 0.01 ml/g of body weight.
Sample processing for plasma and tissue pharmacokinetic studies
Due to the limited blood volume of a mouse, plasma and tissue pharmacokinetic studies, and microdialysis studies were performed in separate groups of mice. Mice (three per time point) were killed with carbon dioxide, and heparinized blood samples (approximately 0.8 to 1 ml) were collected by cardiac puncture 5 min after administration of vehicle, and at 5, 15, 30, 45, 60, 90, and 120 min after cisplatin administration. Mice (three per time point) were killed with carbon dioxide, and heparinized blood samples (approximately 0.8 to 1 ml) were collected by cardiac puncture at 0.08 h after administration of vehicle, and at 2, 24, 96, and 144 h after administration of SPI-077 and SPI-077 B103.
Blood samples were centrifuged at 12,000 g for 4 min. For the analysis of total Pt in plasma, the resulting plasma was decanted into screw-top tubes, immediately frozen in liquid nitrogen, and stored at −70°C until analyzed. For analysis of unbound Pt in plasma, the plasma was immediately ultrafiltered by placing 50 μl of plasma into an Amicon Centrifree micropartition device (Amicon Division, W.R. Grace, Beverly, Mass.) and then centrifuged at 2000 g for 20 min at 4°C [11, 12]. The resulting ultrafiltrates were stored at −70°C until analyzed. Unbound Pt in the ultrafiltrate and total Pt in the plasma were measured by FAAS [7, 8, 19].
Tumor, liver, kidneys, and spleen were also obtained from each mouse used for the plasma pharmacokinetic studies described above. Tissues were removed, weighed, frozen in liquid nitrogen, and stored at −70°C until analyzed. For analysis of total Pt, tissue samples were thawed, homogenized in phosphate-buffered saline (PBS) (tissue:PBS at 1:3, w/v), and the homogenate was analyzed for Pt using FAAS [7, 8, 20].
Unbound Pt in tumor ECF, and total Pt and Pt-DNA adducts in tumors
To evaluate the variability in Pt exposure within a single tumor, dual microdialysis probe studies were performed in each tumor [15, 19]. Commercially available microdialysis probes (CMA 20, Stockholm, Sweden) with a molecular cut-off of 20 kDa, a membrane length of 4 mm, and an outer diameter 0.5 mm were used. Due to the pore cut-off size of the semipermeable membrane and size of the liposome (110 nm), only the unbound Pt released from the liposome into the tumor ECF could cross the semipermeable membrane and be collected. Additionally, only Pt not bound to large plasma proteins, such as albumin, could cross the semipermeable membrane and be collected [19]. Therefore, Pt samples collected by microdialysis from tumor ECF were defined as unbound Pt [19]. The microdialysis probe was perfused using a microdialysis microperfusion pump (CMA 102). Dialysate samples were collected using a microfraction collector (CMA 142).
Prior to administration of cisplatin, microdialysis probes were placed at parallel sites on the left and right sides of the tumor. For implantation of the probes, mice were anesthetized with pentobarbital (75 mg/kg i.p.), and 2-mm incisions were made in the skin 3 to 4 mm from the right and left ends of the tumor, and the probes were inserted 6 mm into the tumor. The incision sites were closed and probes were held in place with surgical glue. Probe placement was confirmed at necropsy.
After probe placement, 45 min was allowed for probe and tumor ECF equilibration [13, 14, 15]. The in vivo recovery of Pt by each probe in each tumor was assessed according to the retrodialysis method [13, 14, 15]. After the retrodialysis procedure, a washout period was performed, during which Ringer’s solution USP without cisplatin was perfused through the system. After administration of cisplatin, microdialysis sampling of tumor ECF was performed every 12 min for 120 min. The Pt concentration measured in each 12-min sample represented the average Pt concentration of that interval, and thus the time of the sample was defined as the mid-point of that interval (i.e., 6, 18, 30, 42, 54, 66, 78, 90, 102, and 114 min). The microdialysis samples were stored at 4°C until analyzed for Pt by FAAS [7, 8, 20].
