Abstract
Background
The anterolateral triangle around the cavernous sinus is a surgical skull base triangle used as a neurosurgical landmark essential to skull-based surgeries. There are few reports of its measurements with little attention paid to anatomical variations.
Methodology
A total of 15 adult human cadaveric skulls were dissected to expose the anterolateral triangle on both sides. The triangle was defined and measurements of the three borders were taken precisely and the area of each triangle was calculated using Heron’s formula.
Results
On an average, the length of the anteromedial border is 11.4 (+ 2.2 mm); the length of the posteromedial border is 8.7 (+ 2.6 mm); the length of the lateral border is 13.06 (+ 2.6 mm) and the area of the anterolateral triangle is 48.05 (+ 17.5 mm2).
Conclusion
Concise understanding of anterolateral triangle is essential to skull-based surgeries; comprehending its anatomy helps with better surgical planning and provides insight into local pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
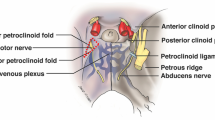
The literature refers to a total of twelve surgical triangles surrounding the cavernous sinus (CS) and in the middle cranial fossa (MCF). The cranial nerves II–VI, which serve as vital anatomical landmarks for neurosurgeons operating on the skull base, generally delineate the limits of these triangles [1]. Parkinson was the first to identify the triangle created by the trochlear and ophthalmic nerves in the lateral wall of the CS in the middle of the 1960s to securely reach the internal carotid artery (ICA) lesion [2]. Following this, a few anatomical and surgical studies revealed several triangles related to the CS that are clinically significant, especially to neurosurgeons [3, 4]. Ten triangles are of neurosurgical importance which are mentioned in the literature and are classified into three categories (Fig. 1) [1].
Classification of the neurosurgical triangles in the middle cranial fossa surrounding the cavernous sinus [17]
In the present cadaveric study, we aimed to compare the dimensions of the anterolateral triangle (ALT) of the MCF bilaterally in 15 adult donated cadavers. Dolenc first described the triangle as the ‘lateral triangle’ in 1989, and it has since undergone several nomenclature revisions [5]. There are a very few studies in the literature that have clearly delineated and quantified the ALT. The ALT is bounded anteromedially by posterior border of maxillary nerve, postero-medially by anterior border of mandibular nerve and laterally by a line connecting the foramen rotundum to the foramen ovale [6, 7]. The triangle contains the lateral wing of the sphenoid and the nerve of the pterygoid canal (Vidian nerve) [8]. The nerve of the pterygoid canal can reliably be tracked in the triangle as it courses posteriorly near the mandibular division of the trigeminal nerve, which in turn serves as a landmark to approach the petrous part of the ICA [9]. The lateral and anterior aspect of the cavernous part of the ICA and the lateral wall of sphenoidal sinus can also be accessed via the ALT [10]. It is feasible to endoscopically see the inferomedial temporal dura of the MCF through the ALT, which makes it a significant corridor for endoscopic endonasal approaches to the MCF [11, 12]. The ALT also serves as a corridor for anterior infratemporal fossa approach for any infraorbital, maxillary, and pterygoid tumours [10, 13]. Hence, intimate understanding of the ALT is essential to skull-based surgery; knowing its anatomy and variations aids in surgical planning and understanding of regional pathology. The ALT’s boundaries have been well-defined and evaluated only in a few studies [4, 7]. To better access the pathological alterations within and around this area, it is also necessary to first understand the dimensions of the ALT. Hence, we anticipate that this study may aid neurosurgeons and clinicians in better comprehending surgical approaches surgical approaches to the CS and MCF by completing the knowledge about the dimensions of the ALT of the middle cranial fossa.
Methodology
The present study was conducted on 15 adult donated human cadavers (9 females and 6 males) (Table 1), with age ranging from 75 to 80 years in the Department of Anatomy, All India Institute of Medical Sciences Bibinagar, Hyderabad. All donors or their relatives provided informed written consent prior to their death so that their bodies can be utilised for medical education and research. As the study was conducted on donated cadavers, exemption from review was taken from Institutional Ethics Committee (IEC).
