Abstract
Co-inheritance of triplicated α-genes can alter the clinical and hematological phenotypes of β-thalassemias. We evaluated the phenotypic diversity and transfusion requirements in β-thalassemia heterozygotes, homozygotes, and normal individuals with associated α-gene triplication. Clinical and hematological evaluation was done and the β-thalassemia mutations characterized by a covalent reverse dot blot hybridization/amplification refractory mutation system. Alpha-globin gene triplication was assessed by multiplex PCR. During the last 2.5 years, 181 β-thalassemia patients and β-thalassemia carriers with an unusual clinical presentation were referred to us for screening for the presence of associated α-globin gene triplication. Twenty-nine of them had associated α-gene triplication (3 β-thalassemia homozygotes or compound heterozygotes and 26 β-thalassemia heterozygotes). One β-thalassemia compound heterozygote [IVS 1–5 (G → C) + CD 41/42 (−CTTT)] was anemic at birth and required blood transfusions unusually early by 6 weeks of age. The second patient (4.5 years) was also clinically severe and became transfusion dependent in spite of having one mild β-thalassemia mutation [Capsite +1 (A → C)]. The third case (3.5 years) who was homozygous for a mild β-gene mutation [−88 (C → T)] with α gene triplication was untransfused. The 26 β-thalassemia heterozygotes with associated triplicated α-genes presented variably, with a β-thalassemia intermedia-like presentation. While screening the family members of all these cases, we found another 10 β-thalassemia heterozygotes and 9 normal individuals with α-globin gene triplication; however, all of them were asymptomatic. Beta-thalassemia carriers, homozygotes, and compound heterozygotes with an unusual presentation should be screened for the possible presence of associated α-globin gene triplication which could influence the clinical and hematological presentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beta-thalassemias are a heterogeneous group of autosomal recessive disorders characterized by reduced or absent β-globin chain synthesis. The resulting relative excess of unbound α-globin chains precipitates in erythroid precursors in the bone marrow, leading to their premature death and hence to ineffective erythropoiesis. β-Thalassemia patients have variable clinical phenotypes, ranging from the severe transfusion-dependent thalassemia major to the milder form of thalassemia intermedia. Patients with the major form of the disease have severe microcytic and hypochromic anemia and hepatosplenomegaly and usually come to medical attention within the first 2 years of life [1].
Individuals with β-thalassemia intermedia present later in life with milder anemia that may require occasional transfusions, liver and spleen enlargement, typical bone changes, and mild to moderate jaundice. Few β-thalassemia intermedia patients may become transfusion dependent at a later age. Beta-thalassemia heterozygotes are usually asymptomatic [1]. Triplication of the α-globin genes leads to increased production of α-globin chains. This is usually not a problem in otherwise normal individuals [2, 3]; however, when α-gene triplication is co-inherited with β-thalassemia, there may be sufficient α- and β-globin imbalance to produce a more severe phenotype [1, 2].
We report our experience on the co-inheritance of triplicated α-globin genes and β-thalassemia.
Materials and methods
One hundred and eighty-one individuals (β-thalassemia patients and carriers) with an unusual clinical presentation were referred to us over the last 2.5 years for investigating the possible co-inheritance of additional α-genes with β-thalassemia. They were either β-thalassemia homozygotes or compound heterozygotes who presented with severe anemia very early in life or they were β-thalassemia heterozygotes with a thalassemia intermedia-like presentation.
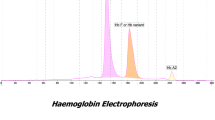
Clinical evaluation was done in all the cases and their past history noted from their medical records. Five to 6 ml of blood was collected in EDTA from all the individuals and their family members who were clinically normal after an informed consent was obtained. The study was approved by our Institutional Ethics Committee. The complete blood count was measured by an automated hematology counter (Sysmex, K-1000, Sysmex Corporation, Kobe, Japan), and the percentage of HbA2 and HbF were measured by HPLC on the Variant Hb Testing System (Bio-Rad Laboratories, Hercules, CA, USA). DNA was extracted from the leucocytes using a standard method. Beta-genotyping was done by covalent reverse dot blot (CRDB) hybridization [4] or by amplification refractory mutation system (ARMS) [5]. Screening for α-gene triplication was done by multiplex PCR [6].
Results
Among the 181 individuals with different β-thalassemia phenotypes evaluated, 29 had triplicated α-globin genes. They included 3 β-thalassemia homozygotes or compound heterozygotes and 26 β-thalassemia heterozygotes. Ten β-thalassemia heterozygotes and 9 normal individuals from the family members who were tested also had α-gene triplication.
