Abstract
Purpose
It is well known that many anastomoses can join the external carotid system and the ophthalmic artery. However, their frequency has never been reported. Since they can be relevant for interventional radiologists operating in the orbit, we decided to illustrate and determine the frequency of the anastomoses that can be found in children.
Methods
A retrospective study of 443 angiographic procedures (via ophthalmic artery and/or external carotid artery) carried out on 97 children affected by intraocular retinoblastoma was made to investigate the arterial anatomy of 106 orbits.
Results
Anastomoses were observed in 44.33 % of orbits. However, their true frequency is likely much higher as the rate of visualization increased up to 91.11 % of orbits when the angiographic study was extended to the external carotid artery. In order of frequency we detected the following anastomoses: lacrimal artery—middle meningeal artery, lacrimal artery—anterior deep temporal artery, ophthalmic artery—middle meningeal artery, ophthalmic artery—facial artery, supraorbital artery—superficial temporal artery, supratrochlear artery—superficial temporal artery, supraorbital artery—middle meningeal artery, dorsal nasal artery—infraorbital artery, supraorbital artery—zygomaticoorbital artery, lacrimal artery—zygomaticoorbital artery.
Conclusion
When properly searched, anastomoses between the ophthalmic artery and the external carotid artery are almost constant in children. Depending on the clinical scenario, they can represent dangers or valuable alternative routes for collateral circulations and intraarterial chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known to angiographists and anatomists that the territory supplied by the ophthalmic artery (OA) is a sort of border zone between the internal and the external carotid systems [10]. In fact, though the OA arises from the internal carotid artery and acts as the major axis distributing blood to the intraorbital organs, the blood supply of the orbit is not always sustained exclusively by the internal carotid artery. This is due to several anastomoses that connect the OA (or its collaterals) to branches of the external carotid artery (ECA). Thus, if in most cases the blood within the OA runs from the internal carotid artery with a centrifuge course, sometime the flow can be reversed depending on the hemodynamic requirements of the moment or on chronically established vascular pathologies [4, 8]. Many of these anastomoses have been frequently reported either in the anatomical or in the angiographic literature [10, 15, 21, 25, 28]. However, to the best of our knowledge, a dedicated and systematic study of the transorbital anastomotic pathways occurring between the internal and the external carotid systems through the OA and its branches has never been carried out. Furthermore, and possibly even more important, data on the frequency of such anastomoses are lacking or they are incomplete [15]. A more detailed knowledge of the anastomotic pathways joining the OA and the external carotid system has a great importance for ophthalmologists and angiographists who want to have a clear picture of the vascular anatomy of the orbit. It is also important for interventional radiologists who may want to inject drugs into orbital arteries to reach specific targets [12, 19, 27] or may need to treat vascular-related disorders with the embolization of the external carotid territory [11]. These considerations prompted us to manage a retrospective study using angiographic material conserved in our archives. The material selected from the archives was restricted to children affected by intraocular retinoblastomas. As the location of the tumors was always confined within the globe, the pathology was not supposed to alter the regular orbital hemodynamic.
The angiographies employed in this investigation, belonging to very young patients, gave us also the chance to outline an anatomoradiological study of the transorbital anastomoses as they physiologically occur before the development of age-related atherosclerotic lesions can alter the regular orbital hemodynamic. Besides illustrating many different examples of transorbital anastomotic pathways, this investigation also provides first systematic data on their frequency. We believe that this report can be found useful by interventional radiologists and ophthalmologists operating in the field.
