Abstract
Autoreactive cytotoxic T cells play a key role in the pathogenesis of aplastic anemia (AA) by myelosuppressive cytokines including interferon-gamma, tumor necrosis factor alpha, and transforming growth factor beta. The purpose of this study is to determine which single nucleotide polymorphisms (SNPs) in cytokine genes were relevant to AA risk and whether the relevant SNPs were associated with response to immunosuppressive therapy (IST). Among 84 screened patients, 80 patients confirmed as having acquired AA, and 84 age- and sex-matched healthy controls were analyzed consecutively. We genotyped ten polymorphisms in three cytokine genes (IFNG, TNF, and TGFB1) and FAS gene. We assessed the association between polymorphisms and AA risk, and the association between polymorphisms and response to IST in three genetic models (dominant, recessive, and additive). The IFNG −2,353 T allele (dominant model, OR = 0.43, p = .012) and TCA haplotype (dominant model, OR = 0.50, p = .038) were significantly associated with the development of AA. In addition, this relevant IFNG −2,353 T allele and TCA haplotype were related to the response of IST (dominant model, OR = 0.076, p = .034). Concerning TGFB1, although its polymorphisms are not related to AA susceptibility, P10L T allele (recessive model, OR = 0.18, p = .038) and CT haplotype (dominant model, OR = 5.68, p = .038) were associated with response to IST. This exploratory study concurred with prior studies indicating that polymorphisms in IFNG are related to AA susceptibility. In addition, it was found that polymorphisms in IFNG and TGFB1 are associated with response to IST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunosuppressive therapy (IST) is one of the main treatment modalities for acquired aplastic anemia (AA). Approximately 70% of AA patients improve with IST consisting of antithymocyte globulin (ATG) and cyclosporine, and this response rate supports the immunogenic pathophysiology of AA [1–4]. Recent studies suggested that autoreactive cytotoxic T cells play a key role in the pathogenesis of AA by myelosuppressive cytokines including interferon-gamma (IFN-γ) and tumor necrosis factor alpha [5, 6]. These cytokines induce apoptosis in hematopoietic stem cells, partially through the Fas-dependent pathway [7, 8]. Other studies have demonstrated that decreased expression of transforming growth factor beta (TGF-β), an inhibitor of T cells, contributes to the underlying T cell-mediated marrow destruction in AA [9, 10].
Previous reports that discussed genetic polymorphisms of cytokines have focused on the role of susceptibility to AA [11–15]. These studies suggest that AA may arise in genetically susceptible minority with rare disease-causing variants. However, establishing whether these genotyped single nucleotide polymorphisms (SNPs) are functionally relevant to causality is challenging. If the genetic polymorphisms of cytokines showed significant association with the risk of susceptibility to AA and the rate of response, it would support the immunogenic association of causality.
In this study, we conducted an analysis to determine which SNPs in cytokine genes were relevant to AA risk and whether the relevant SNPs were associated with response to IST.
Patients and methods
Among 84 screened patients, 80 patients were confirmed as having acquired AA at Seoul National University Hospital and were analyzed consecutively in this study. Four patients were excluded; one was diagnosed with hypoplastic myelodysplastic syndrome, and the others were suspicious for early stage AA but recovered spontaneously soon after diagnosis. DNA collection was performed between January 2000 and December 2008. All samples were treated anonymously. The control group was composed of 84 unrelated healthy Korean subjects matched for age and sex with no history of autoimmune or hematologic disease.
The diagnosis of AA was based on bone marrow biopsy and peripheral blood cell counts according to the criteria of the International Aplastic Anemia Agranulocytosis Study Group [16]. Severe AA was defined as a bone marrow cellularity of less than 30% and severe pancytopenia with at least two of the following peripheral blood count criteria: (1) absolute neutrophil count (ANC) <0.5 × 109/L; (2) absolute reticulocyte count (ARC) <20 × 109/L; and (3) platelet count <20 × 109/L [17]. Patients fulfilling the criteria for severe AA and having ANCs <0.2 × 109/L were classified as very severe AA [18].
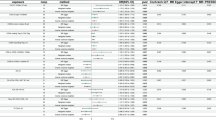
The eligibility for IST with the combination of horse ATG (h-ATG) and cyclosporine included patients with non-severe AA who were transfusion-dependent, patients with non-severe AA who had significant neutropenia, and patients with severe or very severe AA who were not eligible for stem cell transplantation. The hematologic response at 3 and 6 months following initial ATG was adopted from the criteria for response, which is summarized in Table 1. Responses were confirmed by two or more blood counts at least 4 weeks apart [19]. Patient characteristics considered relevant to the response to IST were age, sex, severity of AA, absolute lymphocyte count (ALC), ARC, and platelet count [20].