The 3 β-thalassemia homozygotes/compound heterozygotes with associated α-globin gene triplication had variable clinical phenotypes. Their hematological and molecular findings are shown in Table 1.
The first case was a 6-week-old female baby who was anemic at birth (Hb 12.1 g/dl) and required transfusions at the age of 6 weeks and subsequently became transfusion dependent. She had inherited a severe β+-thalassemia mutation [IVS 1–5 (G → C)] and a β0-thalassemia mutation [CD 41/42 (−CTTT)] along with the triplicated α-globin gene.
The second case was a 4.5-year-old male child who clinically presented with anemia at the age of 8 months and gradually became transfusion dependent. He had hepatosplenomegaly, and his liver and spleen were palpable 10 cm below the costal margin. He had inherited one mild β++ mutation [Capsite +1 (A → C)] and a β0 mutation [CD 41/42 (−CTTT)] with the triplicated α-globin gene.
The third case was a 3.5-year-old male child who was also anemic at birth (Hb 12.5 g/dl). However, he is untransfused till now and is maintaining a hemoglobin level of around 9 g/dl. His β-globin genotype is β++/β++, being homozygous for a mild β-thalassemia mutation [−88 (C → T)] with co-inherited α-globin gene triplication.
Of the 36 β-thalassemia heterozygotes with triplicated α-globin genes, 26 were clinically symptomatic whereas 10 were asymptomatic. Eighteen of the 26 symptomatic individuals required intermittent transfusions, while 2 of them needed repeated transfusions only during their pregnancy. Fourteen of them had splenomegaly (spleen 4 to 5 cm below the costal margin), hepatomegaly (liver 2–3 cm below the costal margin), or both. One of the 14 cases was splenectomized (spleen 18 cm below the costal margin). One β-thalassemia heterozygote with triplicated α-globin genes was a 3-month-old female baby, heterozygous for the IVS 1–5 (G → C) β+-thalassemia mutation with splenomegaly (spleen 5 cm below the costal margin) and a Hb level of 5.2 g/dl. This child was subsequently transfused once and is now 1 year old. On screening her parents, the mother had β-thalassemia trait and α-globin gene triplication while the father had a normal β genotype but had α-globin gene triplication.
Twenty-one of the 26 symptomatic β-thalassemia heterozygotes had the severe β+ mutation IVS 1–5 (G → C), while 5 of them had β0 mutations [IVS 1–1 (G → T)—1, CD 15 (G → A)—2, and CD 41/42 (−CTTT)—2].
Of the 10 asymptomatic β-thalassemia heterozygotes, 8 had the IVS 1–5 (G → C) mutation, and one case each had the milder Capsite +1 (A → C) and the milder −88 (C → T) mutation, respectively.
We compared the hematological parameters of 26 symptomatic β-thalassemia heterozygotes having α-gene triplication with those of the 10 asymptomatic heterozygotes having α-globin gene triplication as well as with 30 β-thalassemia heterozygotes with a normal α genotype.
Their hematological and molecular findings and requirements of blood transfusion are shown in Table 2.
The group of symptomatic β-thalassemia heterozygotes with α-globin gene triplication had significantly lower (p ≤ 0.05) Hb levels and higher HbF levels as compared to the asymptomatic group of heterozygotes with α-globin gene triplication. However, no significant difference was observed in the mean Hb level and HbF level with the group of β-thalassemia heterozygotes without α-globin gene triplication. The RBC count was lower in the symptomatic β-thalassemia heterozygotes with α-gene triplication compared to the other two groups. The family members with β-thalassemia trait and α-globin gene triplication were clinically asymptomatic, but they had high RBC counts (3.82–6.08 × 1012/l) and a similar degree of hypochromia and microcytosis as compared to the symptomatic carriers.
Nine individuals with a normal β genotype but with triplicated α-globin genes were also encountered among the family members of these cases. All of them were clinically asymptomatic and their hematological parameters did not show any difference when compared with a group of 30 clinically normal individuals with a normal β and α genotype (Table 3).
Discussion
The different phenotypes of β-thalassemia are mainly distinguished by the clinical severity of the disease. The non-transfusion-dependent thalassemias primarily include cases of β-thalassemia intermedia, HbE-β-thalassemia, and HbH disease. Unlike the β-thalassemia major patients, they do not require regular blood transfusions for survival. Majority of the thalassemia intermedia patients are homozygotes or compound heterozygotes for β-thalassemia, but they could have a single dominant β-thalassemia mutation or concurrent inheritance of an α-gene deletion or triplication or a mutation in the γ-gene [7–9]. Thus, associated primary, secondary, or tertiary modifiers can alter the phenotypic presentation.
