Abstract
Ribosomal protein (RP) L23 has been suggested to be a negative regulator of cell apoptosis. In the present study, we analyzed RPL23 expression in 169 patients with myelodysplastic syndrome (MDS) by using real-time PCR. The apoptosis of CD34+ marrow cells was examined by flow cytometry, and the correlation between RPL23 expression levels and apoptosis in CD34+ cells was assessed. We then analyzed the clinical significance of RPL23 expression for predicting disease progression and patient survival as well as therapeutic response in patients administered with a cytarabine, homoharringtonine, and G-CSF (CHG) regimen or decitabine therapy. Increased RPL23 expression was found in patients with higher-risk MDS than in patients with lower-risk disease (p = 0.004). RPL23 expression levels were found being inversely correlated with decreased apoptotic ratio of CD34+ cells in higher-risk patients (r = −0.672, p < 0.001). Compared to patients with normal RPL23 expression levels, those with increased RPL23 expression presented higher rates of transformation to acute myeloid leukemia (p = 0.005) and reduced 2-year survival rates (p = 0.012). Multivariate regression analysis showed that RPL23 expression level was an independent predictor of prognosis, regardless of patient age, IPSS score, or hemoglobin level. Moreover, patients with RPL23 over-expression appeared to have lower response rates to CHG chemotherapy (p = 0.027) but similar response rates to decitabine treatment. In conclusion, the over-expression of RPL23 might confer apoptosis resistance in CD34+ cells, which may lead to disease progression and adverse prognosis in MDS. Increased RPL23 expression was an inverse indicator for CHG regimen, but not for decitabine treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndrome (MDS) comprises a heterogeneous group of clonal hematopoietic stem cell disorders that are characterized by peripheral cytopenias, hypercellular bone marrow (BM), and increased mortality due to the evolution of acute myeloid leukemia (AML) [1]. In lower-risk MDS patients, the significantly increased rate of apoptosis among hematopoietic cells contributes to BM hypercellularity and peripheral cytopenia. By contrast, BM hematopoietic cells in patients with higher-risk MDS demonstrate resistance to apoptosis, and some of these patients subsequently develop AML [2, 3]. However, this apoptotic resistance observed in higher-risk MDS patients is poorly understood.
Ribosomal proteins (RPs) are ubiquitous RNA-binding proteins that are believed to perform multiple auxiliary extraribosomal functions and have been suggested to play a role in the occurrence of cancer [4]. RPL23 is a protein component of the 60 S large ribosomal subunit that interacts functionally with murine double minute 2 protein (MDM2 or HDM2 in humans) [5]. Upon binding to MDM2, RPL23 inhibits MDM2-mediated p53 degradation, thus activating p53 and inducing cellular apoptosis [5, 6]. Intriguingly, RPL23 has also been suggested to be a negative regulator of apoptosis by suppressing the Miz1-induced transcription of the cell cycle inhibitors p15INK4B and p21CIP1 [7]. A microarray analysis conducted by Sridhar et al. [8] supported the antiapoptotic characterization of RPL23 and demonstrated that a substantial number of RP genes, including RPL23, are over-expressed in the CD34+ marrow cells of higher-risk MDS patients (particularly those with transformed MDS). However, the two opposing roles of RPL23 in cellular apoptosis may be the result of differences in individual cells and disease stages.
In this retrospective study, we measured the mRNA expression levels of RPL23 in a large cohort of MDS patients with different disease stages and subtypes. Additionally, this was the first study to analyze the association between RPL23 expression and the rate of apoptosis among CD34+ marrow cells. The results indicated that RPL23 expression was predictive of disease progression and survival. Moreover, considering the significant role of RPL23 in apoptosis, we assessed whether the expression of RPL23 could predict the efficacy of MDS treatments, including a low-dose cytarabine and homoharringtonine priming with granulocyte colony-stimulating factor (G-CSF) (CHG) chemotherapy regimen, which exerts cancer-killing and proapoptotic effects) and decitabine administration (which acts mainly as a hypomethylating agent at low doses).