During routine dissection and practical teaching of undergraduate medical students, after careful removal of brain, duramater overlying the floor of the MCF was removed with utmost care in order to expose underlying structures. In order to do the morphometric study of triangles of MCF, we tried to preserve the trigeminal ganglion and its three divisions. Fine dissection was done to define the boundaries of the ALT on both the sides of the skull base in each of the 15 cadavers. The triangle was bounded antero-medially by posterior border of the maxillary nerve which extended from its intersection with the medial margin of mandibular nerve to the posterior most border of the foramen rotundum (a in Figs. 2, 3). The postero-medial boundary was formed by anterior border of the mandibular nerve, which was measured from its intersection with the maxillary nerve to the anterior most end of the foramen ovale (b in Figs. 2, 3). The lateral boundary was formed by a line joining the foramen rotundum to foramen ovale (c in Figs. 2, 3). Each border of the ALT was measured three times by one author; average of the three was taken as final measurement. All the measurements were made by the same author to avoid subjective variation. Measurements were taken with the help of geometric divider, keeping its pointed ends on the ends of margins to be measured (Fig. 4a, b). Utmost care was taken to ensure that the exact distance between the pointed ends of the divider with which dimensions were measured on the specimen remain undisturbed whilst it was being transferred to the ruler for the measurements. With the help of Heron’s formula, area of each triangle was calculated (as mentioned below). The results were statistically analysed for mean, range and standard deviation. The student’s t test was used to compare each parameter on the right and left side.
Middle cranial fossa (MCF) of right side-superolateral view, showing Right Antero-Lateral Triangle (ALT) bounded antero-medially by posterior border of Maxillary nerve (a), posteromedially by anterior border of Mandibular nerve (b) and laterally by a line (c) joining middle of foramen rotundum (FR) to middle of foramen ovale (FO). ICA1: Internal carotid artery in cavernous sinus (Cavernous part), ICA2: Para clinoidal of Internal carotid artery (Cut end), ACP: Anterior Clinoid Process, ON: Optic Nerve, PTB: Petrous Temporal Bone, TG: Trigeminal Ganglion
Middle cranial fossa (MCF) of left side-superolateral view, showing Left Antero-Lateral Triangle (ALT) bounded antero-medially by posterior border of Maxillary nerve (a), postero-medially by anterior border of Mandibular nerve (b) and laterally by a line (c) joining middle of foramen rotundum to middle of foramen ovale. CS: Cavernous sinus, TG: Trigeminal Ganglion, MMA: Middle meningeal artery, PG: Pituitary Gland in sella turcica
Method used for measuring the boundaries of Anterolateral triangle of Middle Cranial Fossa (MCF)-Superolateral view. A Using geometric divider, keeping its pointed ends on the ends of margins to be measured. B Distance between two points FR (Foramen rotundum) and FO (Foramen ovale) marked on the ruler and measurements noted for three sides of triangles. TG: Trigeminal ganglion, ACF: Anterior Cranial Fossa, MCF: Middle cranial fossa, PCF: Posterior cranial fossa

Results
The lengths of the anteromedial border (along the maxillary nerve) ranged from 8 to 16 mm, with a mean length and standard deviation of 11.4 mm and 2.2 mm, respectively. The lengths of the posteromedial border (along the mandibular nerve) ranged from 4 to 14 mm, with a mean length and standard deviation of 8.7 mm and 2.6 mm, respectively. The lengths of the lateral border (from foramen rotundum to foramen ovale) ranged from 7 to 18 mm, with a mean length and standard deviation of 13.06 mm and 2.6 mm, respectively, the area of the ALT observed was 48.05 + 17.5 mm2 (Table 2). In the 15 formalin fixed cadavers dissected, no statistically significant difference was observed in the measurements related to the boundaries of the ALT of the CS between the right and the left side (p > 0.05) (Table 3).
Discussion
Advanced brain surgery is moving towards endovascular and emerging radiosurgery due to their high level of safety and quick recovery times. The ALT is one of the ten CS surgical triangles and an important anatomical landmark for skull base surgeons [14]. Three components must be clarified in relation to the authors' methodology, two of which deal with measurements and one with nomenclature. To prevent bias, one of the authors carried out all the measurements. When all three sides of a triangle are known, the area may be easily calculated using the Heron's formula. The authors followed Rhoton's naming scheme when referring to the nomenclature of the triangle [15].