The study was performed according to the Declaration of Helsinki guidelines for biomedical research and was approved by the Institutional Review Board of Seoul National University Hospital (IRB No: H-0811-012-261).
Genetic polymorphisms
We selected three cytokine genes (IFNG, TNF, and TGFB1) and FAS, which are known to be involved in T cell-mediated marrow destruction. In these four genes, we chose ten polymorphisms based on allelic frequency higher than 0.05 in Asians and the assumption of clinical relevance from previously reported associations. Methods for genotyping assay are provided in the Electronic supplementary material. Imputation of missing genotype was not applied. We estimated individual haplotypes of the three cytokine genes by using the expectation maximization algorithm (PHASE program, ver.2.0.2).
Data analysis
To assess the association between polymorphisms and risk of AA, we calculated statistical differences in allele, genotype, and haplotype distributions between patients and healthy controls by using the Chi-square test in three genetic models (dominant, recessive, and additive). In the analysis of haplotypes of interest, two frequent haplotypes of each gene were included, and others were grouped together. To examine whether each SNP site was in Hardy–Weinberg equilibrium (HWE), the distributions of observed genotype frequency and expected genotype frequency were compared using the Chi-square test (p > 0.05).
To analyze the association between polymorphisms and response to IST, we used multivariate logistic regression analyses of three genetic models. We used dichotomous outcomes defined as response (complete or partial) or non-response. Patients who did not complete 3 or 6 months of initial IST due to stem cell transplantation or who required a second round of IST were considered as non-responders. All response outcomes in the multivariate analysis were adjusted for age, gender, severity, ALC, and ARC.
All statistical analyses were performed using the Stata Software, version 11 (Stata Corp, College Station, TX, USA). Statistical results with p values less than 0.05 were regarded as significant. Because this study was exploratory, the adjustment for multiple comparisons was not applied.
Results
Patients
The baseline characteristics of the AA patients and the controls are shown in Table 2. Of the total 80 AA patients, there were 44 (55%) who had received the h-ATG-based IST. At 3 and 6 months following IST, 43 patients were evaluable for response, and one patient was lost to follow-up. Among the 43 evaluable patients, 24 (56%) showed response to IST at 3 months. Five additional patients (12%) who had not responded at 3 months showed response at 6 months (Fig. 1). The genotype frequencies of ten SNPs in four genes were in Hardy–Weinberg equilibrium in patients and controls.
The association between cytokine polymorphisms and the risk of AA
In this study, association with AA susceptibility was assessed for ten SNPs in IFNG, TNF, TGFB1, and FAS and their frequent haplotypes (Table 3). Among them, one SNP and one haplotype in IFNG were significantly associated with the development of AA (IFNG −2,353 A/T); the presence of the minor T allele in the dominant model was protective and related to a 2.3-fold reduction in the risk for AA (p = 0.012), and the presence of the IFNG TCA haplotype was related to a 2-fold reduced risk for AA (p = 0.038). In terms of other SNPs and haplotypes, they did not show significant associations with the risk of AA.
The association between cytokine polymorphisms and response to IST
The results of the multivariate logistic regression analysis for the response to IST at 3 and 6 months according to genetic polymorphisms are summarized in Table 4. In terms of two SNPs in TGFB1, TGFB1 P10L T/C was significantly related; the T allele (recessive model) was related to a 4.3-fold reduced response to IST at 3 months (p = 0.038). The response was related to the TGFB1 haplotype; the presence of the CT haplotype (dominant model) was favorable to IST and was related to a 5.7-fold higher response at 3 months compared with the response in patients without the CT haplotype (p = 0.038).
The IFNG −2,353 minor T allele was shown to induce resistance to IST; the presence of the T allele and TCA haplotype in IFNG (dominant model) was related to a 13.2-fold reduced hematologic response at 6 months following initial IST (P = 0.034). The TC haplotype homozygote in TGFB1 (recessive model) was related to a 4.6-fold reduced response to IST at 6 months (P = .036). However, four SNPs and two haplotypes in TNF did not show any significant associations with response at 3 and 6 months.
Discussion
Our study reports that the genetic polymorphisms of IFNG are associated with susceptibility to the development of AA and furthermore are associated with hematologic response to initial IST. Concerning TGFB1, although its polymorphisms are not related to AA susceptibility, they are associated with response to IST.