After administration of SPI-077 or SPI-077 B103, microdialysis sampling of tumor ECF was performed every 0.2 h from 0 to 2, 24 to 26, 96 to 98, and 144 to 146 h. Individual mice were used for each 2-h sampling interval. For the 0 to 2-h collection period, the same procedures for probe placement, retrodialysis calibration, washout, and sample recovery were performed as in the cisplatin studies. For the 24 to 26-h, 96 to 98-h, and 144 to 146-h collection periods, the same procedures for probe placement and sample recovery were performed, but retrodialysis calibration was not performed because the drug had been administered.
At the end of the microdialysis procedures, tumor samples were obtained at each probe site and analyzed for total Pt. Tumor homogenates were processed, and total Pt was analyzed by FAAS. In addition, bifunctional intrastrand DNA adducts between Pt and two adjacent guanines (Pt-GG), and between Pt and adjacent adenines and guanines (Pt-AG) were measured in B16 tumor samples. A 32P-postlabeling assay was used to quantitate Pt-GG and Pt-AG platinum-DNA adducts [11].
Pharmacokinetic analysis
ADAPT II was used to fit a two-compartment pharmacokinetic model, with uncoupled distribution of the plasma and tumor compartments, to the plasma and tumor ECF concentration versus time profiles of unbound Pt [21]. The estimated systemic parameters for unbound Pt included volume of the central compartment (Vc) and elimination rate constant (k10) [21]. The estimated model for the plasma concentration versus time data was then used to represent the time-course of drug delivery to the tumor. Uptake and disposition in the tumor ECF were modeled separately [19, 21, 22]. The equation defining the concentration of unbound Pt in tumor ECF was defined as follows:
where CECF (ng/ml) denotes the concentration of unbound Pt in the tumor ECF, kP-ECF (h−1) is the rate of transfer of unbound Pt from plasma into tumor ECF, VECF (ml) is the volume of tumor ECF, kECF-P (h−1) is the rate constant of transport of unbound Pt out of tumor ECF, and Ap (ng) represents the fitted exponential function describing the amount of unbound Pt in the plasma. The kECF-P (h−1) represents the summation of the movement of drug from the tumor ECF. The model represented by Eq. 1 was fitted to the concentrations of unbound Pt in the tumor ECF. For each mouse and each tumor site, the maximum likelihood estimates of the ratio kP-ECF/VECF (plasma to tumor ECF transport rate constant per unit volume (ml) of tumor) and kECF-P were obtained.
The pharmacokinetic model was used to calculate the systemic clearance of unbound Pt (CL), and area under the plasma (AUCP) and tumor ECF (AUCECF) concentration versus time curves of unbound Pt from time zero to infinity [21, 23]. The penetration of unbound Pt into the tumor ECF was calculated as the ratio of AUCP to AUCECF [15, 19, 22].
Statistical analysis
The Wilcoxon rank sum test was used to compare the AUCECF, total Pt in tumor homogenates, and Pt-GG and Pt-AG DNA adducts, after administration of cisplatin and SPI-077 [24, 25]. In addition, the Sample t-test assuming equal variances was used to compare the peak concentrations of total Pt in plasma, tumor, liver, kidney, and spleen [24, 25]. StatXact-3 software (Hearne Scientific Software, Melbourne, Australia) was used to perform the Wilcoxon rank sum test.
Results
Total and ultrafilterable cisplatin in stock solutions of SPI-077 and SPI-077 B-103
The total and ultrafiltrate concentrations of cisplatin in the stock solution of SPI-077 were 1.1 and 0.02 mg/ml, respectively. The total and ultrafiltrate concentrations of cisplatin in the stock solution of SPI-077 B103 were 1.0 and 0.06 mg/ml, respectively.
