Abstract
Acute leukemias of ambiguous lineage (ALAL) are rare hematologic malignancies with poor outcomes. Retrospective studies have suggested that acute lymphoblastic leukemia (ALL) regimens are more effective than acute myeloid leukemia (AML) regimens. We retrospectively examined the effectiveness of the widely-used adult ALL regimen hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (hyperCVAD) as initial therapy in patients with ALAL at five academic institutions. Twenty-five patients were identified, including 23 with mixed phenotype acute leukemia (MPAL) and two with acute undifferentiated leukemia. Five of 8 tested (63%) had FLT3-ITD and 3 of 25 (12%) were Philadelphia chromosome-positive. The complete remission (CR) rate was 76%, with CR with incomplete count recovery (CRi) in an additional 8%, for an overall response rate of 84%. Median number of cycles to CR/CRi was 1. There were no deaths in the first 30 days. Of the 21 patients achieving CR or CRi, 14 (66%) proceeded to allogeneic hematopoietic stem cell transplantation. With a median follow-up time of 31.6 months, median overall survival for the entire cohort was not reached, and the estimated 2-year survival was 63%. HyperCVAD can be considered an effective and tolerable front-line regimen for patients with ALAL, and warrants further prospective study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The vast majority of acute leukemias can be classified as either myeloid or lymphoid, but in approximately 4% of cases [1], traditional immunophenotyping cannot clearly establish differentiation along a single lineage. While several different nomenclature systems, diagnostic algorithms, and classification schemes have been developed over the years, these leukemias can collectively be termed acute leukemias of ambiguous lineage (ALAL). In the most recent World Health Organization (WHO) classification of acute leukemia published in 2016, ALAL can be further categorized into five subgroups: acute undifferentiated leukemia, mixed phenotype acute leukemia (MPAL) with t(9;22) (q34.1; q11.2), MPAL with t(v; 11q23.3), B/myeloid MPAL not otherwise specified, and T/myeloid MPAL not otherwise specified [2]. The prognosis for ALAL is considered poor and appears worse than for either de novo acute myeloid leukemia (AML) or acute lymphoid leukemia (ALL) [3,4,5], with median survival estimates of approximately 18 months and 5-year survival rates of approximately 40% [6, 7]. Outcomes are especially poor in ALAL patients above the age of 75 years, roughly only 20% of whom receive chemotherapy, with 2-year survival rates of approximately 5% [8].
Due to the rarity of ALAL and multiple historical diagnostic criteria, this remains a poorly understood malignancy with no true consensus on optimal therapy. Retrospective studies with somewhat heterogeneous populations suggest that patients with ALAL, including MPAL, have better outcomes when treated with regimens used for ALL rather than AML. Recently, a large metaanalysis of both the pediatric and adult MPAL populations showed that ALL induction was statistically superior to AML induction with respect to complete remission (CR) rate and overall survival (OS) [9]. Based on these data, current expert opinion recommends an ALL-like induction therapy followed by allogeneic hematopoietic stem cell transplantation (alloHSCT) after achievement of remission [10, 11]; however, specific ALL regimens have not been studied extensively in this disease.
In a phase II study in adult patients with ALL, induction chemotherapy with hyperCVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high-dose cytarabine and methotrexate) was associated with a CR rate of 92% a relatively low induction mortality rate of 5%, and a 5-year survival rate of 38% [12]. Compared with a historical cohort of patients receiving VAD regimens, hyperCVAD was superior with respect to CR rate, CR duration, and OS [12, 13]. HyperCVAD is currently one of the National Comprehensive Cancer Network-recommended front-line regimens for adult patients with Philadelphia chromosome (Ph)-negative or -positive ALL, the latter in conjunction with a tyrosine kinase inhibitor (TKI), and is one of the most widely used regimens for adult ALL in the USA [14]. In this study, we retrospectively analyzed the effectiveness of hyperCVAD in the upfront treatment of patients with ALAL.