Materials and methods
The present investigation consists of a retrospective study of a series of angiographies carried out on patients affected by intraocular retinoblastoma and selected for intraarterial injection of antitumoral agents. A selective angiography of the internal carotid artery and a superselective angiography of the OA were carried out before and after drug injection. In some patients the selective angiography of the ECA and/or the superselective angiography of its branches was/were also required as the blood flow of the OA was inadequate for drug infusion. The arterial anatomy of the orbits was studied to detect all the transorbital anastomotic pathways occurring between the internal and external carotid systems and to determine their rate of recurrence. From June 2008 to December 2014, a series of 97 patients (mean age at the first treatment: 27.84 ± 21.38 months) with 106 eyes affected by retinoblastoma were selected for intraarterial injection of melphalan or melphalan and topotecan. The parents of all patients gave their informed consent. On the whole, they underwent a total of 443 pharmacologic procedures. Before proceeding with the injection of the antitumoral drugs, an acceptable choroidal blush had to be obtained. To this aim, two different types of angiographic study were carried out: (i) in many cases a good choroidal blush had been easily achieved with the mere superselective angiography of the OA; (ii) in other cases, when the choroidal blush obtained through the OA was not convincing, the angiographic study had been extended to the ECA and/or of its rami to look for anastomotic pathways that allowed the choroidal blush. Accordingly, angiographic examinations were also retrospectively divided into two groups: group 1 consisted of 61 orbits examined exclusively through the superselective angiography of the OA; group 2 gathered 45 orbits in which the angiographic study was carried out, not only through the OA, but it was also extended to the ECA and/or its branches. This distinction was intended to evaluate if different angiographic approaches were more or less suitable to unveil the anastomoses. For radioprotection, radiographic projections were almost always limited to the lateral one. Only in three instances an antero-posterior projection was required for a better understanding of the orbital vascular anatomy.
Results
Several anastomoses between the internal and the external carotid systems were observed in the orbit of our young patients. Listed in order of frequency, we detected the following connections: lacrimal artery-middle meningeal artery, lacrimal artery-anterior deep temporal artery, OA-middle meningeal artery, OA-facial artery, supraorbital artery-superficial temporal artery, supratrochlear artery-superficial temporal artery, supraorbital artery-middle meningeal artery, dorsal nasal artery-infraorbital artery, supraorbital artery-zygomaticoorbital artery, lacrimal artery-zygomaticoorbital artery. In addition, though they do not connect the external and the internal carotid systems, we observed anastomoses between the meningolacrimal artery and the anterior deep temporal artery.
Overall, we could demonstrate anastomoses in 47 orbits (44.33 % of cases). However, as 17 orbits (16.04 % of cases) showed more than one anastomotic pathway, the total number of anastomoses observed was 70. More in detail, 2 co-existent anastomotic pathways were observed in 13 orbits whereas patterns with 3 or 4 anastomoses were both detected in two orbits.
Depending on their course, anastomoses could be split into two main categories: anastomoses at the orbital apex, likely running through the superior orbital fissure, and anastomoses located in the anterior orbit. Results are summarized in Table 1.
Anastomoses at the orbital apex
These anastomoses were the most common (38 cases, 54.28 % of all anastomoses) and always involved the middle meningeal artery that was connected with the lacrimal artery in 22 cases, the OA in 15 cases, and the supraorbital artery in one case. Anastomoses with the lacrimal artery were achieved by the joining of the sphenoid artery (also referred to as orbital branch of the middle meningeal artery) to the recurrent meningeal branch (Fig. 1) which is known to pass through the superior orbital fissure [9, 21, 22]. Overall this anastomosis was found in 20.75 % of orbits; however, when considering the different types angiographic study the frequency of detection was 37.77 % in group 2 (17 orbits out of 45) and only 8.19 % (5 orbits out of 61) in group 1.