In vitro calibration studies
There was no detectable Pt in the dialysate solutions after in vitro recovery studies of SPI-077 and SPI-077 B103 alone. At room temperature, the mean±SD in vitro recoveries of cisplatin from solutions containing cisplatin alone, cisplatin and SPI-077, and cisplatin and SPI-077 B103 were 0.43±0.07, 0.45±0.03, and 0.37±0.04, respectively (P>0.05).
Plasma, tumor, and tissue pharmacokinetic studies
The plasma concentration versus time profiles of total Pt and unbound Pt after administration of cisplatin are presented in Fig. 1. After cisplatin administration, unbound Pt in plasma was detectable in all mice from 5 min to 2 h. The concentration versus time profile of unbound Pt was best fitted with a one-compartmental model, and the CL, k10, and Vc, were 500 l/h/m2, 2.3 h−1, and 143 l/m2, respectively. Unbound Pt was not detectable in plasma after administration of SPI-077 and SPI-077 B-103.
Concentration versus time profiles of total Pt and unbound Pt in plasma, and unbound Pt in tumor ECF after administration of cisplatin at 10 mg/kg. The mean and SD of total Pt in plasma (▲), unbound Pt in plasma (■), and unbound Pt in tumor ECF (○) are presented. The mean and SD of total Pt and unbound Pt in plasma were calculated from three mice at each time-point. The mean and SD of unbound Pt in tumor ECF was calculated at the mid-point of each interval from the 12 microdialysis studies. The concentration of Pt measured in each 24-min sample of tumor ECF from 0 to 120 min represents the average concentration of that interval. Thus the time of the sample was defined as the mid-point of that interval (i.e., 6, 18, 30, 42, 54, 66, 78, 90, 102, and 114 min)
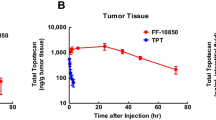
The concentrations of total Pt in plasma, tumor, kidney, liver, and spleen after administration of cisplatin, SPI-077, SPI-077 B103 are presented in Table 1. Because SPI-077 and cisplatin were both administered at 10 mg/kg and SPI-077 B103 was administered at 5 mg/kg, statistical comparisons were only performed on data after administration SPI-077 and cisplatin. Total Pt was detectable in plasma from 0.083 h to 2 h after administration of cisplatin. Total Pt was detectable in plasma from 2 h to 144 h after administration of SPI-077 and SPI-077 B103. The peak plasma concentrations of total Pt were significantly greater after administration of SPI-077 (104.6±33.6) than after administration of cisplatin (14.2±5.7 μg/ml; P<0.05). The peak concentrations of total Pt in tumor were approximately 4-fold greater after administration of SPI-077 than after administration of cisplatin (P<0.05). In addition, the time to peak concentrations of total Pt in tumor were longer after administration of SPI-077 (48 h) and SPI-077 B103 (96 h) than after administration of cisplatin (0.5 h). The peak concentrations of total Pt in liver were approximately 2-fold higher after administration of SPI-077 than after administration of cisplatin (P<0.05). The peak concentrations of total Pt in spleen were approximately 28-fold higher after administration of SPI-077 than after administration of cisplatin (P<0.05). However, the peak concentrations of total Pt in kidney were approximately 2-fold higher after administration of cisplatin than after administration of SPI-077 (P<0.05).
Unbound Pt in tumor ECF, and total Pt and Pt-DNA adducts in tumors
The concentration versus time profiles of unbound Pt in tumor ECF are presented in Fig. 1. Unbound Pt was detectable in the tumor ECF of each tumor evaluated, but the concentrations of unbound Pt and the time that unbound Pt was detectable in the tumor ECF were highly variable. In addition, the unbound Pt concentrations were higher at later time-points in tumor ECF as compared to plasma concentrations in some tumors. A summary of the unbound Pt in tumor ECF, total Pt in tumor extracts, and Pt-DNA adducts after administration of cisplatin, SPI-077, SPI-077 B-103 is presented in Table 2. Mean±SD kP-ECF/VECF and kECF-P were 0.003±0.002 h−1/l/m2 and 3.8±1.3 h−1, respectively, after administration of cisplatin. Mean±SD unbound Pt AUCECF was 0.72±0.31 μg/ml·h. Mean±SD ratio of unbound Pt AUCECF to unbound Pt AUCP was 0.29±0.18.