These findings are consistent with previous functional implications of increased IFNG expression during the pathogenesis of AA [5, 6, 21]. Additionally, the finding that AA patients with intracellular IFN-γ expression in peripheral lymphocytes showed almost 3-fold higher response to IST than patients without IFN-γ—expressing lymphocytes (p < 0.0001) supports the immunogenic association of responsiveness [6]. In terms of relationships between genetic polymorphisms and AA susceptibility, a polymorphic CA microsatellite marker in the first intron and its related SNP (IFNG +874 A/T) have demonstrated effects on AA susceptibility [11, 12]. Furthermore, these polymorphisms were found to be associated with the level of IFN-γ production [22, 23].
However, although several studies reported that TNF −308 G/A was significantly related to AA susceptibility [12, 13] and therapeutic response to IST [14], candidate SNPs in our study did not show any association with AA susceptibility or response to IST. Regarding TGF-β, the functionality of polymorphisms in TGFB1 has rarely been reported [24]. However, the significant relationship between TGFB1 polymorphisms and therapeutic response to IST in our study suggests their late effects on marrow suppression.
To our knowledge, this is the first study to identify that genetic variants of key cytokines responsible for AA are involved in both disease susceptibility and clinical response in consecutive analyses. Moreover, the polymorphisms (IFNG −2,353 A/T, TGFB1 P10L T/C) in our study were firstly reported regarding their roles in AA. The possibility of spurious associations was minimized through the selection of matched control and adjustment for potential confounders [20].
In addition, our results may help explain the variability of response to IST in AA. Prediction of responsiveness to IST based on pathophysiology would be useful in the clinical setting. Patients with a high probability of response might be treated first with IST rather than conventional marrow transplantation, which may reduce the significant morbidity and mortality of this disease.
From this study, however, we cannot conclude whether the genetic variants of cytokines can be used as risk factors or predictive markers of AA. Our significantly associated polymorphisms, IFNG −2,353 A/T and TGFB1 P10L T/C, have not been investigated for their effects on IFNG and TGFB1 expression, respectively, and our study used a retrospective design with a small number of patients in Asian population. Moreover, though the associated polymorphisms in this study are frequent in Caucasian population, the observed relationship has not been investigated in other populations.
In conclusion, this exploratory study concurred with prior studies indicating that polymorphisms in IFNG are related to AA susceptibility. In addition, it was found that polymorphisms in IFNG and TGFB1 are associated with response to IST. Further studies in other population by a larger prospective design are needed to better elucidate the determinants of risk of AA and responsiveness to IST.
References
Young N, Calado R, Scheinberg P (2006) Current concepts in the pathophysiology and treatment of aplastic anemia. Blood 108:2509
Bacigalupo A, Bruno B, Saracco P, Di Bona E, Locasciulli A, Locatelli F, Gabbas A, Dufour C, Arcese W, Testi G, Broccia G, Carotenuto M, Coser P, Barbui T, Leoni P, Ferster A (2000) Antilymphocyte globulin, cyclosporine, prednisolone, and granulocyte colony-stimulating factor for severe aplastic anemia: an update of the GITMO/EBMT study on 100 patients. European Group for Blood and Marrow Transplantation (EBMT) Working Party on Severe Aplastic Anemia and the Gruppo Italiano Trapianti di Midolio Osseo (GITMO). Blood 95:1931–1934
Fuhrer M, Rampf U, Baumann I, Faldum A, Niemeyer C, Janka-Schaub G, Friedrich W, Ebell W, Borkhardt A, Bender-Goetze C (2005) Immunosuppressive therapy for aplastic anemia in children: a more severe disease predicts better survival. Blood 106:2102–2104
Locasciulli A, Oneto R, Bacigalupo A, Socie G, Korthof E, Bekassy A, Schrezenmeier H, Passweg J, Fuhrer M (2007) Outcome of patients with acquired aplastic anemia given first line bone marrow transplantation or immunosuppressive treatment in the last decade: a report from the European Group for Blood to Marrow Transplantation (EBMT). Haematologica 92:11–18
Dufour C, Corcione A, Svahn J, Haupt R, Battilana N, Pistoia V (2001) Interferon gamma and tumour necrosis factor alpha are overexpressed in bone marrow T lymphocytes from paediatric patients with aplastic anaemia. Br J Haematol 115:1023–1031