Patients and methods
Patients
All patients enrolled in this study had been diagnosed with MDS at our department according to the FAB/WHO classification criteria [9, 10] and the minimal diagnostic standards for MDS [11]. The BM samples were obtained at diagnosis of MDS before initiation of any treatment between 2006 and 2011 following approval by the local ethics committee and according to institutional guidelines. Each of the 169 MDS patients and 25 normal donors provided written informed consent. The characteristics of the MDS patients studied are listed in Table 1. As of December 2011, the median follow-up period for these subjects was 24 months (range of 3–52 months).
Real-time quantitative polymerase chain reaction
Total RNA was extracted from 2 ml of bone marrow mononuclear cells (BMNCs) using the RNeasy Mini Kit (QIAGEN, Germany) according to the manufacturer’s instructions. cDNA was synthesized by random priming from 10 μL of total RNA using the RevertAidTM First Strand cDNA Synthesis Kit (Fermentas, Canada) according to the manufacturer’s instructions. The PCR was performed in a final volume of 10 μL, including 1 μL of cDNA, 0.5 μM of each primer, 4 mM MgCl2, and 2 μL of the supplied enzyme mix containing the reaction buffer, FastStart Taq DNA polymerase, and DNA double-strand specific SYBR Green I dye for PCR product detection. The PCR was performed in a fluorescent quantitation PCR cycler (LightCycler, Roche, Switzerland). The primer sequences for RPL23 were as follows: 5′-TGGTGATGGCCACAGTCAAG-3′ (sense) and 5′-GCTACTGGTCCTGTAATGGCAGA-3′ (antisense). The primer sequences for GAPDH were as follows: 5′-GCACCGTCAAGGCTGAGAAC-3′ (sense) and 5′-GTGGTGAAGACGCCAGTGGA-3′ (antisense). The PCR conditions were as follows: a 30-s preincubation at 95°C and then 40 cycles of 15 s at 95°C, 30 s at 62°C, and 30 s at 72°C. The threshold cycle (Ct) value was subsequently determined, and the relative quantification of mRNA expression was calculated using the comparative Ct method. The relative quantification value of the target, which was normalized to that of an endogenous control (GAPDH gene) and relative to that of a calibrator (the mean expression level of normal controls), was expressed as 2−△△Ct (fold difference), where △Ct = Ct of the target gene−Ct of the endogenous control gene (GAPDH), and △△Ct = △Ct of the samples for the target gene−△Ct of the calibrator for the target gene.
Flow cytometry analysis of apoptosis in CD34+ marrow cells in MDS patients
For the flow cytometry analysis, we used the following fluorescent-labeled monoclonal antibodies CD45-PerCP, CD34-APC, and Annexin V-FITC (BD Biosciences, USA), in addition to the corresponding isotype controls. All samples were subjected to flow cytometry analysis within 12 h of collection. A flow cytometer (FACS Calibur, Becton Dickinson, USA) equipped with CellQuest software was used for logarithmic (Log) sampling, and at least 105 cells were acquired and analyzed for each sample. The BMNCs were stained with anti-CD34 conjugated to APC and anti-CD45 conjugated to PerCP at room temperature for 20 min and then stained with 5 μL of Annexin V conjugated to FITC in combination with 2 μL of PI for 15 min. The cells were then washed once and analyzed within 2 h of staining.
CHG regimen or decitabine treatment
Twenty-nine patients with higher-risk MDS accepted treatment with a priming CHG regimen. The CHG chemotherapy regimen consisted of an intravenous continuous infusion of low-dose cytarabine (25 mg/d) (Pharmacia, Italy) and homoharringtonine (1 mg/d) (Minsheng Pharma, Hangzhou, China) in combination with G-CSF (300 μg/d) (Kirinkunpeng, Japan), which was administered by subcutaneous injection from day 0 until peripheral neutrophil counts had recovered to 2.0 × 109/L. G-CSF was administered intermittently when the peripheral white blood cell count increased beyond 20 × 109/L. Thirty-seven patients with higher-risk MDS were treated with decitabine (Johnson & Johnson Inc, USA), which was administered at a dose of 20 mg/m2 by continuous intravenous infusion for 1 h and repeated daily for 5 days. The cycle was repeated every 4 weeks, depending on each patient’s recovery from myelosuppression. BM aspirates were performed 4 weeks after the CHG regimen or decitabine treatment was completed. The treatment response was assessed after two cycles of the CHG regimen or decitabine therapy and was determined according to the standardized response criteria for MDS [12]. Detailed information regarding these treated patients was shown in Table 2.