There was no detectable Pt in the tumor ECF at 0 to 2 h, 24 to 26 h, 96 to 98 h, and 144 to 146 h after administration of SPI-077 or SPI-077 B-103 (Table 2). Total Pt and Pt-DNA adducts in tumors were detectable at all time-points evaluated after administration of SPI-077 and SPI-077 B-103 (Tables 1 and 2). The peak concentrations of total Pt measured in tumor homogenates were 5-fold greater after administration of SPI-077 than after administration of cisplatin (P<0.05). However, the peak concentrations of Pt-GG and Pt-AG DNA adducts were 3.6-fold lower after administration of SPI-077 than after administration of cisplatin (P<0.05; Table 2).
Discussion
Although the tissue and tumor disposition of pegylated and nonpegylated liposomal anticancer agents have been evaluated [2, 6, 26, 27, 28, 29], this is the first study in which the exposure of encapsulated and released drug in in vitro systems, plasma, and tumors have been evaluated after administration of conventional or STEALTH liposomal formulations of anticancer agents. Previously, we used microdialysis to evaluate the systemic and tumor disposition of Pt after administration of cisplatin to mice bearing murine tumors and human tumor xenografts [19]. However, this is the first study in which the active unbound Pt exposure in tumor ECF and the formation of Pt-DNA adducts after administration of liposomal cisplatin have been compared to that after administration of nonliposomal cisplatin. Administration of SPI-077 and SPI-077 B103 resulted in total Pt tumor concentrations that were 2.2- to 5-fold higher than after administration of cisplatin. However, the total Pt measured is the sum of encapsulated and released Pt. Moreover, there was no detectable Pt in the tumor ECF after administration of SPI-077 or SPI-077 B103, whereas unbound Pt concentrations were detectable in the ECF of all tumors after administration of cisplatin. In addition, the formation of Pt-DNA adducts was approximately 3.5-fold higher after administration of cisplatin than after administration of STEALTH liposomal formulations of cisplatin. Although no unbound Pt was detectable in the tumor ECF after administration of the STEALTH liposomal Pt formulations, Pt-DNA adducts were detectable. This presumably reflects the slow release of Pt into the tumor ECF and uptake of the tumor cells that was below the lower limit of detection of our assay. These results suggest that SPI-077 and SPI-077 B103 distribute into tumors, but release less unbound Pt into tumor ECF and form fewer Pt-DNA adducts than cisplatin.
Doxil and SPI-077 are STEALTH liposomal formulations of doxorubicin and cisplatin, respectively [2, 3, 4, 6, 30, 31, 32]. Doxil is approved for the treatment of AIDS-related Kaposi’s sarcoma and relapsed ovarian cancer [30, 31, 32]. The results of Doxil and SPI-077 preclinical and clinical studies show that both have extended systemic half-lives and exposure durations, higher exposures in liver, spleen, and tumor as measured in tissues homogenates, and reduced toxicity as compared to non-liposomal formulations of doxorubicin and cisplatin [2, 3, 4, 5, 30, 31, 32, 33]. Administration of SPI-077 in phase I and II trials at doses (>320 mg/m2) severalfold greater than the maximum tolerated dose of cisplatin did not result in clinical responses or cisplatin-associated toxicities [5]. In addition, pharmacokinetic studies as part of these trials have shown very low levels of released (i.e., ultrafilterable) Pt in plasma [3, 4, 5]. Thus, an alternative formulation of STEALTH liposomal cisplatin (i.e., SPI-077 B103) with a greater theoretical propensity for the release of cisplatin was developed (Alza Corporation, data on file). However, we were not able to detect released cisplatin in in vitro systems, plasma, or tumor ECF after administration of either formulation of STEALTH liposomal cisplatin. In addition, the in vitro recovery of Pt was similar in studies of cisplatin alone or in combination with SPI-077 or SPI-077 B103. Thus, the presence of SPI-077 or SPI-077 B103 does not alter the recovery of cisplatin. This suggests that our in vivo results were not due to altered recovery of Pt after SPI-077 or SPI-077 B103 administration.