Anastomosis between the middle meningeal artery and the lacrimal artery. a Superselective angiography of the sphenoid branch of the middle meningeal artery; early phase. An anastomosis joins the sphenoid artery (sph) and the recurrent meningeal branch (rmb) stemming from the first segment of the lacrimal artery (lac). b Superselective angiography of the sphenoid branch of the middle meningeal artery; later phase. The reflux of contrast medium into the middle meningeal artery (mm) demonstrates the true origin of the sphenoid artery (sph). At the same time, the progression of the contrast medium within the lacrimal artery (lac) injects a muscular branch (mb) of the lacrimal artery arising opposite to the recurrent meningeal branch (rmb) and, with a retrograde flow, the OA (oph). c Superselective angiography of the OA. The angiography of the OA (oph) does not show the lacrimal artery whose blood flow is retrograde
Direct anastomoses between the middle meningeal artery and the OA involved an anastomotic channel known as meningoophthalmic artery [6, 21]. This type of anastomosis was observed in 14.15 % of orbits. Again, when considering the different types of angiographic study the frequency of detection was remarkably different: 31.11 % (14 orbits out of 45) in group 2 and only 1.63 % (1 orbit out of 61) in group 1. The meningoophthalmic artery showed a variable caliber (Fig. 2) as it could be a very thin vessel or such a large vessel to represent, depending on the circumstances and the direction of the blood flow, a second OA stemming from the middle meningeal artery, after Hayreh’s report [15], or a middle meningeal artery arising from the OA.
Three cases of meningoophthalmic arteries (anastomoses between the middle meningeal artery and the OA) of different caliber. a, b Case 1; c, d Case 2; e–h Case 3. a Superselective angiography of the middle meningeal artery; early phase. The middle meningeal artery (mm) detaches an anterior ramus, the meningoophthalmic artery (mo) that enters the orbit and joins the OA (oph). b Superselective angiography of the middle meningeal artery; later phase. The contrast medium has progressed through the meningoophthalmic (mo) artery and diffuses into the OA (oph). c Superselective angiography of the meningoophthalmic artery; early phase. The catheter, pushed along the middle meningeal artery, has been placed into the meningoophthalmic artery (mo) which is seen in all its length. d Superselective angiography of the meningoophthalmic artery; later phase. The contrast medium injected into the meningoophthalmic artery (mo) medium diffuses directly into the OA (oph). The lacrimal artery (lac), stemming from the OA, is also visible. e Selective angiography of the internal carotid artery. The OA is not visible. f Selective angiography of the ECA. The contrast medium reaches the OA (oph) with a retrograde flow via a large meningoophthalmic artery (mo) stemming from the middle meningeal artery (mm). g Superselective angiography of the meningoophthalmic artery; early phase. The meningoophthalmic artery (mo) is seen ending directly into the OA (oph). h Superselective angiography of the meningoophthalmic artery; later phase. Once into the OA (oph), the contrast medium diffuses distally into the branches of the OA including the lacrimal artery (lac)
The anastomosis connecting the middle meningeal artery with the supraorbital artery was very similar to those joining the middle meningeal artery to the lacrimal artery. However, because of a rare early origin of the supraorbital artery, the anastomosis ended into this artery rather than into the lacrimal artery that stemmed more distally (Fig. 3).
Double anastomosis between the middle meningeal artery and the supraorbital artery and between the anterior deep temporal artery and the lacrimal artery. a Superselective angiography of the OA. In contrast to the usual branching pattern, the OA (oph) gives off the supraorbital artery (so) before detaching the lacrimal artery (lac). An anastomotic artery (aa) arises from the supraorbital artery. b Selective angiography of the ECA; early phase. The middle meningeal artery (mm) detaches an orbital branch (ob) which ends giving off an anastomotic artery (aa). The anterior deep temporal artery (adt) gives origin to a lacrimal branch that anastomoses with the lacrimal artery (lac). c Selective angiography of the ECA; later phase. This angiogram demonstrates that the anastomotic artery (aa) seen in a and b is the same vessel joining the orbital branch (ob) of the middle meningeal artery (mm) and the supraorbital artery (so). The contrast medium flowing from the anterior deep temporal artery (adt) through the anastomosis visible also in b diffuses with a retrograde flow along the lacrimal artery (lac)
Anastomoses in the anterior orbit
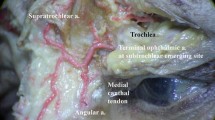
This collection of anastomoses was observed only when the angiographic study was extended to the ECA (i.e. it was observed only in the examinations belonging to group 2). Though they always passed through the anterior orbital opening or traversed the zygomatic bone, the anastomoses located in the anterior orbit encompassed several possibilities. The most common anastomotic pathway occurred between the lacrimal artery and the anterior deep temporal artery (Figs. 3, 4a–c). Overall we could observe it in 15 cases (14.15 % of orbits). Within group 2, the frequency of detection was 33.33 % (15 orbits out of 45 orbits). The anastomosis was realized via the zygomaticotemporal artery of the lacrimal artery that, piercing the zygomatic bone, reached the temporal fossa and joined the anterior deep temporal artery (Fig. 4a–c).