Statistical methods
Statistical analyses were performed using the Statistical Package for Social Sciences 10.0 (SPSS Inc., Chicago, IL, USA). Two independent sample populations were compared using Student’s t test, and multiple sample populations were compared using one-way ANOVAs. The Pearson χ2 or Fisher’s exact test was applied to compare the enumeration data between groups. The Pearson correlation analysis was used to examine the correlations between two parameters, and the Kaplan–Meier method was used to estimate the median overall survival. The log-rank test was used to compare Kaplan–Meier survival estimates between groups, and the Cox regression analysis was used for the multivariable analysis. p values <0.05 were considered statistically significant.
Results
Patient characteristics
A total of 169 MDS patients, consisting of 103 males and 66 females, were involved in this study. Their median age was 56 years (range 17–86 years). These patients were classified as having MDS with isolated del(5q) (n = 3), refractory anemia (RA) (n = 8), RA with ringed sideroblasts (RAS) (n = 6), refractory cytopenia with multilineage dysplasia (RCMD) (n = 102), RCMD with ringed sideroblasts (RCMD-RS) (n = 6), refractory anemia with excess blasts-1 (RAEB-1) (n = 21), RAEB-2 (n = 13), RAEB in transformation (RAEB-t) (n = 6), chronic myelomonocytic leukemia (CMML)-1 (n = 3), and CMML-2 (n = 1). One hundred thirty-one patients with international prognostic scoring system (IPSS) [13] scores ≤1.0 were included in the lower-risk MDS group (including 14 low-risk and 117 int-1 patients), whereas 38 MDS patients with IPSS scores >1.0 were included in the higher-risk MDS group (22 int-2 and 16 high-risk patients). Detailed information regarding these MDS patients is shown in Table 1. Twenty-nine patients received CHG chemotherapy regimens, and 37 patients received decitabine treatment (Table 2).
RPL23 expression levels were significantly elevated in higher-risk MDS patients
RPL23 mRNA expression levels, as defined by the 2−△△Ct values (mean ± SE), were evaluated for 169 MDS samples. The expression level of RPL23 (2−△Ct) in normal controls was 0.48 ± 0.08. The RPL23 expression levels for patients with various clinical forms of MDS were as follows (in increasing order): CMML patients, 0.25 ± 0.06; 5q-/RA/RAS patients, 0.43 ± 0.08; RCMD/RCMD-RS patients, 0.65 ± 0.07; RAEB-1 patients, 1.21 ± 0.22; RAEB-2 patients, 1.47 ± 0.38; and RAEB-t patients, 2.57 ± 0.77 (F = 10.716, p < 0.001) (Fig. 1). Patients with higher-risk MDS (IPSS scores >1.0) demonstrated increased RPL23 expression levels compared to patients with lower-risk MDS (IPSS scores ≤1.0) (1.49 ± 0.27 vs. 0.83 ± 0.09, t = 2.929, p = 0.004) (Fig. 2).