A potential explanation for the differences in pharmacokinetics, toxicity, and antitumor effect of Doxil and SPI-077 may be associated with differences in the characteristics of doxorubicin and cisplatin and the make-up of the liposomal bilayer [12, 34, 35]. The differences in the engineering and formulation of the STEALTH liposomes for Doxil and SPI-077 may explain the differences in release rates and antitumor activity of these liposomal agents. Thus, tumor disposition and release of drug from the liposomal carrier used for various anticancer agents, and different liposomal formulations of the same anticancer agent should be evaluated.
The plasma and tumor disposition of the drug encapsulated in liposomes depends on the physiochemical characteristics of the liposomes (i.e., size, surface charge, membrane lipid make-up and packing process, steric stabilization, and dose) rather than the characteristics of the encapsulated drug [26, 27, 36, 37, 38, 39]. Liposomal agents accumulate in areas, such as tumors, that contain a discontinuous microvasculature or in organs, such as liver or spleen, containing the macrophages of the reticuloendothelial system [36, 38, 40]. The high concentrations of total Pt measured in tumor, liver, and spleen homogenates after administration of STEALTH liposomal formulations are consistent with these prior studies.
The use of liposomal formulations of various anticancer agents (e.g., 9-nitrocamptothecin, topotecan, lurtotecan, and paclitaxel) to enhance the delivery of the drug to the tumor are being evaluated in several pharmaceutical companies and research centers [41, 42, 43, 44, 45, 46, 47]. In addition, other carrier molecules or substances (e.g., PEG) are being developed to achieve greater exposure or disposition of anticancer agents in tumors [48]. However, the processes involved in the delivery of these carriers and the release of the active agent, the variability in these processes, and the degree to which the active agent is released into the tumor ECF or into the tumor cell are unknown. After extravasation, the STEALTH liposomes lodge in the interstitial spaces among tumor cells. Once in the tumor, STEALTH liposomes are localized in the ECF surrounding the tumor cell, but do not enter the cell [26, 27, 28]. Thus, for the STEALTH and other liposomes to deliver the active form of the anticancer agent, such as doxorubicin or cisplatin, the drug must be released from the liposome into the ECF and then diffuse into the cell [26, 27, 28]. As a result, the ability of the liposome to carry the anticancer agent to the tumor and release it into the ECF are equally important factors in determining the antitumor effect of liposomal encapsulated anticancer agents. The kinetics of this local release were unknown as it was difficult to distinguish liposomal encapsulated drug from free drug in solid tissue. The development of microdialysis techniques used in our study allows the differentiation of agents encapsulated in and released from liposomes [13, 14, 15, 16, 17]. The clinical importance of these studies is underscored by the need to select liposomal anticancer agents with high tumor penetration and delivery of the active drug to the tumor. Moreover, we have shown that microdialysis is an effective method to distinguish between liposomally encapsulated drug and released drug, and should be used to evaluate future liposomal and other carrier-mediated drug delivery formulations.