a–c Double anastomoses between the anterior deep temporal artery and the lacrimal artery, and between the infraorbital artery and the dorsal nasal artery. d Anastomosis between the facial artery and the dorsal nasal artery. a Superselective angiography of the OA. The ophthalmic artery OA (oph) has a regular branching pattern which includes the anterior ethmoidal artery (ae). b Selective angiography of the ECA; early phase. The anterior deep temporal artery (adt) ends into the lacrimal artery (lac). At the same time, the infraorbital artery (io) gives off an ascending branch (aa) that anastomoses with the dorsal nasal artery (dn). c Selective angiography of the ECA; later phase. This angiogram confirms the identity of the arteries seen in B. The anterior ethmoid artery (ae) (confront with a) becomes visible since the contrast medium has flowed backwards from the dorsal nasal artery (dn). The contrast medium from lacrimal artery (lac) diffuses with a retrograde flow into the OA (oph). The anterior deep temporal artery (adt) and the anastomotic vessel (aa) of the infraorbital artery are still visible. d Superselective angiography of the facial artery. A direct anastomosis between the facial artery (fac) and the dorsal nasal artery (dn) through the angular artery (ang) is easily descernible. The OA (oph) is reached by the contrast medium with a retrograde flow
Less frequently, we observed an anastomosis between the dorsal nasal artery, terminal branch of the OA, and the angular artery, terminal branch of the facial artery (Fig. 4d). Unfortunately, due to the intrinsic purposes of the angiographic examinations which in most cases had not motive to show the anteriormost course of the OA, this type of anastomosis was most frequently beyond the borders of the angiograms or under shielded areas. In spite of such restrictions, this connection was demonstrated in 4 cases (3.77 % of all orbits, 8.9 % in group 2) as in these particular cases it was so well-developed that its hemodynamic importance required a more detailed investigation. In addition, in 3 cases the dorsal nasal artery was also observed as connected with the orbital branch of the infraorbital artery (Fig. 4a–c) (2.83 % of all orbits; 6.66 % in group 2).
A collection of additional rarer anastomoses was also found. In four orbits, the anastomoses involved the frontal branch of the superficial temporal artery; in half cases the anastomosis was completed by the supraorbital artery (Fig. 5a, b), whereas in the other half the frontal branch of the superficial temporal artery was connected with the supratrochlear artery (Fig. 5c). Overall, each type of anastomosis (supraorbital artery—superficial temporal artery and supratrochlear artery—superficial temporal artery) was found in 1.89 % of cases. The rate of recurrence for each type of anastomosis in group 2 was as high as 4.44 % of cases (2 orbits out of 45); overall, the superficial temporal artery was concerned in 8.89 % of cases of group 2 (4 orbits out of 45).