Unequal crossing over between the linked α-globin genes on chromosome 16 may generate single or triplicated α-globin genes [1]. The presence of α-globin gene triplications is known to have aggravating effects on the phenotype of β-thalassemia heterozygotes [3, 10–12]. Beta-thalassemia heterozygotes with co-inherited α-globin gene triplication have moderate anemia, and these individuals may also present clinically like β-thalassemia intermedia cases (β-TI) [13, 14]. The effect of a single or a couple of additional α-globin genes in homozygous β-thalassemia cases would aggravate the severity even further; however, this has not been investigated in detail [1].
We identified 29 individuals with triplicated α-genes among 181 β-thalassemia patients and carriers with an unusual clinical presentation who were investigated. Among the 3 β-thalassemia homozygotes/compound heterozygotes with associated α-globin gene triplication, the first case presented unusually early at 6 weeks. β-Thalassemia major cases generally do not present till 3 to 6 months of age. There is, however, some data to indicate that β-thalassemia homozygotes with triplicated α-genes show evidence of hemolytic anemia earlier in life and anticipated transfusion dependency [15]. The β genotype would also influence the clinical presentation. Our second case (Table 1) was transfused 10 times in 4.5 years. The Capsite mutation when associated with a second severe β-gene mutation leads to a varied phenotype, and these patients are often transfusion independent. However, the triplicated α-gene may have further aggravated the condition. The third case was homozygous for a mild β-thalassemia mutation −88 (C → T) with α-gene triplication and has remained untransfused till now (Hb 9.0 g/dl). However, he is only 3.5 years old yet.
β-Thalassemia heterozygotes with associated α-globin gene triplication show a variable phenotype. At one end of the spectrum, they are asymptomatic like most β-thalassemia heterozygotes although they may have slightly higher HbF values. At the other end, some individuals have a picture of mild thalassemia intermedia with hemoglobin values ranging from 8 to 10 g/dl and splenomegaly [1]. The clinical picture of heterozygous β-thalassemia with homozygous α-globin gene triplication has been of a moderate to severe form of thalassemia intermedia, with hemoglobin values in the range of 6–9 g/dl and moderate splenomegaly. In our study, the 3-month-old child, a β-thalassemia heterozygote with severe anemia (Table 2), could have inherited the triplicated α-globin genes from both her parents. As gene dosage studies were not done, we were not able to confirm this. In few earlier studies, the combination of homozygous α-gene triplication with β-thalassemia alleles has resulted in a moderate-to-severe β-thalassemia intermedia presentation with occasional blood transfusion requirements [13, 16, 17]. Fallah et al. [17] reported a 4-year-old child with an ααα/ααα genotype and heterozygous β-thalassemia with the IVS 1–5 (G → C) mutation, who had been transfused once for her anemia. All our symptomatic β-thalassemia heterozygotes had the common Indian β-globin gene mutations of the severe β+ or β0 type associated with a lower output or absence of the synthesis of β-globin chains, whereas the asymptomatic carriers had the β+ and β++ type of mutations with a higher amount of β-globin chain synthesis.
An earlier study showed that HbA2 levels were moderately increased in the presence of α-globin gene triplications, either in association with β-thalassemia [13] or solely [18]. We did not observe this in our study. The HbA2 level in β-thalassemia increases when excess of α-globin chains binds to excess δ-globin chains. As explained earlier in the case of α-globin gene triplication alone, the δ-globin chains are not overexpressed, so the small excess of α-globin chains after binding completely to the δ-globin chains would be eliminated by proteolysis whereas the HbA2 level could be reduced because of the absence of α-globin chains which may in turn lead to proteolysis of the excess δ-globin chains [15].
The prevalence of the presence of α-globin gene triplication in β-thalassemia heterozygotes has been shown earlier to be around 2 % and in normal individuals around 3 % in India [19]. This study shows that α-gene triplication is not that infrequent in Indians and its interaction with a diversity of β-thalassemia mutations leads to variable phenotypes. Hence, the presence of triplicated α-globin genes should always be considered in β-thalassemia homozygotes and heterozygotes with an unusual presentation, which could influence the clinical and hematological presentation.
Abbreviations
- HPLC:
-
High-performance liquid chromatography
- CRDB:
-
Covalent reverse dot blot hybridization
- ARMS:
-
Amplification refractory mutation system
- TI:
-
Thalassemia intermedia
References
Weatherall DJ, Clegg JB. The thalassemia syndromes. 4th Ed. Blackwell Science; 2001.