References
Dorr RT, Von Hoff DD (1993) Cisplatin monograph, 2nd ed. In: Dorr RT, Von Hoff DD (eds) Cancer chemotherapy handbook. Appleton and Lange, New York, p 286
Harrington KJ, Lewanski CR, Northcote AD, Whittaker J, Wellbank H, Vile RG, Peters AM, Stewart JS (2001) Phase I-II study of pegylated liposomal cisplatin (SPI-077) in patients with inoperable head and neck cancer. Ann Oncol 12:493
DeMario MD, Vogelzang NJ, Janisch L, Tonda M, Amantes MA, Pendyala L, Ratain MJ (1998) A phase I study of liposome-formulated cisplatin (SPI-077) given every 3 weeks in patients with advanced cancer. Proc Am Soc Clin Oncol 17:883
Veal GJ, Griffin MJ, Price E, Parry A, Dick GS, Little MA, Yule SM, Morland B, Estlin EJ, Hale JP, Pearson AD, Welbank H, Boddy AV (2001) A phase I study in paediatric patients to evaluate the safety and pharmacokinetics of SPI-77, a liposome encapsulated formulation of cisplatin. Br J Cancer 84:1029
Schellens JHM, Meerum Terwogt J, Groenewegen G, Blijham GH, Ten Bokkel Huinink WW, Swart M, Maliepaard M, Floot B, Welbank H, Beijnen JH (1998) Phase I and pharmacologic study of SPI-77, a novel STEALTH liposomal encapsulated formulation of cisplatin (CDDP). Proc Am Assoc Cancer Res 39:2218
Newman MS, Colbern GT, Working PK, Engbers C, Amantea MA (1999) Comparative pharmacokinetics, tissue distribution, and therapeutic effectiveness of cisplatin encapsulated in long-circulating, pegylated liposomes (SPI-077) in tumor-bearing mice. Cancer Chemother Pharmacol 43:1
Gerad H, Egorin MJ, Whitacre M, Van Echo DA, Aisner J (1983) Renal failure and platinum pharmacokinetics in three patients treated with cis-diamminedichloroplatinum(II) and whole-body hyperthermia. Cancer Chemother Pharmacol 11:162
Egorin MJ, Van Echo DA, Tipping SJ, Olman EA, Whitacre MY, Thompson BW, Aisner J (1984) Pharmacokinetics and dosage reduction of cis-diammine(1,1-cyclobutanedicarboxylato)platinum in patients with impaired renal function. Cancer Res 44:5432
Allen TM, Stuart DD (1998) Liposomal pharmacokinetics. Classical, sterically-stabilized, cationic liposomes and immunoliposomes. In: Janoff AS (ed) Liposomes: rational design. Marcel Dekker, New York, p 63
Woodle MC, Lasic DD (1992) Sterically stabilized liposomes. Biochim Biophys Acta 1113:171
Pluim D, Maliepaard M, van Waardenburg RC, Beijnen JH, Schellens JH (1999) 32P-postlabeling assay for the quantification of the major platinum-DNA adducts. Anal Biochem 275:30
Reed E, Saurhoff S, Poirier MC (1998) Quantitation of platinum-DNA binding after therapeutic levels of drug exposure: a novel use of graphite furnace spectrometry. Atom Spectrosc 3:93
Johansen MJ, Newman RA, Madden T (1997) The use of microdialysis in pharmacokinetics and pharmacodynamics. Pharmacotherapy 17:464
Kehr J (1993) A survey on quantitative microdialysis: theoretical models and practical implications. J Neurosci Methods 48:251
Zamboni WC, Houghton PJ, Hulstein JL, Kirstein M, Walsh J, Cheshire PJ, Hanna SK, Danks MK, Stewart CF (1999) Relationship between tumor extracellular fluid exposure to topotecan and tumor response in human neuroblastoma xenograft and cell lines. Cancer Chemother Pharmacol 43:269
Muller M, Mader RM, Steiner B, Steger GG, Jansen B, Gnant M, Helbich T, Jakesz R, Eichler HG, Blochl-Daum B (1997) 5-Fluorouracil kinetics in the interstitial tumor space: clinical response in breast cancer patients. Cancer Res 57:2598