Methods
Patients
We retrospectively reviewed records from adult (≥ 18 years old) patients initially treated for ALAL with the hyperCVAD chemotherapy regimen at five academic institutions (University of Maryland Greenebaum Comprehensive Cancer Center, Moffitt Cancer Center, Mayo Clinic, Virginia Commonwealth University, and Roswell Park Comprehensive Cancer Center). The study was approved by each institution’s Institutional Review Board. Patients with ALAL, as defined by the 2016 WHO Classification, were identified using each institution’s database or through patient lists obtained from pathology and/or pharmacy. Due to the complexity in establishing the diagnosis, a pathology report from the academic institution was required for the patient to be included in the study. Data collected included age, gender, complete blood counts, percentage of marrow blasts, karyotype, mutations, presence of central nervous system (CNS) involvement, number of cycles, treatment response, time to progression, and time to death. Patients with ALAL with 11q23 rearrangements or t(9;22) were included, with the exception of those with blast-phase chronic myelogenous leukemia with mixed phenotype. Complex karyotype was defined as at least 3 cytogenetic abnormalities. Responses were defined according to modified International Working Group Criteria for acute myeloid leukemia [15].
The primary objective was to estimate CR rate, and secondary objectives included to evaluate the percentage of patients who go on to receive allogeneic hematopoietic stem cell transplant and to estimate the median relapse-free survival (RFS) and OS.
Treatment
All patients who received at least one cycle of hyperCVAD-based chemotherapy as their initial treatment following diagnosis were included. At some institutions, high-dose cytarabine/methotrexate (the “B” or “even” cycle of hyperCVAD) was initiated prior to the CVAD cycle (“A” or “odd” cycle). Patients who received a TKI along with hyperCVAD were included.
Statistical analysis
Descriptive statistics were used for baseline patient and disease characteristics and response rates. OS was measured from day one of chemotherapy until the date of death. RFS was measured from the date of initial confirmed CR until the date of relapse or death. All time-to-event analyses were conducted using the Kaplan-Meier method. Statistical analyses were conducted using IBM SPSS version 24.
Results
Patient demographics and baseline characteristics
Twenty-five patients were identified who fulfilled WHO 2016 Criteria for ALAL and received initial induction with hyperCVAD between January 1, 2002, and February 28, 2017. Pretreatment characteristics are summarized in Table 1. The median age was 49 years, with 13 (52%) female and 12 (48%) male patients. Most patients were Caucasian (80%); 20% were African-American. Most had mixed phenotype acute leukemia (n = 23, 92%); 2 had acute undifferentiated leukemia. Median white blood cell count (WBC) at presentation was 29 k/mcL. Normal and complex karyotypes were seen in seven (28%) patients each, one patient had t(4;11), and three patients had t(9;22). Monosomal karyotype was seen in 3 patients. Monosomy 7 was present in 2 patients, both as part of a complex karyotype. One patient had monosomy 17 as part of a complex karyotype, but no other patients had loss of 17p. Next-generation sequencing was unavailable in 17 patients and incomplete (only FLT3 and NPM1 evaluated) in three patients. FLT3-ITD was detected in 5 of eight patients (63%) tested for this mutation, of whom 3 had B/myeloid and 2 had T/myeloid MPAL. Five patients had more than one mutation. Three (12%) patients had CNS involvement at presentation, and one patient developed CNS disease during the course of therapy.
Response to therapy
The median number of HyperCVAD cycles administered to the entire cohort was 4 (range, 1–8), and the 30-day mortality rate was zero. The CR rate was 76% (n = 19), and an additional 8% (n = 2) had CR with incomplete count recovery (CRi), for an overall response rate (ORR) of 84%. One patient had a partial response (4%), and three patients had no response (14%). Of the 21 patients achieving CR or CRi, median number of cycles to CR was one. All three patients with Ph-positive disease received concurrent dasatinib and achieved CR. Of the five patients who had FLT3 mutations at diagnosis, three of the five achieved CR, and one achieved PR. None received treatment with FLT3 inhibitors during the dose-intensive phase, although the three patients who achieved CR had sorafenib as maintenance therapy, one patient received it during the maintenance phase of hyperCVAD, and two following alloHSCT. All three patients stopped sorafenib within 4 months due to poor tolerance.