RPL23 mRNA expression level in patients with MDS and MDS-AML. The RPL23 mRNA expression levels gradually increased from 0.43 ± 0.08 and 0.65 ± 0.07 in patients with 5q-/RA/RAS and RCMD/RCMD-RS, respectively, to 1.21 ± 0.22, 1.47 ± 0.38, and 2.57 ± 0.77 in patients with RAEB-1, RAEB-2, and RAEB-t, respectively (F = 10.716, p < 0.001)
Over-expression of RPL23 was more common in higher-risk MDS patients
We used a cutoff value of 1.0, with samples having a 2−△△Ct values greater than 1.0 considered positive for over-expression. This number for cutoff is in accordance to the Relative Quantification Software (Roche Molecular Diagnostics) Recommendations for the LightCycler. RPL23 over-expression was observed in 51 of the 169 patients (30.2 %). The percentage of RAEB-1/REAB-2/RAEB-t patients with RPL23 over-expression (20/40, 50.0 %) was significantly higher than that of patients with 5q-/RA/RAS (2/17, 11.8 %) or RCMD/RCMD-RS (29/108, 26.9 %) (p = 0.007 and 0.008, respectively). Notably, none of the patients with CMML showed elevated RPL23 expression. Also, 47.4 % (18/38) of patients with higher-risk MDS demonstrated RPL23 over-expression, which was significantly greater than the frequency of over-expression among lower-risk patients (25.2 %, 33 of 131, χ2 = 6.876, p = 0.009).
RPL23 expression levels were inversely correlated with the percentage of apoptotic CD34+ cells
Apoptotic CD34+ marrow cells were detected in 33 cases (Fig. 3a–e), and the percentage of apoptotic CD34+ cells was significantly greater among lower-risk MDS patients than higher-risk MDS patients (34.3 ± 3.1 vs. 11.8 ± 2.4 %, p < 0.001) (Fig. 3f–h). Moreover, in MDS patients, RPL23 expression was significantly inversely correlated with the percentage of apoptotic CD34+ marrow cells (r = −0.672, p < 0.001) (Fig. 4).
Flow cytometric analysis of bone marrow CD34+ cells and apoptosis ratio in CD34+ cells for MDS patients and normal control. (a) On a CD45 vs. side-scatter plot, CD45- positive events (R1) were selected. (b) On a CD34 vs. side-scatter, region R2 represents CD34+ cells (gated by R1). (c) CD45 vs. side-scatter analysis of CD34+ cells gated by R1 and R2. (d) Region R4 represents a blast region (cells gated by R1, R2 and R3). (e) CD45 vs. CD34 analysis of CD34+ cells (R6) gated by R1, R2, R3 and R4. (f–h) Apoptosis ratio in CD34+ cells (gated by R6) was determined on annexin V-FITC versus PI plots. The lower right quadrants in panel f-h represent the apoptotic cells, FITC-Annexin V positive and PI negative. Compared to the apoptotic ratio in CD34+ cells of normal controls (f), the percentage of apoptotic CD34+ cells increased in lower-risk MDS patients (g) and decreased in patients with higher-risk MDS (h)
Over-expression of RPL23 predicted disease progression and poor survival
During a median follow-up period of 24 months (range 3–52 months), 37.1 % (13/35) of patients with RPL23 over-expression progressed to AML, compared to 14.7 % (14/95) of patients with normal RPL23 expression levels (χ2 = 7.803, p = 0.005). Moreover, there was a significant difference in the 2-year survival rates between patients with RPL23 over-expression and patients with normal RPL23 expression levels (49.3 vs. 71.6 %, p = 0.012) (Fig. 5). For patients with lower-risk MDS, the 2-year survival rate of patients with RPL23 over-expression was strikingly lower than that of patients with normal RPL23 expression levels (59.9 vs. 82.1 %, p = 0.005) (Fig. 6a). Among higher-risk patients, the median survival time of patients with RPL23 over-expression was also significantly shorter than that of patients with normal RPL23 expression levels (11 vs. 22 months, p = 0.018) (Fig. 6b). Using multivariate regression analysis, we showed that the RPL23 expression level served as an independent prognostic indicator, regardless of patient age, IPSS score, or hemoglobin level (Table 3).