a, b Anastomosis between the superficial temporal artery and the supraorbital artery. c Anastomosis between the superficial temporal artery and the supratrochlear artery. d–f Anastomosis between the zygomaticoorbital artery and the supraorbital artery. a Superselective angiography of the OA. The OA (oph) has a regular branching pattern which includes the supraorbital artery (so). b Superselective angiography of the superficial temporal artery. The superficial temporal artery (st) gives off a descending anastomotic branch (aa) that joins the supraorbital artery (so) (confront with A). c Superselective angiography of the superficial temporal artery. The superficial temporal artery (st) gives off an anastomotic branch (aa) that joins the supratrochlear artery (sut) and injects with a retrograde flow the OA (oph). d Superselective angiography of the OA. The OA (oph) displays a regular pattern of branching which includes the supraorbital artery (so). e Selective angiography of the ECA; early phase. The OA (oph) is injected via an anastomosis with the middle meningeal artery. The supraorbital artery (so) seen in d is also visible. A zygomaticoorbital artery (zo) stems from the superficial temporal artery and ascends to give off a descending anastomotic branch (aa). f Selective angiography of the ECA; later phase. This angiogram demonstrates that the anastomotic branch (aa) of the zygomaticoorbital artery (confront with e) actually joins the supraorbital artery (so)
Two additional cases were anastomoses involving the zygomaticoorbital artery. The overall frequency of detection was 1.89 %; however the frequency of detection in group 2 was 4.44 % (2 orbits out of 45). In one case the anastomotic pathway was completed by the supraorbital artery (Fig. 5d–f), in the other case by the lacrimal artery (Fig. 6).
Anastomosis between the zygomaticoorbital artery and the lacrimal artery. a Superselective angiography of the superficial temporal artery. The zygomaticotemporal artery (zo) stems from the superficial temporal artery via a common trunk with the middle temporal artery and joins the lacrimal artery (lac) via an anastomotic branch (aa). b Superselective angiography of the zygomaticotemporal artery. This angiogram confirms the identity of the lacrimal artery (lac) seen in A as it acts as a conduit through which the contrast medium reaches the ophthalmic artery (oph). An anastomosis between the lacrimal artery and the anterior deep temporal artery (adt) becomes visible with the contrast medium that descends starting from the confluence of the anastomotic vessel (aa) of the zygomaticoorbital artery (zo) with the lacrimal artery
A meningolacrimal artery (a lacrimal artery arising from the middle meningeal artery) was observed in 11 orbits. When present, the meningolacrimal artery was anastomosed with the anterior deep temporal artery in 4 orbits (36.36 % of cases) with the same modalities of a regular lacrimal artery. This anastomosis, however, did not connect the internal and the external carotid systems. On the whole, an anastomosis between the meningolacrimal artery and the anterior deep temporal artery was detected in 3.77 % of all orbits.
Bilateral symmetry of the anastomoses
As in 9 subjects the pathology was bilateral, we had the chance to investigate if the anastomoses showed a symmetric behavior. Unfortunately data from both sides were comparable only in three subjects that were studied bilaterally with the same angiographic approach (superselective angiography of the OA plus selective angiography of the ECA). In the other six cases one side was studied only through the OA and could not be compared reliably with the contralateral orbit. Interestingly, 2 patients out of 3 showed a perfect symmetry: in one case there were anastomoses on both sides between the middle meningeal artery and the lacrimal artery and between the anterior deep temporal artery and the lacrimal artery; in the second patient there were anastomoses on both sides between the middle meningeal artery and the ophthalmic artery and between the anterior deep temporal artery and the meningolacrimal artery.
Discussion
A good knowledge of the vascular anatomy is required in several clinical scenarios. The regular anatomy reported in anatomy textbooks, however, is often not as detailed as it is sometime required. This is the case of the blood supply of the orbit whose description is usually restricted to the branching pattern of the OA and to the minor contributions coming from the infraorbital and facial arteries [20, 24]. The anastomotic pathways joining the OA and the external carotid system frequently go unnoticed and even when they are recalled in more specialized textbooks, their importance is often overlooked [5]. Even reviews on specialized journals are not always thorough in dealing with this significant issue [11]. For the sake of clarity we summarize in Fig. 7 the anastomoses observed in our investigation and that complement the diagrammatic representation drawn by Hayreh [13, 14]. To Hayreh’s diagram, therefore, we should add the direct anastomosis between the middle meningeal artery and the OA (meningoophthalmic artery), the anastomosis between the middle meningeal artery and the supraorbital artery, and the connection between the zygomaticoorbital artery and the supraorbital artery. Whereas the direct anastomosis between the middle meningeal artery and the OA has been previously reported [9, 21], to our knowledge the other two anastomoses are novel entries in the list of connections between the OA and the external carotid system. Due to the lack of infiltration to the globe surface by the retinoblastomas that have been treated (i.e., still restricted within the eyeball), we are of the opinion that the anastomoses were in place before the development of the tumors. Furthermore, with the exception of a couple of cases, all the anastomoses that we showed have been previously reported in healthy adult orbits [14], as to say that they can exist regardless the presence of tumors. However, it is worth to underline that our survey was carried out on angiographies performed in orbits affected by neoplastic lesions and that we cannot rule out completely the possibility that in some cases tumors might have altered the regular hemodynamic.