Outcomes
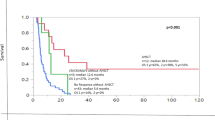
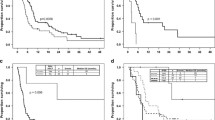
For the entire cohort, 16 (64%) patients were alive and in remission at time of data analysis, and median OS was not reached after a median follow-up time of 31.6 months. Estimated 12-month and 24-month survival was 79% and 63%, respectively (Fig. 1). Without censoring for alloHSCT, median RFS for the 21 patients who achieved CR/CRi was not reached, and estimated 12-month and 24-month RFS was 81% and 64% (Fig. 2). Fifteen patients proceeded to alloHSCT, including 14 of the 21 patients (66%) who achieved CR or CRi, and the estimated 24-month survival was 77%, compared with 64% for the seven responders who did not undergo alloHSCT (p = 0.78). At the time of data analysis, 11 (73%) of the 15 patients who underwent alloHSCT were alive and in remission. Among the patients who did not undergo alloHSCT, two relapsed within 2 months of achieving CR, and four were alive and in remission 10 to 64 months after hyperCVAD initiation. Of the three Ph-positive patients, one proceeded with alloHSCT, and all three patients were alive at 10, 39, and 51 months. The three patients with FLT3 mutations who achieved CR were alive and in remission at 16, 24, and 64 months.
Discussion
To our knowledge, this multiinstitutional retrospective study is the largest series of adult patients with ALAL treated with a single ALL regimen. The hyperCVAD chemotherapy regimen produced high response rates in this rare patient population, and 30-day mortality rate was zero, demonstrating excellent tolerability. Median OS was not reached after a relatively long follow-up period, and alloHSCT was not a requisite for extended survival, as evidenced by a small subset of patients who had good long-term outcomes without undergoing transplant. Although our patient sample size was relatively small, with 25 ALAL patients (the vast majority of whom had MPAL), the CR/CRi rate of 84% and 2-year survival rate of 63% appear favorable relative to the published literature. In the aforementioned metaanalysis of patients with MPAL, the CR rate with ALL induction regimens was 73.9%, and 3-year OS was 48% [9], but over half of the patients were children, who are known to have better outcomes than adults [16,15,16,19].
There were no distinct presenting features in our adult ALAL patient population. WBC at presentation varied widely, ALAL was not more prevalent in either gender, and CNS disease was relatively rare (12%), consistent with previous reports [9, 20]. Aside from t(9;22), our population did not demonstrate any recurrent cytogenetic abnormalities. Our patients had a slightly different distribution of immunophenotypes compared with most other studies on MPAL. While in the literature, B/myeloid and T/myeloid subtypes account for 55–70% [6, 7, 20,19,22], and 30–35% [6, 7, 20] of MPAL, respectively, the T/myeloid subtype was more common in our study population, accounting for 52% of the entire cohort. It is at least possible that this may have contributed to some selection bias, in that individual practitioners may have been more likely to use hyperCVAD as initial therapy for patients with a T/myeloid immunophenotype.
As expected for a study involving intensive chemotherapy for acute leukemia, our population was relatively young with a median age of 49 years. Several studies in the ALL literature have consistently shown the benefit of pediatric-inspired regimens over adult-type regimens in the adolescent and young adult (AYA) population [23,22,23,26], but this issue has not been explored extensively in patients with ALAL or MPAL. Although hyperCVAD is typically considered an adult-type regimen, at least one retrospective study suggests that it is as effective as pediatric-inspired regimens in ALL [27]. In our study, only five patients were age 18–40, which is often considered the age range for the AYA population. Although meaningful conclusions cannot be made with such a small sample size, all five patients achieved a complete remission with hyperCVAD and four of the five were alive and disease-free from 18.5 to 51 months at the time of data analysis. None of our patients were above the age of 70, thus, whether this regimen is effective and tolerable in this subset of patients with very poor outcomes also cannot be determined from our study.