Overall survival of MDS patients, grouped according to RPL23 expression level. Over a median follow-up period of 24 months (range 3–52 months), the 2-year survival rates of patients with RPL23 over-expression were significantly lower than those of patients with normal RPL23 expression levels (49.3 vs. 71.6 %, p = 0.012)
Overall survival of lower-risk (a) and higher-risk MDS (b) patients, grouped according to RPL23 expression level. Among patients with lower-risk MDS, the 2-year survival rates of those with RPL23 over-expression were significantly lower than those of patients expressing normal levels of RPL23 (59.9 vs. 82.1 %, p = 0.005) (a). Among higher-risk patients, the median survival time of those with RPL23 over-expression was significantly shorter than that of patients expressing normal levels of RPL23 (11 vs. 22 months, p = 0.018) (b)
Patients with elevated RPL23 expression levels achieved lower response rates to CHG regimen chemotherapy but not to decitabine treatment
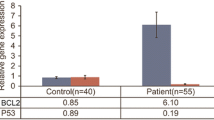
The baseline characteristics (including age, gender, FAB/WHO classification, karyotype, IPSS score) of patients treated with the CHG regimen and decitabine were comparable (p > 0.05) (see Table 2). Of the 29 higher-risk MDS patients who received the CHG chemotherapy regimen, 2 of 14 (14.3 %) patients with RPL23 over-expression experienced complete remission (CR) or marrow CR (CR + mCR) compared to 9 of 15 (60.0 %) patients with normal levels of RPL23 expression (p = 0.027). By contrast, for the 37 patients who received decitabine treatment (median number of courses was 3), there was no difference in the response rates (CR + mCR) between patients with RPL23 over-expression (6/17, 35.2 %) and those with normal expression (5/20, 25.0 %, p > 0.05).
Discussion
This study was the first to show that RPL23 is overexpressed at the mRNA level in higher-risk MDS patients and that elevated RPL23 expression is inversely associated with apoptosis in CD34+ marrow cells. These results support the findings of a cDNA microarray analysis performed by Sridhar et al. [8], who found RPL23 to be associated with poor outcome and MDS transformation to AML. Our findings are also consistent with those of Wanzel et al. [7], who demonstrated that RPL23 is a negative regulator of apoptosis through its suppression of Miz1-induced transcription of the cell cycle inhibitors p15INK4B and p21CIP1. More importantly, we observed that increased RPL23 expression was associated with disease aggressiveness. Compared to patients with normal expression levels of RPL23, patients with increased RPL23 expression levels experienced much higher rates of transformation to AML (p = 0.005) and therefore lower 2-year survival rates (p = 0.012). Furthermore, over-expression of RPL23 correlated with reduced overall survival in both lower-risk and higher-risk MDS patients (as defined by IPSS score). Therefore, these results, in addition to those of the multivariate regression analysis, suggest that RPL23 expression can serve as an independent prognostic indicator, regardless of the age, IPSS score, and hemoglobin level of the patient. The relevance of this protein as an independent negative prognostic factor requires further evaluation and confirmation in a larger cohort of patients and needs to be evaluated prospectively.
In contrast to patients with de novo AML, patients with MDS or MDS-AML typically respond poorly to conventional induction chemotherapy [14, 15], which could be due to the existence of MDS blast cells with primary multidrug resistance (MDR) [16, 17]. It has been reported that RPL23 expression promotes MDR in gastric cancer cells by suppressing drug-induced apoptosis [18], and an enhanced antiapoptotic phenotype among higher-risk MDS patients has been shown to increase CD34+ cell resistance to chemotherapy [19]. Our previous studies showed that the CHG regimen for low-dose chemotherapy was partially effective at treating patients with higher-risk MDS [20, 21], and in the current study, we found that RPL23 over-expression was an inverse indicator of the treatment response to the CHG regimen among higher-risk MDS patients. Patients with elevated levels of RPL23 expression achieved significantly lower response (CR + mCR) rates when compared to those expressing normal levels of RPL23. As the combination of low-dose homoharringtonine and cytarabine has been shown to synergistically induce the apoptosis of blast cells [22], it is conceivable that elevated RPL23 expression (conferring potential apoptosis resistance, as described above) could predict a poor treatment response to CHG chemotherapy. The hypomethylating agent decitabine has demonstrated clinical efficacy in patients with higher-risk MDS [23]. We found that no differences in decitabine treatment response rates between patients with elevated RPL23 expression levels and those with normal RPL23 expression levels. This similar response rate may have been due to the mechanism of action of low-dose decitabine therapy; this treatment is thought to induce re-expression of tumor-suppressive genes via hypomethylation rather than by inducing apoptosis of blast cells [24]. Thus, it is possible that a hypomethylation agent would be more suitable than proapoptotic therapy for the treatment of MDS patients with increased levels of RPL23 expression.