In the present study, the length of the anteromedial border observed was 11.4 (± 2.2 mm); the length of the posteromedial border was 8.7 (± 2.6 mm); the length of the lateral border was 13.06 (± 2.6 mm) and the area of the ALT calculated was 48.05 ± 17.5 mm2. We found only four original studies in the literature that have defined and measured the ALT.
In the study done by Watanabe et al. the mean length of the antero-medial border was reported as 13.9 (± 3.1 mm), which is somewhat longer than our study. However, the postero-medial border, the lateral border and the area reported by them as 7.6 (± 2.9 mm), 15.5 (± 2.3 mm), 49.8 ± 15.5 mm2, respectively are almost similar to our study [4]. Granger et al. in his study documented that the mean lengths of the antero-medial, postero-medial, lateral borders were 8.3 ± 2.2 mm, 5.9 ± 2.0 mm, 11.5 ± 2.9 mm, respectively and the mean area was 20.46 ± 9.30 mm2 [8]. This is contradictory to our study, with almost all their measurements were shorter to our findings. On the other hand, in the study done by Isolen et al. they documented that the mean lengths of the anteromedial, posteromedial, lateral borders were 12.25 ± 0.67 mm, 10.80 ± 1.12 mm, 11.59 ± 1.61 mm, respectively and the mean area was 51.52 ± 4.25 mm2, the measurements were longer than what we reported [7]. Dolci et al. instead of using divider and vernier callipers, used stereotaxy and predetermined coordinates to calculate the area of the ALT. Their study yielded an average area of 47.27 ± 5.27 mm2, the findings of which are almost similar to our study [16]. The comparison table for the morphometry of ALT is given in Table 4.
We speculate that different levels of maxillary nerve and mandibular nerve dissection and the force exerted upon retracting the duramater over the MCF might be the cause of these measurement discrepancies. To overrule the subjective variations that will be unavoidably encountered during the dissection, in future, the cadaveric findings should be correlated with the radiological studies for enabling efficient selection of optimal surgical approaches to the MCF through this critical corridor.
The normal architecture of the triangles surrounding the CS are crucial to the approach of CS lesions as they serve as the lesions' natural access points. The surgeon must be well aware of the sizes of these geometric spaces whenever disease or surgical procedures may cause distortions. Intracavernous aneurysms do not significantly impair the precise identification of crucial landmarks when dissecting these anatomical gateways to the MCF, but certain cases of CS neoplasia that may produce a high degree of anatomical distortion. The surgeon must also be aware that mobilising the cranial nerves may cause the triangles to expand [17].
Conclusion
The triangle serves as a critical window in endoscopic endonasal surgeries and for gaining access to other middle fossa structures. It enables the surgeon to navigate around neurological lesions whilst identifying important structures located nearby. Understanding these anatomical landmarks and their individual diameters is essential for recognising the pathology and preventing injuries to adjacent structures. Hence, determining the dimensions of the ALT is critical to better access the pathological changes within and around this area. We anticipate that our findings will extend the understanding of this important surgical triangle and associated structures in radiology, anatomy education, and surgical training.
Availability of data and materials
Data and material related to the report will be available with the corresponding author for further reference.