Blochl-Daum B, Muller M, Meisinger V, Eichler HG, Fassolt A, Pehamberger H (1996) Measurement of extracellular fluid carboplatin kinetics in melanoma metastases with microdialysis. Br J Cancer 73:920
Muller M, Schmid R, Georgopoulos A, Buxbaum A, Wasicek C, Eichler HG (1995) Application of microdialysis to clinical pharmacokinetics in humans. Clin Pharmacol Ther 57:371
Zamboni WC, Gervais AC, Egorin MJ, Schellens JH, Hamburger DR, Delauter BJ, Grim A, Zuhowski EG, Joseph E, Pluim D, Potter DM, Eiseman JL (2002) Inter- and intratumoral disposition of platinum in solid tumors after administration of cisplatin. Clin Cancer Res 8:2992
Conley BA, Ramsland TS, Sentz DL, Wu S, Rosen DM, Wollman M, Eiseman JL (1999) Antitumor activity, distribution, and metabolism of 13-cis-retinoic acid as a single agent or in combination with tamoxifen in established human MCF-7 xenografts in mice. Cancer Chemother Pharmacol 43:183
D’Argenio DZ, Schumitzky A (1979) A program package for simulation and parameter estimation in pharmacokinetic systems. Comput Programs Biomed 9:115
Zamboni WC, Luftner DI, Egorin MJ, Schweigert M, Sezer O, Richter T, Natale JJ, Possinger K (2001) The effect of increasing topotecan infusion from 30 minutes to 4 hours on the duration of exposure in cerebrospinal fluid. Ann Oncol 12:119
Gibaldi M, Perrier D (1982) Pharmacokinetics, 2nd edn. Marcel Dekker, New York
Hirsch RP, Riegelman RK (1992) Statistical first aid: interpretation of health research data. Blackwell Scientific, Boston
Rosner B (2000) Fundamentals of biostatistics, 5th edn. Duxbury, Pacific Grove, CA
Harrington KJ, Mohammadtaghi S, Uster PS, Glass D, Peters AM, Vile RG, Stewart JS (2001) Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clin Cancer Res 7:243
Harrington KJ, Rowlinson-Busza G, Syrigos KN, Uster PS, Abra RM, Stewart JS (2000) Biodistribution and pharmacokinetics of 111In-DTPA-labelled pegylated liposomes in a human tumour xenograft model: implications for novel targeting strategies. Br J Cancer 83:232
Harrington KJ, Rowlinson-Busza G, Syrigos KN, Abra RM, Uster PS, Peters AM, Stewart JS (2000) Influence of tumour size on uptake of (111)ln-DTPA-labelled pegylated liposomes in a human tumour xenograft model. Br J Cancer 83:684
Northfelt DW (1994) STEALTH liposomal doxorubicin (SLD) delivers more DOX to AIDS-Kaposi’s sarcoma lesions than to normal skin. Proc Am Soc Clin Oncol 13:51
Stewart S, Jablonowski H, Goebel FD, Arasteh K, Spittle M, Rios A, Aboulafia D, Galleshaw J, Dezube BJ (1998) Randomized comparative trial of pegylated liposomal doxorubicin versus bleomycin and vincristine in the treatment of AIDS-related Kaposi’s sarcoma. International Pegylated Liposomal Doxorubicin Study Group. J Clin Oncol 16:683
Northfelt DW, Dezube BJ, Thommes JA, Miller BJ, Fischl MA, Friedman-Kien A, Kaplan LD, Du MC, Mamelok RD, Henry DH (1998) Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi’s sarcoma: results of a randomized phase III clinical trial. J Clin Oncol 16:2445
Muggia FM, Hainsworth JD, Jeffers S, Miller P, Groshen S, Tan M, Roman L, Uziely B, Muderspach L, Garcia A, Burnett A, Greco FA, Morrow CP, Paradiso LJ, Liang LJ (1997) Phase II study of liposomal doxorubicin in refractory ovarian cancer: antitumor activity and toxicity modification by liposomal encapsulation. J Clin Oncol 15:987
Berry G, Billingham M, Alderman E, Richardson P, Torti F, Lum B, Patek A, Martin FJ (1998) The use of cardiac biopsy to demonstrate reduced cardiotoxicity in AIDS Kaposi’s sarcoma patients treated with pegylated liposomal doxorubicin. Ann Oncol 9:711