In conclusion, RPL23 over-expression in patients with MDS is associated with abnormal blast resistance to apoptosis, which likely leads to disease progression and a poor prognosis. It is therefore conceivable that RPL23 over-expression could serve as an inverse indication for certain types of chemotherapy, such as the CHG regimen (but not decitabine therapy), in patients with higher-risk MDS.
References
Nimer SD (2008) Myelodysplastic syndromes. Blood 111:4841–4851
Raza A, Gezer S, Mundle S, Gao XZ, Alvi S, Borok R, Rifkin S, Iftikhar A, Shetty V, Parcharidou A et al (1995) Apoptosis in bone marrow biopsy samples involving stromal and hematopoietic cells in 50 patients with myelodysplastic syndromes. Blood 86:268–276
Li X, Bryant E, Deeg HJ (2004) Simultaneous demonstration of clonal chromosome abnormalities and apoptosis in individual marrow cells in myelodysplastic syndrome. Int J Hematol 80:140–145
Warner JR, Mclntosh (2009) How common are extraribosomal functions of ribosomal proteins? Mol Cell 34:3–11
Jin A, Itahana K, O’Keefe K, Zhang Y (2004) Inhibition of HDM2 and activation of p53 by ribosomal protein L23. Mol Cell Biol 24:7669–7680
Dai MS, Zeng SX, Jin Y, Sun XX, David L, Lu H (2004) Ribosomal protein L23 activates p53 by inhibiting MDM2 function in response to ribosomal perturbation but not to translation inhibition. Mol Cell Biol 24:7654–7668
Wanzel M, Russ AC, Kleine-Kohlbrecher D, Colombo E, Pelicci PG, Eilers M (2008) A ribosomal protein L23-nucleophosmin circuit coordinates Mizl function with cell growth. Nat Cell Biol 10:1051–1061
Sridhar K, Ross DT, Tibshirani R, Butte AJ, Greenberg PL (2009) Relationship of differential gene expression profiles in CD34+ myelodysplastic syndrome marrow cells to disease subtype and progression. Blood 114:4847–4858
Delacrétaz F, Schmidt PM, Piguet D, Bachmann F, Costa J (1987) Histopathology of myelodysplastic syndromes. The FAB classification (proposals) applied to bone marrow biopsy. Am J Clin Pathol 87:180–186
Jaffe E, Harris N, Stein H, Vardiman J (2001) World Health Organization classification of tumours. Pathology and genetics of tumours of haematopoietic and lymphoid tissues, ARC, Lyon
Valent P, Horny HP (2009) Minimal diagnostic criteria for myelodysplastic syndromes and separation from ICUS and IDUS: update and open questions. Eur J Clin Invest 39:548–553
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, Pinto A, Beran M, de Witte TM, Stone RM, Mittelman M, Sanz GF, Gore SD, Schiffer CA, Kantarjian H (2006) Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 108:419–425
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, Ohyashiki K, Toyama K, Aul C, Mufti G, Bennett J (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89:2079–2088
Wattel E, De Botton S, Luc Laï J, Preudhomme C, Lepelley P, Bauters F, Fenaux P (1997) Long-term follow-up of de novo myelodysplastic syndromes treated with intensive chemotherapy: incidence of long-term survivors and outcome of partial responders. Br J Haematol 98:983–991
Oosterveld M, Muus P, Suciu S, Koller C, Verhoef G, Labar B, Wijermans P, Aul C, Fière D, Selleslag D, Willemze R, Gratwohl A, Ferrant A, Mandelli F, Cortes J, de Witte T, Estey E, EORTC, EBMT, SAKK, GIMEMA Leukemia Groups and the MD Anderson Cancer Center (2002) Chemotherapy only compared to chemotherapy followed by transplantation in high risk myelodysplastic syndrome and secondary acute myeloid leukemia; two parallel studies adjusted for various prognostic factors. Leukemia 16:1615–1621