Camaschella C, Kattamis A, Petroni D (1997) Different haematological phenotypes caused by the interaction of triplicated α-globi. Am J Hematol 55:83–88
Goossens M, Dozy AM, Embury SH, Zachariada Z, Hadjiminas M, Stamatoyannopoulos G et al (1980) Triplicated α-globin loci in humans. Proc Natl Acad Sci USA 77:518–521
Colah R, Goraksahkar A, Lu C, Nadkarni A, Desai S, Pawar N et al (1997) Application of covalent reverse dot blot hybridization for rapid prenatal diagnosis of the common Indian thalassemia syndromes. Indian J Haematol Blood Transfus 15:10
Old JM (2001) DNA based diagnosis of hemoglobin disorders. In: Steinberg MH, Forget BG, Higs DR and Nagel RL (Eds.), Disorders of hemoglobin—genetics, pathophysiology and clinical management. Cambridge University Press 2001; pp 941–948.
Tan A, Quah T, Low P, Chang S (2001) A rapid and reliable 7 deletion multiplex polymerase chain reaction assay for α-thalassemia. Blood 98:250–251
Rachmilewitz E, Giardina P (2011) How I treat thalassemia. Blood 118(13):3479–3488
Musallam K, Taher A, Rachmilewitz E (2012) β thalassemia intermedia: a clinical perspective. Cold Spring Harb Perspect Med 2(7):a013482
Musallam K, Revella S, Vichinsky E, Rachmilewitz E (2013) Non-transfusion dependent thalassemias. Haematologica 98:833–844
Henni T, Belhani M, Morle F, Bachir D, Tabone P, Colonna P et al (1985) α-Globin gene triplication in severe heterozygous β-thalassemia. Acta Haematol 74:236–239
Colah R, Nadkarni A, Mukerjee M, Goraksahkar A, Surve R, Mohanty D (1997) β-Thalassemia heterozygotes with α-globin gene triplication. Br J Hematol 97:506–507
Urbinati F, Madigan C, Malik P (2006) Pathophysiology and therapy for hemoglobinopathies. Part II: thalassemias. Expert Rev Mol Med 8:1–26
Treager- Synodinos J, Kanavakis E, Vrettou C, Maragoudaki E, Michael TH, Metaxotou- Mavromati A et al (1996) The triplicated α- globin gene locus in β-thalassemia heterozygous: clinical, haematological, biosynthetic and molecular studies. Br J Haematol 95:467–471
Panigrahi I, Mahapatra M, Kumar R, Cahudhary VP, Sexsena R (2006) Jaundice and α-gene triplication in β-thalassemia: association or causation? Hematology 11:109–112
Giordano PC, Bakker- Verwij M, Harteveld C (2009) Frequency of α-globin gene triplication and their interaction with β-thalassemia mutations. Hemoglobin 33:124–131
Premawardhena A, Fisher C, Olivieri N, De Silver S, Sloane- Stanley J, Wood W et al (2005) A novel molecular basis for β-thalassemia intermedia poses new questions about its pathophysiology. Blood 106:3251–3255
Fallah M, Zadeh-Vakili A, Aleyasin S, Mahdian R, Karimipour M, Raeisi M et al (2009) Molecular characterization of thalassemia intermedia, due to co-inheritance of homozygous α triplication and IVS-I-5 β-thalassemia. Blood Cell Mol Dis 43:158–160
Paleari R, Giambona A, Cannata M, Leto F, Maggio A, IFCC Working Group Standardization of HbA2 (2007) External quality assessment of hemoglobin A2 measurement: data from an Italian pilot study with fresh whole blood samples and commercial HPLC systems. Clin Chem Lab Med 45:88–92
Nadkarni A, Tamhankar A, Surve R, Shirsat R, Colah R, Gorakshakar A et al (1997) Effect of associated α-thalassemia and α-gene triplication on haematological profile of β-thalassemia heterozygotes and normal individuals. Med Sci Res 25:685–686
Acknowledgments
We are thankful to all the clinicians for referring the patients.
Authorship contributions
PM, DU, and MG carried out the molecular analysis for alpha-gene triplication, and PM wrote the first draft of the manuscript. PS helped with the molecular analysis for β-thalassemia, AN supervised the laboratory work, and CS clinically evaluated the patients. RC designed the study, helped with the analysis of the data, and finalized the manuscript. KG provided inputs for the manuscript. All the authors have read and approved the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mehta, P.R., Upadhye, D.S., Sawant, P.M. et al. Diverse phenotypes and transfusion requirements due to interaction of β-thalassemias with triplicated α-globin genes. Ann Hematol 94, 1953–1958 (2015). https://doi.org/10.1007/s00277-015-2479-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2479-8