As the vast majority of our patients were treated many years before broad mutational profiling was available, only eight patients had any molecular data to analyze. Interestingly, in contrast to the findings of Yan and colleagues [20], who reported no mutations in FLT3, IDH1, IDH2, or RUNX1 among 117 patients with MPAL, FLT3-ITD mutations were the most common mutation in our MPAL population, present in 5 of 8 patients studied (63%), and IDH2 and RUNX1 mutations were detected in two patients each. Although three of these patients eventually received sorafenib as maintenance therapy, the duration of sorafenib therapy was very short due to intolerance, thus, the role of this agent in ALAL, or specifically MPAL, is uncertain. To our knowledge, the role of newer targeted inhibitors such as midostaurin and gilteritinib for FLT3-mutated disease and enasidenib for IDH2-mutated disease has not been explored.
The role of alloHSCT in the treatment of patients with ALAL, including those who are treated with ALL chemotherapy regimens, remains unclear. Prior large registry studies of patients with MPAL from the Center for International Blood and Marrow Transplant Research (CIBMTR) [28] and the European Society for Blood and Marrow Transplantation (EBMT) [29] reported fairly promising 3-year leukemia-free survival of 56% and 46.5%, respectively, but no control group was available for comparison. Most retrospective studies suggest improved outcomes for patients undergoing alloHSCT compared with consolidation therapy alone [7, 20, 30], but the pediatric and young adolescent population may not benefit from transplantation after achievement of CR1 [17, 18]. We found no significant difference in 2-year OS for patients who received alloHSCT compared to those who did not (77% vs. 64%, respectively, p = 0.78) in our cohort of patients treated with hyperCVAD-based therapy, albeit with a small number of patients and potential selection bias. AlloHSCT is also a time-dependent variable, which further confounds analysis of the true impact of this intervention.
In conclusion, we demonstrate that hyperCVAD is an effective front-line therapy for patients with ALAL and is associated with low induction mortality. Due to the rarity of this disease, clinical trial data to guide optimal therapy are currently lacking, but hyperCVAD appears to be an effective regimen, and may also be an appropriate backbone for incorporation of novel therapies for ALAL in future prospective studies.
References
Van-Den-Ancker W, Terwijn M, Westers TM et al (2010) Acute leukemias of ambiguous lineage: diagnostic consequences of the WHO2008 classification. Leukemia 24:1392–1396
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127:2391–2405
Xu XQ, Wang JM, Lü SQ et al (2009) Clinical and biological characteristics of adult biphenotypic acute leukemia in comparison with that of acute myeloid leukemia and acute lymphoblastic leukemia: a case series of a Chinese population. Haematologica 94:919–927
Khan M, Siddiqi R, Naqvi K (2018) An update on classification, genetics, and clinical approach to mixed phenotype acute leukemia (MPAL). Ann Hematol 97:945–953
Steensma DP (2011) Oddballs: acute leukemias of mixed phenotype and ambiguous origin. Hematol Oncol Clin North Am 25:1235–1253
Matutes E, Pickl WF, Veer MVNT et al (2011) Mixed-phenotype acute leukemia: clinical and laboratory features and outcome in 100 patients defined according to the WHO 2008 classification. Blood 117:3163–3171
Tian H, Xu Y, Liu L, Yan L, Jin Z, Tang X, Han Y, Fu Z, Qiu H, Sun A, Wu D (2016) Comparison of outcomes in mixed phenotype acute leukemia patients treated with chemotherapy and stem cell transplantation versus chemotherapy alone. Leuk Res 45:40–46
Guru Murthy GS, Dhakal I, Lee JY, Mehta P (2017) Acute leukemia of ambiguous lineage in elderly patients – analysis of survival using surveillance epidemiology and end results-Medicare Database. Clin Lymphoma Myeloma Leuk 17:100–107