Schematic diagram summarizing the network of transorbital anastomotic pathways observed in this study. The anastomoses are represented by the double-pointed arrows. The thickness of the arrows is proportional to the number of anastomoses observed in this investigation. The arteries connected by the anastomoses are encircled by lines whose thickness is also proportional to the number of anastomotic pathways involving each given artery
As for their frequency, the anastomoses occurring between the OA and the external carotid system seem to concern almost 1 orbit out of 2, the overall frequency encountered in our study being 44.33 % of orbits. However, the actual frequency is likely much higher. Indeed, at least one anastomotic pathway could be almost always demonstrated in the examinations belonging to group 2 where the superselective angiography of the OA was accompanied by the angiography of the external carotid artery or by the superselective angiography of its branches. In contrast, among the examinations collected in group 1, which gathers angiographic studies carried out exclusively through the OA, anastomoses could be detected only in 6 cases. Thus, whereas the angiography of the OA alone seems quite ineffective in unveiling transorbital anastomotic pathways between the external and the internal carotid systems (6 orbits out of 61, 9.83 % of cases), the combined angiographic approaches (either through the OA or the ECA) seem extremely efficient for their demonstration (41 orbits out of 45; 91.11 % of cases) suggesting that, when properly searched, transorbital anastomoses are indeed almost constant at least in children.
The high rate of recurrence of these anastomoses has practical implications for interventional radiologists when, for instance, they plan embolizations of the external carotid territory [1, 16, 23] or they have to perform intraarterial chemotherapy for intraorbital tumors [1, 19, 27]. In the first case, a careful angiographic study aimed to seek for such anastomoses should be mandatory to avoid unwelcome passage of embolic material into the OA and/or, from there, into the internal carotid territory [2]. In the second case, the regular local hemodynamic of the OA can be altered by the flow coming from the ECA [3, 7, 17]. Consequently, to reach their target, antitumoral drugs may require administration routes alternatives to the OA [3, 7, 17, 27]. Potentially, the many anastomoses that we have shown give an ample variety of chances that goes far beyond the previously reported infusion into the middle meningeal artery [17]. When contrast medium infusion into the OA fails, the possibility to use a distal branch of the external carotid system to inject antitumoral drugs should be carefully explored for the treatment of intraocular retinoblastoma. Actually, sporadic accounts of interventional radiologists exploiting these pathways have been already reported [3, 7]. Similar considerations can be put forward when the target of intraarterial chemotherapy is the lacrimal gland affected by adenoid cystic carcinoma [19, 26]. In this instance, as the lacrimal artery ordinarily stems from the OA, the most obvious route to infuse antitumoral agents should be the OA itself. However, as previously assessed [18, 28], visualization of the lacrimal artery via the OA can be difficult because of its numerous anastomoses with the external carotid system or because it arises from the middle meningeal artery as a meningolacrimal artery [21]. In such cases, the angiographic exploration of the anastomoses occurring between the lacrimal artery and the external carotid system could be essential to establish the best route to deliver the drugs. In this context it is of interest to note that, some way or other, in our survey 42 anastomoses (60 % of cases) concern the lacrimal artery which results connected with the middle meningeal artery in 31.43 % of cases, with the anterior deep temporal artery in 21.42 % of cases and with the zygomaticoorbital artery in one case. Connections with the middle meningeal artery are realized from the proximal segment of the lacrimal artery whereas all other anastomoses are transmalar and join the artery soon before its entering the gland. In a way, therefore, we can certainly affirm that the lacrimal artery occupies a central position among the vessels connecting the external carotid system with the OA.