Sloand E, Kim S, Maciejewski JP, Tisdale J, Follmann D, Young NS (2002) Intracellular interferon-gamma in circulating and marrow T cells detected by flow cytometry and the response to immunosuppressive therapy in patients with aplastic anemia. Blood 100:1185–1191
Maciejewski J, Selleri C, Anderson S, Young NS (1995) Fas antigen expression on CD34+ human marrow cells is induced by interferon gamma and tumor necrosis factor alpha and potentiates cytokine-mediated hematopoietic suppression in vitro. Blood 85:3183–3190
Killick SB, Cox CV, Marsh JC, Gordon-Smith EC, Gibson FM (2000) Mechanisms of bone marrow progenitor cell apoptosis in aplastic anaemia and the effect of anti-thymocyte globulin: examination of the role of the Fas-Fas-L interaction. Br J Haematol 111:1164–1169
Li MO, Flavell RA (2008) TGF-beta: a master of all T cell trades. Cell 134:392–404
Rizzo S, Killick SB, Patel S, Ball SE, Wadhwa M, Dilger P, Gordon-Smith EC, Gibson FM (1999) Reduced TGF-beta1 in patients with aplastic anaemia in vivo and in vitro. Br J Haematol 107:797–803
Dufour C, Capasso M, Svahn J, Marrone A, Haupt R, Bacigalupo A, Giordani L, Longoni D, Pillon M, Pistorio A, Di Michele P, Iori AP, Pongiglione C, Lanciotti M, Iolascon A (2004) Homozygosis for (12) CA repeats in the first intron of the human IFN-gamma gene is significantly associated with the risk of aplastic anaemia in Caucasian population. Br J Haematol 126:682–685
Gidvani V, Ramkissoon S, Sloand EM, Young NS (2007) Cytokine gene polymorphisms in acquired bone marrow failure. Am J Hematol 82:721–724
Peng J, Liu C, Zhu K, Zhu Y, Yu Y, Li J, Hou M, Chen X, Xu C, Zhang M (2003) The TNF2 allele is a risk factor to severe aplastic anemia independent of HLA-DR. Hum Immunol 64:896–901
Demeter J, Messer G, Schrezenmeier H (2002) Clinical relevance of the TNF-alpha promoter/enhancer polymorphism in patients with aplastic anemia. Ann Hematol 81:566–569
Takaku T, Calado RT, Kajigaya S, Young NS (2009) Interleukin-23 receptor (IL-23R) gene polymorphisms in acquired aplastic anemia. Ann Hematol 88:653–657
Anonymous (1987) Incidence of aplastic anemia: the relevance of diagnostic criteria. By the international agranulocytosis and aplastic anemia study. Blood 70:1718–1721
Camitta B, Thomas E, Nathan D, Santos G, Gordon-Smith E, Gale R, Rappeport J, Storb R (1976) Severe aplastic anemia: a prospective study of the effect of early marrow transplantation on acute mortality. Blood 48:63
Bacigalupo A, Hows J, Gluckman E, Nissen C, Marsh J, Van Lint M, Congiu M, De Planque M, Ernst P, McCann S (1988) Bone marrow transplantation (BMT) versus immunosuppression for the treatment of severe aplastic anaemia (SAA): a report of the EBMT* SAA Working Party. Br J Haematol 70:177–182
Camitta BM (2000) What is the definition of cure for aplastic anemia? Acta Haematol 103:16–18
Scheinberg P, Wu CO, Nunez O, Young NS (2009) Predicting response to immunosuppressive therapy and survival in severe aplastic anaemia. Br J Haematol 144:206–216
Nistico A, Young NS (1994) Gamma-Interferon gene expression in the bone marrow of patients with aplastic anemia. Ann Intern Med 120:463–469
Pravica V, Asderakis A, Perrey C, Hajeer A, Sinnott PJ, Hutchinson IV (1999) In vitro production of IFN-gamma correlates with CA repeat polymorphism in the human IFN-gamma gene. Eur J Immunogenet 26:1–3
Pravica V, Perrey C, Stevens A, Lee JH, Hutchinson IV (2000) A single nucleotide polymorphism in the first intron of the human IFN-gamma gene: absolute correlation with a polymorphic CA microsatellite marker of high IFN-gamma production. Hum Immunol 61:863–866
Fermo E, Bianchi P, Barcellini W, Pedotti P, Boschetti C, Alfinito F, Cortelezzi A, Zanella A (2004) Immunoregulatory cytokine polymorphisms in Italian patients affected by paroxysmal nocturnal haemoglobinuria and aplastic anaemia. Eur J Immunogenet 31:267–269
Acknowledgment
This study was supported by grant title “The impact of genetic polymorphism on the prevalance and treatment outcomes of aplastic anemia” from the Korea Cancer Research Foundation and by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (0405-BC02-0604-0004).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table 1
Primer sets and Tm for the SNaPshot assay. (DOC 76 kb)
Rights and permissions
About this article
Cite this article
Lee, YG., Kim, I., Kim, J.H. et al. Impact of cytokine gene polymorphisms on risk and treatment outcomes of aplastic anemia. Ann Hematol 90, 515–521 (2011). https://doi.org/10.1007/s00277-010-1102-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-010-1102-2