Maruffi M, Sposto R, Oberley MJ, Kysh L, Orgel E (2018) Therapy for children and adults with mixed phenotype acute leukemia: a systematic review and meta-analysis. Leukemia 32:1515–1528
Wolach O, Stone RM (2016) How I treat mixed-phenotype acute leukemia. Blood 125:2477–2486
Wolach O, Stone RM (2017) Mixed-phenotype acute leukemia: current challenges in diagnosis and therapy. Curr Opin Hematol 24:139–145
Kantarjian H, Thomas D, O’Brien S et al (2004) Long-term follow-up results of hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (hyper-CVAD), a dose-intensive regimen, in adult acute lymphocytic leukemia. Cancer 101:2788–2801
Kantarjian HM, O’Brien S, Smith TL, Cortes J, Giles FJ, Beran M, Pierce S, Huh Y, Andreeff M, Koller C, Ha CS, Keating MJ, Murphy S, Freireich EJ (2000) Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol 18:547–561
NCCN Clinical Practice Guidelines in Oncology, Acute Lymphoblastic Leukemia, Version 2.2019. In: NCCN Website. https//www.nccn.org/professionals/physician_gls/pdf/all.pdf. Updat. May 15, 2019. Accessed Novemb 9, 2019. https://www.nccn.org/professionals/physician_gls/pdf/all.pdf. Accessed 9 Nov 2019
Cheson BD, Bennett JM, Kopecky KJ, Büchner T, Willman CL, Estey EH, Schiffer CA, Doehner H, Tallman MS, Lister TA, Lo-Coco F, Willemze R, Biondi A, Hiddemann W, Larson RA, Löwenberg B, Sanz MA, Head DR, Ohno R, Bloomfield CD, International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia (2003) Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol 21:4642–4649
Al-Seraihy AS, Owaidah TM, Ayas M et al (2009) Clinical characteristics and outcome of children with biphenotypic acute leukemia. Haematologica 94:1682–1690
Hrusak O, De Haas V, Stancikova J et al (2018) International cooperative study identifies treatment strategy in childhood ambiguous lineage leukemia. Blood 132:264–276
Orgel E, Alexander TB, Wood BL, Kahwash SB, Devidas M, Dai Y, Alonzo TA, Mullighan CG, Inaba H, Hunger SP, Raetz EA, Gamis AS, Rabin KR, Carroll AJ III, Heerema NA, Berman JN, Woods WG, Loh ML, Zweidler-McKay PA, Horan JT, for the Children’s Oncology Group Acute Leukemia of Ambiguous Lineage Task Force (2020) Mixed-phenotype acute leukemia: a cohort and consensus research strategy from the children’s oncology group acute leukemia of ambiguous lineage task force. Cancer 126:593–601
Weinberg OK, Seetharam M, Li R et al (2014) Mixed phenotype acute leukemia a study of 61 cases using world health organization and european group for the immunological classification of leukaemias criteria. Am J Clin Pathol 142:803–808
Yan L, Ping N, Zhu M, Sun A, Xue Y, Ruan C, Drexler HG, MacLeod RAF, Wu D, Chen S (2012) Clinical, immunophenotypic, cytogenetic, and molecular genetic features in 117 adult patients with mixed-phenotype acute leukemia defined by WHO-2008 classification. Haematologica 97:1708–1712
Deffis-Court M, Alvarado-Ibarra M, Ruiz-Argüelles GJ, Rosas-López A, Barrera-Lumbreras G, Aguayo-González Á, López-Karpovitch X, López-Hernández M, Velázquez-Sánchez de Cima S, Zamora-Ortiz G, Crespo-Solís E (2014) Diagnosing and treating mixed phenotype acute leukemia: a multicenter 10-year experience in México. Ann Hematol 93:595–601
Shimizu H, Saitoh T, Machida S, Kako S, Doki N, Mori T, Sakura T, Kanda Y, Kanamori H, Miyawaki S, Okamoto S, Kanto Study Group for Cell Therapy (KSGCT) (2015) Allogeneic hematopoietic stem cell transplantation for adult patients with mixed phenotype acute leukemia: results of a matched-pair analysis. Eur J Haematol 95:455–460
Ram R, Wolach O, Vidal L, Gafter-Gvili A, Shpilberg O, Raanani P (2012) Adolescents and young adults with acute lymphoblastic leukemia have a better outcome when treated with pediatric-inspired regimens: systematic review and meta-analysis. Am J Hematol 87:472–478