References
Rhoton AL (2002) The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery 51(4):S375-410
Parkinson D (1965) A surgical approach to the cavernous portion of the carotid artery. Anatomical studies and case report. J Neurosurg 23(5):474–483. https://doi.org/10.3171/jns.1965.23.5.0474
Bayatli E, Cömert A (2023) Scratching in the minefield: using intertriangles line to safely perform anterior petrosectomy. Surg Radiol Anat 45:513–522. https://doi.org/10.1007/s00276-023-03131-w
Watanabe A, Nagaseki Y, Ohkubo S, Ohhashi Y, Horikoshi T, Nishigaya K et al (2003) Anatomical variations of the ten triangles around the cavernous sinus. Clin Anat N Y N 16(1):9–14. https://doi.org/10.1002/ca.10072
Dolenc V, Rogers L (2009) Cavernous sinus: developments and future perspectives. Springer, London. ISBN 13: 9783211101636. https://www.abebooks.com/9783211721377/Cavernous-Sinus-Developments-Future-Perspectives-3211721371/plp
Chavez-Herrera VR, Campero Á, Ballesteros-Herrera D et al (2023) Microsurgical and illustrative anatomy of the cavernous sinus, middle fossa, and paraclival triangles: a straightforward, comprehensive review. SurgRadiol Anat 45:389–400. https://doi.org/10.1007/s00276-023-03105-y
Isolan GR, Krayenbühl N, de Oliveira E, Al-Mefty O (2007) Microsurgical anatomy of the cavernous sinus: measurements of the triangles in and around it. Skull base. Off J North Am Skull Base Soc Al 17(6):357–367. https://doi.org/10.1055/s-2007-985194
Granger A, Bricoune O, Rajnauth T, Kimball D, Kimball H, Tubbs RS et al (2018) Anterolateral triangle: a cadaveric study with neurosurgical significance. Cureus 10(2):e2185. https://doi.org/10.7759/cureus.2185
Kassam AB, Vescan AD, Carrau RL, Prevedello DM, Gardner P, Mintz AH et al (2008) Expanded endonasal approach: vidian canal as a landmark to the petrous internal carotid artery. J Neurosurg 108(1):177–183. https://doi.org/10.3171/JNS/2008/108/01/0177
Kassam AB, Gardner P, Snyderman C, Mintz A, Carrau R (2005) Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus 19(1):6
Kasemsiri P, Solares CA, Carrau RL, Prosser JD, Prevedello DM, Otto BA et al (2013) Endoscopic endonasal transpterygoid approaches: anatomical landmarks for planning the surgical corridor. Laryngoscope 123(4):811–815. https://doi.org/10.1002/lary.23697
Komatsu F, Oda S, Shimoda M, Imai M, Shigematsu H, Komatsu M et al (2014) Endoscopic endonasal approach to the middle cranial fossa through the cavernous sinus triangles: anatomical considerations. Neurol Med Chir (Tokyo) 54(12):1004–1008. https://doi.org/10.2176/nmc.oa.2014-0092
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL (2005) Expanded endonasal approach: the rostrocaudal axis. Part .I Crista galli to the sella turcica. Neurosurg Focus 19(1):3
Dalgiç A, Boyaci S, Aksoy K (2010) Anatomical study of the cavernous sinus emphasizing operative approaches. Turk Neurosurg 20(2):186–204. https://doi.org/10.5137/1019-5149.JTN.2343-09.1
Rhoton AL (2002) The supratentorial cranial space: microsurgical anatomy and surgical approaches. Neurosurgery 51(4):S1-3. https://doi.org/10.1097/00006123-200210001-00001
Dolci RLL, Upadhyay S, Ditzel Filho LFS, Fiore ME, Buohliqah L, Lazarini PR et al (2016) Endoscopic endonasal study of the cavernous sinus and quadrangular space: anatomic relationships. Head Neck 38(1):1680–1687. https://doi.org/10.1002/hed.24301
Kawase T, van Loveren H, Keller JT, Tew JM (1996) Meningeal architecture of the cavernous sinus: clinical and surgical implications. Neurosurgery 39(3):527–534. https://doi.org/10.1097/00006123-199609000-00019. (Discussion 534–536)
Acknowledgements
We deeply appreciate the cadavers' family members who gave their loved ones' corpses for scientific study. We also want to thank the technical staff of our cadaveric laboratory for their assistance.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: AK. Data acquisition: RM, AK. Data analysis or interpretation: RM, AK. Drafting of the manuscript: RM, AK, MC. Critical revision of the manuscript: RM, AK, MC. Approval of the final version of the manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no any conflict of interest.
Consent for publication
All the authors gave consent for the publication of the report.
Ethics approval and consent to participate
This is a cadaveric study that is completely done on donated cadavers, used for teaching and research purpose. All donors or their relatives provided informed written consent prior to their death so that their bodies can be utilised for medical education and research. As the study was conducted on donated cadavers, exemption from review was taken from Institutional Ethics Committee (IEC).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaliappan, A., Motwani, R. & Chandrupatla, M. Anterolateral surgical triangle of the cavernous sinus: a cadaveric study of neurosurgical importance. Surg Radiol Anat 46, 41–46 (2024). https://doi.org/10.1007/s00276-023-03261-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03261-1