The development of the orbital and ocular blood supply is quite complex and involves three vessels: the stapedial artery, the primitive dorsal OA and the primitive ventral OA. After anastomosing one another, portions of these arteries regress leaving in place what will be the adult pattern [14]. However, because of the many arteries and anastomoses involved, small derangements from the normal developmental program give rise to course variations of the OA as well as to several branching patterns [14, 15]. Incomplete regression of fetal anastomoses can account for some of the best known anastomotic pathways that are found after birth [9, 21, 29]. Collectively such anastomoses are located at the orbital apex encompassing connections between the lacrimal artery and the middle meningeal artery through the meningeal recurrent branch, and connections between the OA and the middle meningeal artery via the meningoophthalmic artery [9, 21]; in both cases the anastomosis runs through the superior orbital fissure [9]. Anastomotic pathways in this site represent the majority as they account for 54.28 % of all the anastomoses observed in this survey (38 out of 70). However, it is worth to underline that, when looking for anastomotic pathways, attention should be also focused on the anterior orbit. Actually, almost half of all anastomoses (45.71 % of cases) are found in the anterior orbit and they are likely established in a later stage of development as they concern the distal portion of arteries that join one another at the periphery of their territory of distribution. These anastomotic pathways are less frequently acknowledged and involve branches of the OA running forward in the orbit (supraorbital, supratrochlear, dorsal nasal and lacrimal arteries) and connecting some way or other with periorbital arteries (anterior deep temporal artery, angular artery, superficial temporal artery, zygomaticoorbital artery, facial artery) or with the infraorbital artery.
Finally, we have to mention that previously reported minor anastomoses, including connections between the ethmoidal arteries and the sphenopalatine artery [11] or between the palpebral arteries and some periorbital vessels [15], have not been observed in our study. However, our angiographic material is worth to give a picture of the circulation occurring in the orbit of children. It is evident that aging and/or pathological conditions known to alter the regular hemodynamic can promote the enlargement of such anastomoses that should not be overlooked in elder patients.
References
Agid R, Terbrugge K, Rodesch G, Andersson T, Söderman M (2009) Management strategies for anterior cranial fossa (ethmoidal) dural arteriovenous fistulas with an emphasis on endovascular treatment. J Neurosurg 110:79–84
Ahn HS, Kerber CW, Deeb ZL (1980) Extra- to intracranial arterial anastomoses in therapeutic embolization: recognition and role. Am J Neuroradiol 1:71–75
Amans MR, Narvid J, Halbach VV (2014) Intra-arterial chemotherapy for bilateral retinoblastoma via left ophthalmic artery and right anterior deep temporal artery. BMJ Case Reports. doi:10.1136/bcr-2014-204549
Berthelot JL, Hureau J (1982) Clinical anatomy study of the macroscopic anastomoses of the ophthalmic artery in the periorbital region. Clin Anat 3:271–278
Bron AJ, Tripathi RC, Tripathi BJ (2001) The orbital and cerebral vessels. In: Bron AJ, Tripathi RC, Tripathi BJ (eds) Wolff’s anatomy of the eye and orbit, 8th edn. Arnold, London, pp 84–106
Clay CL, Saint-Michel D, Vignaud J, Moret J, Lasjaunias P (1976) Apport de la carotide externe à la vascularisation de l’orbite. Arch Ophtalmol 36:475–490
Cooke D, Farid H, Kim W, Dowd C, Higashida R, Halbach V (2012) Zygomatico-orbital intra-arterial melphalan infusion for intraocular retinoblastoma. J Neurointerv Surg 4:e16