Peleg-Shulman T, Gibson D, Cohen R, Abra R, Barenholz Y (2001) Characterization of sterically stabilized cisplatin liposomes by nuclear magnetic resonance. Biochim Biophys Acta 1510:278
Colbern GT, Dykes DJ, Engbers C, Musterer R, Hiller A, Pegg E, Saville R, Weng S, Luzzio M, Uster P, Amantea M, Working PK (1998) Encapsulation of the topoisomerase I inhibitor GL147211C in pegylated (STEALTH) liposomes: pharmacokinetics and antitumor activity in HT29 colon tumor xenografts. Clin Cancer Res 4:3077
Allen TM, Hansen C (1991) Pharmacokinetics of stealth versus conventional liposomes: effect of dose. Biochim Biophys Acta 1068:133
Papahadjopoulos D, Allen TM, Gabizon A, Mayhew E, Matthay K, Huang SK, Lee KD, Woodle MC, Lasic DD, Redemann C (1991) Sterically stabilized liposomes: improvements in pharmacokinetics and antitumor therapeutic efficacy. Proc Natl Acad Sci U S A 88:11460
Drumond DC, Meyer O, Hong K (1991) Optimizing liposomes for delivery of chemotherapeutic agents to solid tumor. Pharmacol Rev 51:692
Working PK, Newman MS, Huang SK (1994) Pharmacokinetics, biodistribution, and therapeutic efficacy of doxorubicin encapsulated in STEALTH liposomes. Liposome Res 46:667
Jain RK (1996) Delivery of molecular medicine to solid tumors. Science 271:1079
Proulx ME, Desormeaux A, Marquis JF, Olivier M, Bergeron MG (2001) Treatment of visceral leishmaniasis with sterically stabilized liposomes containing camptothecin. Antimicrob Agents Chemother 45:2623
Tardi P, Choice E, Masin D, Redelmeier T, Bally M, Madden TD (2000) Liposomal encapsulation of topotecan enhances anticancer efficacy in murine and human xenograft models. Cancer Res 60:3389
Verschraegen CF, Gilbert BE, Huaringa AJ, Newman R, Harris N, Leyva FJ, Keus L, Campbell K, Nelson-Taylor T, Knight V (2000) Feasibility, phase I, and pharmacologic study of aerosolized 9-nitro-20(S)-camptothecin in patients with advanced malignancies in the lungs. Ann N Y Acad Sci 922:352
Desjardins JP, Abbott EA, Emerson DL, Tomkinson BE, Leray JD, Brown EN, Hamilton M, Dihel L, Ptaszynski M, Bendele RA, Richardson FC (2001) Biodistribution of NX211, liposomal lurtotecan, in tumor bearing mice. Anticancer Drugs 12:235
Sharma A, Straubinger RM, Ojima I, Bernacki RJ (1995) Antitumor efficacy of taxane liposomes on a human ovarian tumor xenograft in nude athymic mice. J Pharm Sci 84:1400
Ducan R, Gac-Breton S, Keane R, Musila R, Sat YN, Satchi R, Searle F (2001) Polymer-drug conjugates, PDEPT and PELT: basic principles for design and transfer from laboratory to clinic. J Control Release 74:135
Sharma A, Straubinger RM, Ojima I, Bernacki RJ (1995) Antitumor efficacy of taxane liposomes on a human ovarian tumor xenograft in nude athymic mice. J Pharm Sci 84:1400–1404
Ducan R, Gac-Breton S, Keane R, Musila R, Sat YN, Satchi R, Searle F (2000) Polymer drug conjugates, PDEPT and PELT: basic principles for design and transfer from laboratory to clinic. J Control Release 74:135–146
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zamboni, W.C., Gervais, A.C., Egorin, M.J. et al. Systemic and tumor disposition of platinum after administration of cisplatin or STEALTH liposomal-cisplatin formulations (SPI-077 and SPI-077 B103) in a preclinical tumor model of melanoma. Cancer Chemother Pharmacol 53, 329–336 (2004). https://doi.org/10.1007/s00280-003-0719-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-003-0719-4