Poulain S, Lepelley P, Preudhomme C, Cambier N, Cornillon J, Wattel E, Cosson A, Fenaux P (2000) Expression of the multidrug resistance-associated protein in myelodysplastic syndromes. Br J Haematol 110:591–598
Kurata M, Hasegawa M, Nakagawa Y, Abe S, Yamamoto K, Suzuki K, Kitagawa M (2006) Expression dynamics of drug resistance genes, multidrug resistance 1 (MDR1) and lung resistance protein (LRP) during the evolution of overt leukemia in myelodysplastic syndromes. Exp Mol Pathol 81:249–254
Shi Y, Zhai H, Wang X, Han Z, Liu C, Lan M, Du J, Guo C, Zhang Y, Wu K, Fan D (2004) Ribosomal proteins S13 and L23 promote multidrug resistance in gastric cancer cells by suppressing drug-induced apoptosis. Exp Cell Res 296:337–346
Suárez L, Vidriales MB, García-Laraña J, Sanz G, Moreno MJ, López A, Barrena S, Martínez R, Tormo M, Palomera L, Lavilla E, López-Berges MC, de Santiago M, de Equiza ME, Miguel JF, Orfao A (2004) CD34+ cells from acute myeloid leukemia, myelodysplastic syndromes, and normal bone marrow display different apoptosis and drug resistance-associated phenotypes. Clin Cancer Res 10:7599–7606
Wu L, Li X, Su J, Chang C, He Q, Zhang X, Xu L, Song L, Pu Q (2009) Effect of low-dose cytarabine, homoharringtonine and granulocyte colony-stimulating factor priming regimen on patients with advanced myelodysplastic syndrome or acute myeloid leukemia transformed from myelodysplastic syndrome. Leuk Lymphoma 50:1461–1467
Wu L, Li X, Su J, He Q, Zhang X, Chang C, Pu Q (2011) Efficacy and safety of CHG regimen (low-dose cytarabine, homoharringtonine with G-CSF priming) as induction chemotherapy for elderly patients with high-risk MDS or AML transformed from MDS. J Cancer Res Clin Oncol 137:1563–1569
Jin J, Jiang DZ, Mai WY, Meng HT, Qian WB, Tong HY, Huang J, Mao LP, Tong Y, Wang L, Chen ZM, Xu WL (2006) Homoharringtonine in combination with cytarabine and aclarubicin resulted in high complete remission rate after the first induction therapy in patients with de novo acute myeloid leukemia. Leukemia 20:1361–1367
Steensma DP, Baer MR, Slack JL, Buckstein R, Godley LA, Garcia-Manero G, Albitar M, Larsen JS, Arora S, Cullen MT, Kantarjian H (2009) Multicenter study of decitabine administered daily for 5 days every 4 weeks to adults with myelodysplastic syndromes: the alternative dosing for outpatient treatment (ADOPT) trial. J Clin Oncol 27:3842–3848
Ng KP, Ebrahem Q, Negrotto S, Mahfouz RZ, Link KA, Hu Z, Gu X, Advani A, Kalaycio M, Sobecks R, Sekeres M, Copelan E, Radivoyevitch T, Maciejewski J, Mulloy JC, Saunthararajah Y (2011) p53 independent epigenetic-differentiation treatment in xenotransplant models of acute myeloid leukemia. Leukemia 25:1739–1750
Acknowledgments
This project was funded by the National High Technology Research and Development Program (“863”Program) of China (item no. 2012AA02A505).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, L., Li, X., Xu, F. et al. Over-expression of RPL23 in myelodysplastic syndromes is associated with apoptosis resistance of CD34+ cells and predicts poor prognosis and distinct response to CHG chemotherapy or decitabine. Ann Hematol 91, 1547–1554 (2012). https://doi.org/10.1007/s00277-012-1486-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-012-1486-2