Countee RW, Vijayanathan T (1979) External carotid artery in internal carotid artery occlusion. Angiographic, therapeutic, and prognostic considerations. Stroke 10:450–460
Diamond MK (1991) Homologies of the meningeal-orbital arteries of humans: a reappraisal. J Anat 178:223–241
Ducasse A, Segal A, Delattre JF, Burette A, Flament JB (1985) La participation de l’artère carotid externe à la vascularisation orbitaire. J Fr Ophtalmol 8:333–339
Geibprasert S, Pongpech S, Armstrong D, Krings T (2009) Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventional needs to know. Am J Neuroradiol 30:1459–1468
Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH (2011) Intraarterial chemotherapy for the management of retinoblastoma. Arch Ophthalmol 129:732–737
Hayreh SS (1962) The ophthalmic artery. III. branches. Br J Ophthalmol 46:212–247
Hayreh SS (1963) Arteries of the orbit in the human being. Br J Surg 50:938–953
Hayreh SS (2006) Orbital vascular anatomy. Eye 20:1130–1144
Kendall B, Moseley I (1977) Therapeutic embolisation of the external carotid arterial tree. J Neurol Neurosurg Psychiatry 40:937–950
Klufas MA, Gobin YP, Marr B, Brodie SE, Dunkel IJ, Abramson DH (2012) Intra-arterial chemotherapy as a treatment for intraocular retinoblastoma: alternatives to direct ophthalmic artery catheterization. Am J Neuroradiol 33:1608–1614
Lasjaunias P, Michotey P, Vignaud J, Clay C (1975) II- Radioanatomie de la vascularisation artérielle de l’orbite, a l’exception du tronc de l’artére ophthalmique. Ann Radiol 18:181–194
Meldrum ML, Tse DT, Benedetto P (1998) Neoadjuvant intracarotid chemotherapy for treatment of advance adenoid cystic carcinoma of the lacrimal gland. Arch Ophthalmol 116:315–321
Moore KL, Dalley AF (1999) Clinically oriented anatomy, 4th edn. Lippincott Williams & Wilkins, Baltimore Philadelphia
Moret J, Lasjaunias P, Théron J, Merland JJ (1977) The middle meningeal artery. Its contribution to the vascularization of the orbit. J Neuroradiol 4:225–248
Perrini P, Cardia A, Fraser K, Lanzino G (2007) A microsurgical study of the anatomy and course of the ophthalmic artery and its possibly dangerous anastomoses. J Neurosurg 106:142–150
Smith TP (2006) Embolization in the external carotid artery. J Vasc Interv Radiol 17:1897–1912
Snell RS (1995) Clinical anatomy, 5th edn. Little Brown & Co, Boston
Testut L (1923) Trattato di anatomia umana, 3rd edn. UTET, Turin
Tse DT, Benedetto P, Morcos JJ, Johnson TE, Weed D, Dubovy S (2006) An atypical presentation of adenoid cystic carcinoma of the lacrimal gland. Am J Ophthalmol 141:187–188
Venturi C, Bracco S, Cerase A, Cioni S, Galluzzi P, Gennari P, Vallone IM, Tinturini R, Vittori C, De Francesco S, Caini M, D’Ambrosio A, Toti P, Renieri A, Hadjistilianou T (2013) Superselective ophthalmic artery infusion of melphalan for intraocular retinoblastoma: preliminary results from 140 treatments. Acta Ophthalmol 91:335–342
Vignaud J, Hasso AN, Lasjaunias P, Clay C (1974) Orbital vascular anatomy and embryology. Radiology 111:617–626
Willinsky R, Lasjaunias P, Berenstein A (1987) Intracavernous branches of the internal carotid artery (ICA). Comprehensive review of their variations. Surg Radiol Anat 9:201–215
Acknowledgments
We are indebted to Dr. Irene Grazzini, to Dr. Mauro Caini, to Dr. Rebecca Tinturini of the Azienda Ospedaliera Universitaria Senese for their invaluable help in managing our little patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bracco, S., Venturi, C., Leonini, S. et al. Transorbital anastomotic pathways between the external and internal carotid systems in children affected by intraocular retinoblastoma. Surg Radiol Anat 38, 79–87 (2016). https://doi.org/10.1007/s00276-015-1519-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-015-1519-3