Stock W, La M, Sanford B et al (2008) What determines the outcomes for adolescents and young adults with acute lymphoblastic leukemia treated on cooperative group protocols? A comparison of children’s cancer group and cancer and leukemia group B studies. Blood 112:1646–1654
Ramanujachar R, Richards S, Hann I, Goldstone A, Mitchell C, Vora A, Rowe J, Webb D (2007) Adolescents with acute lymphoblastic leukaemia: outcome on UK National Paediatric (ALL97) and adult (UKALLXII/E2993) trials. Pediatr Blood Cancer 48:254–261
Boissel N, Auclerc MF, Lhéritier V, Perel Y, Thomas X, Leblanc T, Rousselot P, Cayuela JM, Gabert J, Fegueux N, Piguet C, Huguet-Rigal F, Berthou C, Boiron JM, Pautas C, Michel G, Fière D, Leverger G, Dombret H, Baruchel A (2003) Should adolescents with acute lymphoblastic leukemia be treated as old children or young adults? Comparison of the French FRALLE-93 and LALA-94 trials. J Clin Oncol 21:774–780
Rytting ME, Jabbour EJ, Jorgensen JL, Ravandi F, Franklin AR, Kadia TM, Pemmaraju N, Daver NG, Ferrajoli A, Garcia-Manero G, Konopleva MY, Borthakur G, Garris R, Wang S, Pierce S, Schroeder K, Kornblau SM, Thomas DA, Cortes JE, O'Brien SM, Kantarjian HM (2016) Final results of a single institution experience with a pediatric-based regimen, the augmented Berlin–Frankfurt–Münster, in adolescents and young adults with acute lymphoblastic leukemia, and comparison to the hyper-CVAD regimen. Am J Hematol 91:819–823
Munker R, Brazauskas R, Wang HL, de Lima M, Khoury HJ, Gale RP, Maziarz RT, Sandmaier BM, Weisdorf D, Saber W, Center for International Blood and Marrow Transplant Research (2016) Allogeneic hematopoietic cell transplantation for patients with mixed phenotype acute leukemia. Biol Blood Marrow Transplant 22:1024–1029
Munker R, Labopin M, Esteve J, Schmid C, Mohty M, Nagler A (2017) Mixed phenotype acute leukemia: outcomes with allogeneic stem cell transplantation. A retrospective study from the acute leukemia working party of the EBMT. Haematologica 102:2134–2140
Heesch S, Neumann M, Schwartz S, Bartram I, Schlee C, Burmeister T, Hänel M, Ganser A, Heuser M, Wendtner CM, Berdel WE, Gökbuget N, Hoelzer D, Hofmann WK, Thiel E, Baldus CD (2013) Acute leukemias of ambiguous lineage in adults: molecular and clinical characterization. Ann Hematol 92:747–758
Author information
Authors and Affiliations
Contributions
VHD wrote the protocol, collected, and analyzed the data and had primary responsibility for writing the manuscript. SK participated in analyzing the data and writing the manuscript. KHB, KS, ESW, RC, DAS, ZNS, MRB, and AAK collected data and participated in editing and critically reviewing the manuscript. Availability of data and material Raw deidentified data will be made available upon request and subject to certain criteria, conditions, and exceptions.
Corresponding author
Ethics declarations
Conflict of interest
KS has been on advisory boards for Takeda, Bristol-Myers Squibb, and Novartis; reports honoraria from Astellas and Stemline; and has received research funding from Incyte. ESW has had an advisory role with Abbvie, Astellas, Daiichi Sankyo, Dava Oncology/Arog, Genentech, Jazz, Kite Pharmaceuticals, Kura Oncology, Macrogenics, Pfizer, PTC Therapeutics, and Stemline and has been a speaker for Stemline and Pfizer. All other authors report no relevant conflicts of interest.
Ethics approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. The respective Institutional Review Boards at each study center approved this study. As this was a retrospective study, informed consent could not be obtained from all patients included in the study.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duong, V.H., Begna, K.H., Kashanian, S. et al. Favorable outcomes of acute leukemias of ambiguous lineage treated with hyperCVAD: a multi-center retrospective study. Ann Hematol 99, 2119–2124 (2020). https://doi.org/10.1007/s00277-020-04179-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-04179-z